перспективные биомаркеры для диагноза и
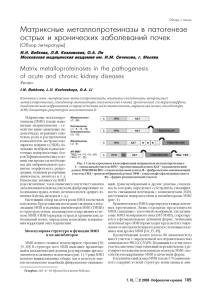
реклама

ОБЗОРЫ Ã. Ñàðäàíà1,2, Á. Äîóýëë3, Ý. Ï. Äèàìàíäèñ1,2,4 ПЕРСПЕКТИВНЫЕ БИОМАРКЕРЫ ДЛЯ ДИАГНОЗА И ПРОГНОЗА РАКА ПРЕДСТАТЕЛЬНОЙ ЖЕЛЕЗЫ (ОБЗОР) q2=2 C!"…= “ !=ƒ!…, `!,*=…“*%L =““%,=,, *,…,#“*%L .,,,. `““%,=, … %2"#=2 ƒ= 2%#…%“2 C!"%=. l……, `““%,=,, , !=*,, ›3!…== %›2 … “%"C==2 “ ……, ="2%!%" C3K,*=,,. o!, ,2,!%"=…,, “2=2 , C!%“ K= ““/=2 “ …= %!,',…= …/L ,“2%#…,* " ›3!…= &Clinical Chemistry[. 4 Emerging Biomarkers for the Diagnosis and Prognosis of Prostate Cancer Girish Sardana1,2, Barry Dowell3, and Eleftherios P. Diamandis1,2,4 1 Department of Laboratory Medicine and Pathobiology, University of Toronto, Toronto, Ontario, Canada, 2 Samuel Lunenfeld Research Institute, Mount Sinai Hospital, Toronto, Ontario, Canada, 3 Abbott Laboratories, Abbott Park, IL; Department of Clinical Biochemistry, University Health Network and Toronto Medical Laboratories, Toronto, Ontario, Canada This article has been translated with the permission of AACC. AACC is not responsible for the accuracy of the translation. The views presented are those of the authors and not necessarily those of AACC or the journal. Reprinted from Clin. Chem. 2008. Vol. 52. P. 1951$1960, by permission of the publisher. Original Copyright I 2008 American Association of Clinical Chemistry, Inc When citing this article, please refer to the original publication source in the journal, Clinical Chemistry. q.*0 9%-(?: ÐÏÆ – ðàê ïðåäñòàòåëüíîé æåëåçû (ïðîñòàòû); ÄÃÏ – äîáðîêà÷åñòâåííàÿ ãèïåðïëàçèÿ ïðîñòàòû; fPSA– ñâîáîäíûé ñïåöèôè÷åñêèé äëÿ ïðîñòàòû àíòèãåí; KLK2 – ðîäñòâåííàÿ êàëëèêðåèíó ïåïòèäàçà 2; PSMA – ñïåöèôè÷åñêèé äëÿ ïðîñòàòû ìåìáðàííûé àíòèãåí; PCA3 – àíòèãåí ðàêà ïðîñòàòû; EPCA – ðàííèé àíòèãåí ðàêà ïðîñòàòû; AMACR – α-ìåòèë-ÊîÀ-ðàöåìàçà; uPA – àêòèâàòîð óðîêèíàçû è ïëàçìèíîãåíà, uPAR – ðåöåïòîð uPa; IGF – èíñóëèíîïîäîáíûé ðîñòîâûé ôàêòîð; IGFBP – áåëîê ñâÿçûâàíèÿ IGF; TGF – òðàíñôîðìèðóþùèé ðîñòîâûé ôàêòîð; PSP94 – ñåêðåòîðíûé áåëîê-94 ïðîñòàòû; CRISP-3 – áîãàòûé öèñòåèíîì ñåêðåòîðíûé áåëîê-3; ANXA3 – àííåêñèí À3; PSCA – àíòèãåí ñòâîëîâûõ êëåòîê ïðîñòàòû; IL-6 – èíòåðëåéêèí 6 Ðàê ïðåäñòàòåëüíîé æåëåçû (ÐÏÆ) ÿâëÿåòñÿ ñà- øèì èç áèîìàðêåðîâ, èçâåñòíûõ â îíêîëîãèè, íî ïðè ìûì ðàñïðîñòðàíåííûì ðàêîâûì çàáîëåâàíèåì ó ýòîì èìååò ìíîæåñòâî íåäîñòàòêîâ. Èñõîäíî PSA ìóæ÷èí è âòîðîé ïî çíà÷èìîñòè ïðè÷èíîé ñìåðòè â èñïîëüçîâàëè äëÿ ìîíèòîðèíãà áîëüíûõ ÐÏÆ, è Ñåâåðíîé Àìåðèêå. Êàæäûé øåñòîé ìóæ÷èíà íàõî- òîëüêî ïîçæå åãî ïðèìåíåíèå áûëî ðàñïðîñòðàíåíî äèòñÿ â ãðóïïå ðèñêà ïî ÐÏÆ íà ïðîòÿæåíèè æèçíè, íà ñêðèíèíã. Îòêðûòèå PSA è åãî âíåäðåíèå â êëèíèà âåðîÿòíîñòü ñìåðòè îò ýòîãî çàáîëåâàíèÿ ñîñòàâëÿ- êó â íà÷àëå 1990-õ ãã. XX â. îêàçàëî îãðîìíîå âëèÿåò 3,4 %.  íàñòîÿùåå âðåìÿ äèàãíîç â áîëüøèíñòâå íèå íà ðàííþþ äèàãíîñòèêó ÐÏÆ è ñòàëî ïðè÷èíîé ñëó÷àåâ ñòàâèòñÿ ó áîëüíûõ íà ðàííåé áåññèìïòîìíîé óâåëè÷åíèÿ äîêóìåíòèðîâàííîé çàáîëåâàåìîñòè ÐÏÆ. ñòàäèè çàáîëåâàíèÿ. Âñëåäñòâèå òàêîãî äèàãíîñòè÷å-  íàñòîÿùåå âðåìÿ PSA èñïîëüçóþò êàê äèàãíîñòèñêîãî ñäâèãà êëàññè÷åñêèå ïîäõîäû ê ïðîãíîçó, òàêèå ÷åñêèé ìàðêåð, íî åãî óðîâíè âñå áîëüøå ïðèçíàþòêàê òàáëèöû Ïàðòýíà (Partin) è íîìîãðàììû Êàòòàíà ñÿ îòðàæàþùèìè ðèñê ÐÏÆ. Âåðõíèé ïðåäåë íîðìû (Kattan), óæå íå ñòîëü ýôôåêòèâíû, êàê â ïðîøëîì. óñòàíîâëåí íà óðîâíå 4 ìêã/ë, ÷òî íå ïîçâîëÿåò âûÿâÂíèìàíèå ñåé÷àñ ñìåñòèëîñü îò ðàííåãî âûÿâëåíèÿ ëÿòü ìíîãèå ñëó÷àè ðàêà, è â ïðîåêòå «Èñïûòàíèå ïðîê îïðåäåëåíèþ êëèíè÷åñêîãî çíà÷åíèÿ îïóõîëåé íà ôèëàêòèêè ðàêà ïðîñòàòû» áûë ñäåëàí âûâîä î òîì, ðàííåé ñòàäèè. Îäíà èç çàäà÷ ïðè ýòîì ñîñòîèò â îòûñ- ÷òî íèêàêàÿ êîíöåíòðàöèÿ PSA íå èñêëþ÷àåò íàëè÷èÿ êàíèè ïóòåé âûÿâëåíèÿ êëèíè÷åñêè çíà÷èìûõ îïóõî- ðàêà. Îïðåäåëåíèå îáùåãî PSA îêàçàëîñü ïîëåçíûì ëåé, ñïîñîáíûõ ê ìåòàñòàçèðîâàíèþ.  íàñòîÿùåå ïðîãíîñòè÷åñêèì ñðåäñòâîì, ïðè÷åì âûñîêèå äîîïåâðåìÿ 30 % îïóõîëåé, óäàëÿåìûõ ïðè ðàäèêàëüíîé ðàöèîííûå óðîâíè ñâÿçàíû ñ äàëåêî çàøåäøèì çàáîïðîñòàòýêòîìèè, ïðèçíàþòñÿ êëèíè÷åñêè íåçíà÷èìû- ëåâàíèåì è ïëîõèì ïðîãíîçîì. Ïðîòèâîðå÷èÿ âîêðóã ìè è íå òðåáóþùèìè âìåøàòåëüñòâà òàêîãî îáúåìà. PSA ñåé÷àñ àêòèâíî îáñóæäàþòñÿ, ïîñêîëüêó íåÿñíî,  áîëüøèíñòâå ñëó÷àåâ âûÿâëÿåòñÿ ëàòåíòíûé íå- ïðèâåë ëè ñêðèíèíã íà PSA ê ñíèæåíèþ ñìåðòíîñòè àãðåññèâíûé ÐÏÆ, ïîýòîìó âàæíî íå ïîäâåðãàòü ýòèõ îò ÐÏÆ. Îòâåò íà âîïðîñ, ñíèæàåò ëè ñêðèíèíã íà áîëüíûõ ðàäèêàëüíîìó ëå÷åíèþ. Ñäåðæèâàíèå ÐÏÆ PSA ñìåðòíîñòü, äîëæåí áûòü ïîëó÷åí ïî ðåçóëüòàòàì âîçìîæíî ïðè ðàííåé äèàãíîñòèêå è äîëæíîì ëå÷å- ïðîâåäåííûõ â 2008–2009 ãã. äâóõ êðóïíûõ ðàíäîìèíèè, îäíàêî ñîîòâåòñòâóþùèé óðîâåíü äèàãíîñòè÷å- çèðîâàííûõ ïðîñïåêòèâíûõ êëèíè÷åñêèõ èññëåäîâàñêîé èçîùðåííîñòè ïîêà åùå íå äîñòèãíóò. íèé «Åâðîïåéñêîå ðàíäîìèçèðîâàííîå èññëåäîâàíèå Áèîìàðêåðîì, èñïîëüçóåìûì â íàñòîÿùåå âðåìÿ ñêðèíèíãà íà ðàê ïðîñòàòû» è «Èçó÷åíèå ñêðèíèíãà äëÿ ðàííåé äèàãíîñòèêè ÐÏÆ, ÿâëÿåòñÿ ñïåöèôè÷å- íà ðàê ïðîñòàòû, ëåãêèõ, ïðÿìîé è îáîäî÷íîé êèøêè ñêèé äëÿ ïðîñòàòû àíòèãåí (PSA). Îí ñ÷èòàåòñÿ ëó÷- è ÿè÷íèêîâ». Ñîîòíîøåíèå ìåæäó PSA è ñòàäèåé îïó- ПОДПИСНОЙ ИНДЕКС 72075 3 ОБЗОРЫ õîëè òàêæå íåÿñíî. Óðîâåíü PSA â òêàíè ñíèæàåòñÿ ïî ñûâîðîòêå ñëåäóåò, ÷òî äèàãíîç ÐÏÆ óëó÷øàåòñÿ ñ óâåëè÷åíèåì êîýôôèöèåíòà Ãëèñîíà, íî êîíöåíòðà- ïðè èñïîëüçîâàíèè KLR2 â ñî÷åòàíèè ñ îáùèì PSA öèè PSA â ñûâîðîòêå ïðè ýòîì ðàñòóò èç-çà ðàçðûâîâ è fPSA, îñîáåííî â òîì, ÷òî êàñàåòñÿ ýêñòðàêàïñóáàçàëüíîé ìåìáðàíû âîêðóã ýïèòåëèàëüíûõ êëåòîê ëÿðíîãî ðàñïðîñòðàíåíèÿ è îáúåìà îïóõîëè. Òàêæå ïðîñòàòû è íàðóøåíèÿ îáùåãî ñòðîåíèÿ òêàíè ïðîñòà- KLK2, ïðè ñðàâíåíèè ñ PSA, äàåò âàæíóþ íåçàâèñèòû. PSA íåñïåöèôè÷åí â îòíîøåíèè ÐÏÆ è ìîæåò ñëó- ìóþ ïðîãíîñòè÷åñêóþ èíôîðìàöèþ î ðèñêå ðåöèäèæèòü ìàðêåðîì äîáðîêà÷åñòâåííîé ãèïåðïëàçèè ïðåä- âîâ ÐÏÆ ïðè óðîâíå PSA < –10 ìêã/ë. Äëÿ âûÿñíåíèÿ ñòàòåëüíîé æåëåçû (ÄÃÏÆ) è óâåëè÷åíèÿ åå îáúåìà. ïðîãíîñòè÷åñêîãî ïîòåíöèàëà KLK2 íåîáõîäèìà äîÎäíàêî êëþ÷åâûå ñòàòèñòè÷åñêèå îöåíêè åãî àäåêâàò- ïîëíèòåëüíàÿ àïðîáàöèÿ ýòîãî ìàðêåðà. íîñòè îêàçàëèñü íåïîêàçàòåëüíûìè: ïðè ïîçèòèâíûõ ïðåäñêàçàòåëüíûõ âåëè÷èíàõ, ïîëó÷àåìûõ â 37 % ñëóСпецифический для предстательной ÷àåâ, äëÿ áîëüíûõ â «ñåðîé» çîíå 4–10 ìêã/ë âåжелезы мембранный антиген ðîÿòíîñòü ñêðûòîãî ÐÏÆ ñîñòàâëÿåò 25 %, è ÐÏÆ Ñïåöèôè÷åñêèé äëÿ ïðîñòàòû ìåìáðàííûé àíòèâûÿâëÿåòñÿ ó 15% áîëüíûõ ñ êîíöåíòðàöèåé PSA <4 ìêã/ë. Íåàäåêâàòíîñòü PSA â êà÷åñòâå ìàðêåðà ãåí (prostate-specific membrane antigen, PSMA) ÿââûçâàëà íåîáõîäèìîñòü â íîâûõ ìàðêåðàõ ÐÏÆ äëÿ ëÿåòñÿ ìåìáðàííûì ãëèêîïðîòåèíîì, êîòîðûé îáïðåäîòâðàùåíèÿ ÷ðåçìåðíûõ òåðàïåâòè÷åñêèõ ìåð ðàçóåòñÿ â âûñîêèõ êîíöåíòðàöèÿõ â ýïèòåëèàëüíûõ â îòíîøåíèè âÿëîòåêóùåãî çàáîëåâàíèÿ. Âäîáàâîê êëåòêàõ çäîðîâûõ ëèö è áîëüíûõ ÐÏÆ. Îêàçàëîñü, ê äèàãíîñòè÷åñêèì ìàðêåðàì, íóæíû ïðîãíîñòè÷å- ÷òî îòíîñèòåëüíàÿ ïðîäóêöèÿ PSMA ïîâûøåíà â ýïèñêèå, ïðåäñêàçàòåëüíûå è òåðàïåâòè÷åñêèå ìàðêåðû òåëèàëüíûõ êëåòêàõ òêàíè ÐÏÆ. Ôèðìà «Cytogen» â êà÷åñòâå ñóððîãàòíûõ êîíå÷íûõ ïîêàçàòåëåé äëÿ ðàçðàáîòàëà êîììåð÷åñêèé òåñò äëÿ âèçóàëèçàöèè ïðåäñêàçàíèÿ òÿæåñòè çàáîëåâàíèÿ, âûáîðà ëå÷åíèÿ PSMA (ProstaScint) ðàäèîèììóíîñöèíòèãðàôèåé. Íàè ìîíèòîðèíãà îòâåòà íà òåðàïèþ, ñîîòâåòñòâåííî. êîíåö, PSMA èññëåäîâàí â êà÷åñòâå òåðàïåâòè÷åñêîé  ýòîì îáçîðå îñíîâíîå âíèìàíèå áóäåò íàïðàâëåíî ìèøåíè àíòèòåë, êîíúþãèðîâàííûõ ñ ðàäèîèçîòîíà íîâûå ìàðêåðû, êîòîðûå âûãëÿäÿò ïåðñïåêòèâíûìè ïàìè èëè îêñèíàìè, èëè àêòèâèðîâàííûìè äåíäðèòäëÿ ðàííåãî âûÿâëåíèÿ è ëå÷åíèÿ ÐÏÆ (2=K. 1). íûìè êëåòêàìè ïðîòèâ PSMA. Èñïîëüçîâàíèå PSMA åùå íå ñòàëî ïðèíÿòûì â êëèíè÷åñêîé ïðàêòèêå, Производные от уровня PSA è åãî âîçìîæíîñòè äëÿ äèàãíîñòèêè è òåðàïèè âñå Ñòàëî ÿñíî, ÷òî ðàáî÷èå õàðàêòåðèñòèêè PSA òðå- åùå íàõîäÿòñÿ â ðàçðàáîòêå. áóþò óëó÷øåíèÿ. Îäèí èç ïîäõîäîâ äëÿ äîñòèæåíèÿ ýòîé öåëè ñîñòîèò â îïðåäåëåíèè ïðîèçâîäíûõ îò Другие тканевые калликреины óðîâíåé PSA, â òîì ÷èñëå ñêîðîñòè èçìåíåíèÿ PSA Äî íåäàâíåãî âðåìåíè òîëüêî KLK3 (ðîäñòâåíñî âðåìåíåì, ñîîòíîøåíèÿ êîíöåíòðàöèè è îáúåìà íàÿ êàëëèêðåèíó ïåïòèäàçà-3, ïðè÷åì èìåííî îíà ïðîñòàòû («ïëîòíîñòü» PSA) è èíòåðâàëîâ óðîâíåé ïðåæäå áûëà èçâåñòíà êàê PSA), KLK2 (ðîäñòâåíPSA, ñïåöèôè÷íûõ äëÿ ðàçíûõ âîçðàñòíûõ ãðóïï. íàÿ êàëëèêðåèíó ïåïòèäàçà-2) è KLK1 (êàëëèêðåèí-1, Âäîáàâîê, óñïåõè â îïðåäåëåíèè PSA è ðîäñòâåííûõ òàêæå èçâåñòíûé êàê ïàíêðåàòè÷åñêèé/ïî÷å÷íûé åìó áåëêîâ ñäåëàëè âîçìîæíûì îïðåäåëåíèå äîëè êàëëèêðåèí) áûëè ãåíàìè, èäåíòèôèöèðîâàííûìè ñâîáîäíîãî PSA (fPSA), ïðåäñòàâëÿþùåãî ñîáîé â êàëëèêðåèíîâîì ëîêóñå íà õðîìîñîìå 19. Èçñîîòíîøåíèå ñâîáîäíîãî è îáùåãî PSA.  ÷àñòíîâåñòíî, ÷òî ýòîò ëîêóñ ïðîñòèðàåòñÿ íà 300 òûñ. ñòè, áûëî ïðîäåìîíñòðèðîâàíî çíà÷åíèå äîëè fPSA ïàð íóêëåîòèäîâ è ñîñòîèò èç 15 ãåíîâ, èìåþùèõ â êà÷åñòâå ïðåäñêàçàòåëüíîãî ïðèçíàêà ïîçäíèõ çíà÷èòåëüíóþ ãîìîëîãèþ è ñõîäñòâî íóêëåîòèäíûõ ñòàäèé ÐÏÆ. Äðóãèå âàðèàíòû âêëþ÷àþò îïðåäåëå- è àìèíîêèñëîòíûõ ïîñëåäîâàòåëüíîñòåé. Âäîáàâîê íèå êîìïëåêñîâ PSA ñ α2-ìàêðîãëîáóëèíîì, α1-àíòè- ê KLK2, äðóãèå êàëëèêðåèíû îêàçàëèñü ïîëåçíûìè õèìîòðèïñèíîì, à òàêæå ðàçíûõ ïðîäóêòîâ ðàñùå- â êà÷åñòâå áèîìàðêåðîâ ÐÏÆ è äðóãèõ çàáîëåâàíèé. ïëåíèÿ PSA, òàêèõ êàê [-2]proPSA è bPSA. Âîñåìü êàëëèêðåèíîâ îáðàçóþòñÿ â îòíîñèòåëüíî âûñîêèõ êîíöåíòðàöèÿõ â òêàíÿõ ïðîñòàòû: KLK 2-4, 10-13 è 15. Èç èõ ÷èñëà KLK11 â ñî÷åòàíèè ñ PSA Человеческая родственная è äîëåé fPSA ïðîäåìîíñòðèðîâàë ñïîñîáíîñòü íåкалликреину пептидаза-2 ñêîëüêî óëó÷øàòü ïðåäñêàçóåìîñòü ÐÏÆ. ×åëîâå÷åñêàÿ ðîäñòâåííàÿ êàëëèêðåèíó ïåïòèäàçà-2 (KLK2, ïðåæäå èçâåñòíàÿ êàê hK2) ÿâëÿåòñÿ Антиген рака предстательной железы 3 ñåêðåòèðóåìîé ñåðèíîâîé ïðîòåèíàçîé, ãåí êîòîÀíòèãåí ðàêà ïðîñòàòû 3 (PCA3), òàêæå èçâåñòðîé îòíîñèòñÿ ê òîìó æå ñåìåéñòâó, ÷òî è ãåí PSA. Èç äàííûõ ïî òêàíÿì ÐÏÆ ñëåäóåò, ÷òî KLK2 ïîâû- íûé êàê DD3, ÿâëÿåòñÿ íåêîäèðóþùåé ÐÍÊ, îáðàøàåòñÿ ïî ìåðå åãî ïðîãðåññèðîâàíèÿ è ïîýòîìó ìî- çóþùåéñÿ èñêëþ÷èòåëüíî â ïðîñòàòå. Ñèëüíî ïîâûæåò ñëóæèòü â êà÷åñòâå áèîìàðêåðà ÐÏÆ. Èç äàííûõ øåííûå óðîâíè PCA3 ïðèñóòñòâóþò â òêàíÿõ ÐÏÆ, 4 WWW.TERRAMEDIСA.SPB.RU ОБЗОРЫ Таблица 1 Список кандидатов в биомаркеры рака предстательной железы и их возможное клиническое применение Êàíäèäàò â áèîìàðêåðû Ïðîâåðåííàÿ êëèíè÷åñêàÿ ïðèìåíèìîñòü KLK2 Äèàãíîñòè÷åñêîå è ïðîãíîñòè÷åñêîå ïðåäñêàçàíèå ýêñòðàêàïñóëÿðíîãî ðàñïðîñòðàíåíèÿ îïóõîëè, îáúåìà îïóõîëè è ðåöèäèâîâ ïî áèîõèìè÷åñêèì ïðèçíàêàì PSMA Âèçóàëèçàöèÿ, òåðàïåâòè÷åñêàÿ ìèøåíü KLK11 Ðàííèé ñûâîðîòî÷íûé ïðåäñêàçàòåëüíûé ïðèçíàê ÐÏÆ PCA3 Áèîìàðêåð ÐÏÆ, îïðåäåëÿåìûé â ìî÷å EPCA/EPCA-2 Èììóíîãèñòîõèìè÷åñêîå âûÿâëåíèå ÐÏÆ, ñûâîðîòî÷íûé ìàðêåð äëÿ äèôôåðåíöèàöèè ëîêàëüíîãî è ìåòàñòàòè÷åñêîãî ÐÏÆ AMACR Âûÿâëåíèå ÐÏÆ ïî àóòîàíòèòåëàì, èììóíîãèñòîõèìè÷åñêîå âûÿâëåíèå, ïðîãíîñòè÷åñêèé ïðèçíàê ñìåðòíîñòè è ðåöèäèâîâ ïî áèîõèìè÷åñêèì ïðèçíàêàì uPA/uPAR Ïîâûøåííûå êîíöåíòðàöèè â òêàíÿõ è ñûâîðîòêå ïðåäñêàçûâàþò áèîõèìè÷åñêèå ðåöèäèâû è ìåòàñòàçû IGF/IGFBP IGF-1 ñëåãêà ïîâûøåí â ñûâîðîòêå ïðè ÐÏÆ, êîíöåíòðàöèè IGFBP íàõîäÿòñÿ â îáðàòíîé êîððåëÿöèè ñ ïðîãðåññèåé ÐÏÆ TMPRSS2:ERG/ ETV1 TGFβ- 1 EZY2 GSTP1 PSP94 CRISP-3 Õðîìîãðàíèí ` Ïåïòèäíûé ôàêòîð âûñâîáîæäåíèÿ ïðîãàñòðèíà e-êàäõåðèí Àííåêñèí `3 PSCA Ãåïñèí Èíòåðëåéêèí 6 ПОДПИСНОЙ ИНДЕКС 72075 Âûÿâëÿþòñÿ íà ïîâûøåííûõ óðîâíÿõ â ìî÷å ó áîëüíûõ ÐÏÆ è èíòðàýïèòåëèàëüíîé íåîïëàçèåé in situ, ñëèÿíèå ãåíîâ âûÿâëÿåòñÿ â òêàíÿõ ÐÏÆ ôëþîðåñöåíòíîé ãèáðèäèçàöèåé in situ Ïîâûøåíèå èììóíîãèñòîõèìè÷åñêîãî îêðàøèâàíèÿ è óðîâíÿ â ñûâîðîòêå êðîâè ïî ìåðå ïðîãðåññèè ÐÏÆ è ðåöèäèâîâ ïî áèîõèìè÷åñêèì ïðèçíàêàì Ýêñïðåññèÿ ãåíà â òêàíÿõ ÐÏÆ ÿâëÿåòñÿ ïðåäñêàçàòåëüíûì ïðèçíàêîì ïðîãðåññèè Âûÿâëåíèå ãèïåðìåòèëèðîâàíèÿ ïðîìîòîðà ýòîãî ãåíà äëÿ îöåíêè öåëåñîîáðàçíîñòè áèîïñèè Ïðåäñêàçàòåëüíûé ïðèçíàê èíäåêñà Ãëèñîíà è ðåöèäèâîâ ïî áèîõèìè÷åñêèì ïðèçíàêàì ïîñëå ëîêàëüíîé îïåðàöèè Ïîâûøåííàÿ ãèñòîõèìè÷åñêàÿ îêðàøèâàåìîñòü òêàíè ïðîñòàòû ó ìóæ÷èí ñ ñèëüíî òðàíñôîðìèðîâàííîé èíòðàýïèòåëèàëüíîé íåîïëàçèåé, íåçàâèñèìûé ïðåäñêàçàòåëüíûé ïðèçíàê ðåöèäèâîâ ÐÏÆ Ìîíèòîðèíã áîëüíûõ ñ íåçàâèñèìûì îò àíäðîãåíîâ ÐÏÆ ñ íåéðîýíäîêðèííîé äèôôåðåíöèàöèåé íà ïîçäíèõ ñòàäèÿõ Ìîíèòîðèíã áîëüíûõ ñ ìåòàñòàòè÷åñêèì ÐÏÆ, èìåþùèì íåéðîýíäîêðèííûå è íåçàâèñèìûå îò àíäðîãåíîâ ôåíîòèïû Ñíèæåííàÿ èììóíîãèñòîõèìè÷åñêàÿ ýêñïðåññèÿ ïðè ÐÏÆ êîððåëèðóåò ñî ñòàäèåé ñíèæåííîé âûæèâàåìîñòè Ñíèæåííîå îáðàçîâàíèå â òêàíÿõ ÐÏÆ ïî ðåçóëüòàòàì èììóíîãèñòîõèìèè, ïðîãíîñòè÷åñêèé ïðèçíàê ðèñêà Èììóíîãèñòîõèìè÷åñêèé ìàðêåð, êîððåëèðóþùèé ñ èíäåêñîì Ãëèñîíà è ñòàäèåé, òåðàïåâòè÷åñêàÿ ìèøåíü Èììóíîãèñòîõèìè÷åñêîå âûÿâëåíèå èíòðàýïèòåëèàëüíîé íåîïëàçèè è ÐÏÆ â îòëè÷èå îò ÄÃÏÆ Ïîâûøåííûå êîíöåíòðàöèè â ñûâîðîòêå íà ïîçäíèõ ñòàäèÿõ ÐÏÆ 5 ОБЗОРЫ â òîì ÷èñëå â ìåòàñòàçàõ, ïðè ñðàâíåíèè ñ òêàíÿìè ÄÃÏÆ. Ñóùåñòâóåò íåñêîëüêî ñïîñîáîâ îïðåäåëåíèÿ PCA3 â ìî÷å. Åäèíñòâåííûì èìåþùèìñÿ â ïðîäàæå òåñòîì ÿâëÿåòñÿ APTIMA® (Gene-Probe), îñíîâàííûé íà ÏÖÐ. Ðåçóëüòàòû îïðåäåëåíèÿ PCA3 íîðìàëèçóþò îòíîñèòåëüíî êîíöåíòðàöèè PSA.  íåäàâíåì èññëåäîâàíèè ñ ó÷àñòèåì íåñêîëüêèõ ó÷ðåæäåíèé íà ïàöèåíòàõ, ïîäâåðãàåìûõ áèîïñèè, êîòîðîå âêëþ÷àëî àíàëèç PCA3 â ìî÷å ïîñëå ìàññàæà ïðîñòàòû, óðîâíåì îòñå÷åíèÿ áûëî îòíîøåíèå 58, ïðè ýòîì ïëîùàäü ïîä êðèâîé ñîîòíîøåíèÿ èñòèííîïîëîæèòåëüíûõ è ëîæíîïîëîæèòåëüíûõ ðåçóëüòàòîâ (receiver operating characteristic curve, ROC curve) áûëà 0,66 ïðîòèâ 0,57 äëÿ PSA.  èññëåäîâàíèè 223 áîëüíûõ, ïîäâåðãíóòûõ ïîâòîðíûì áèîïñèÿì ïîñëå ïîëó÷åíèÿ îòðèöàòåëüíîãî ðåçóëüòàòà áèîïñèè, äëÿ PCA3 áûëà îïðåäåëåíà ïëîùàäü ïîä êðèâîé ROC 0,68, à äèàãíîñòè÷åñêàÿ ÷óâñòâèòåëüíîñòü è ñïåöèôè÷íîñòü îïðåäåëåíû êàê 58 è 72%, ñîîòâåòñòâåííî. Ýòîò òåñò ìîæåò îêàçàòüñÿ ïîëåçíûì â óëó÷øåíèè äèàãíîñòè÷åñêîé ñïåöèôè÷íîñòè PSA. Ñî÷åòàíèå PCA3 åùå ñ òðåìÿ áèîìàðêåðàìè â ìî÷å (GPLDPH2, SPINK1 è ïðîäóêò ñëèòíîãî ãåíà TMPRSS2:EGR ) óëó÷øàåò äèàãíîñòè÷åñêóþ ñïåöèôè÷íîñòü è ÷óâñòâèòåëüíîñòü â ñðàâíåíèè òîëüêî ñ PCA3. Ранние антигены РПЖ Ñ êàíöåðîãåíåçîì ñâÿçàíû èçìåíåíèÿ â áåëêàõ ÿäåðíîãî ìàòðèêñà. Ðàííèé àíòèãåí ðàêà ïðîñòàòû (EPCA) ÿâëÿåòñÿ áåëêîì ÿäåðíîãî ìàòðèêñà, êîòîðûé èñõîäíî áûë âûÿâëåí ïðè ïîñòðîåíèè ïðîòåîìíîãî ïðîôèëÿ òêàíè ïðîñòàòû êðûñû. Ïîçæå îí îêàçàëñÿ ïåðñïåêòèâíûì â ïëàíå äèàãíîñòè÷åñêîãî ìàðêåðà ÐÏÆ. Èììóíîãèñòîõèìè÷åñêèå èññëåäîâàíèÿ áèîïñèé òêàíè ÐÏÆ ïðè èñïîëüçîâàíèè àóòîàíòèòåë ê EPCA ïîêàçàëè ïîâûøåíèå îêðàøèâàåìîñòè îòíîñèòåëüíî íåïîðàæåííûõ ó÷àñòêîâ. Òàêîé ýôôåêò íàáëþäàëñÿ è â íåïîðàæåííûõ ó÷àñòêàõ, ïðèëåãàþùèõ ê îïóõîëåâîé òêàíè, è â 86% ïðîá òêàíè ÐÏÆ. EPCA ïîìîãàåò â èäåíòèôèêàöèè áîëüíûõ ñ ðèñêîì ÐÏÆ ïðè îòðèöàòåëüíûõ ðåçóëüòàòàõ áèîïñèè. Íåäàâíî ðàçðàáîòàííûé àíàëèç êðîâè íà EPCA ïðîäåìîíñòðèðîâàë äèàãíîñòè÷åñêóþ ÷óâñòâèòåëüíîñòü 92% è òî÷íîñòü 94% â íåáîëüøîé êîãîðòå èç 12 áîëüíûõ ÐÏÆ è 34 çäîðîâûõ ëèö.  äðóãîì èññëåäîâàíèè, ãäå áåëîê EPCA-2 îïðåäåëÿëñÿ â ñûâîðîòêå, ÷óâñòâèòåëüíîñòü è ñïåöèôè÷íîñòü ïî âûÿâëåíèþ ÐÏÆ îïðåäåëåíû â 92 è 94%, ñîîòâåòñòâåííî, ïðè÷åì EPCA-2 îêàçàëñÿ ñïîñîáíûì äèôôåðåíöèðîâàòü ëîêàëèçîâàííûé è ìåòàñòàòè÷åñêèé ÐÏÆ, â êàêîâîì ñëó÷àå ïëîùàäü ïîä êðèâîé ROC îïðåäåëåíà êàê 0,89. Ýòè ìíîãîîáåùàþùèå ðåçóëüòàòû íàäî ïîäòâåðäèòü áîëåå êðóïíûìè íåçàâèñèìûìè èññëåäîâàíèÿìè, îäíàêî âûÿâëåíû è äèàãíîñòè÷åñêèå íåäîñòàòêè ýòèõ ìàðêåðîâ, çàñòàâëÿþùèå ñîìíåâàòüñÿ â èõ öåííîñòè. 6 α-Метилацил-КоА-рацемаза α-Ìåòèëàöèë-ÊîÀ-ðàöåìàçà (AMACR ) ÿâëÿåòñÿ ôåðìåíòîì, ó÷àñòâóþùèì â îêèñëèòåëüíîì ìåòàáîëèçìå è ñèíòåçå æèðíûõ êèñëîò ñ ðàçâåòâëåííîé öåïüþ, êîòîðûå îáíàðóæèâàþòñÿ â ìîëî÷íûõ ïðîäóêòàõ è ìÿñå. Êðîìå òîãî, ÷òî ýòîò ôåðìåíò îáðàçóåòñÿ â áîëüøèõ êîëè÷åñòâàõ â òêàíè ÐÏÆ, îí åùå è êîäèðóåòñÿ ãåíîì, êîòîðûé ëîêàëèçîâàí â îáëàñòè 5p13.3, êîòîðàÿ ñîäåðæèò ïîëèìîðôèçìû, ñâÿçàííûå ñ ÐÏÆ. Ìåòààíàëèç äàííûõ ïî îäíîâðåìåííîìó îïðåäåëåíèþ ýêñïðåññèè áîëüøîãî ÷èñëà ãåíîâ îïðåäåëåííî ïîêàçàë, ÷òî ýêñïðåññèÿ AMACR ïîâûøåíà â ÐÏÆ. Ñîâìåñòíî ïðîâåäåííîå â íåñêîëüêèõ ó÷ðåæäåíèÿõ èññëåäîâàíèå ïîêàçàëî, ÷òî èììóíîãèñòîõèìè÷åñêîå îêðàøèâàíèå íà AMAP ìîæåò ïîìîãàòü â ðàçëè÷åíèè ìåæäó çëîêà÷åñòâåííîé è äîáðîêà÷åñòâåííîé òêàíÿìè ðàêà ïðîñòàòû ñ äèàãíîñòè÷åñêîé ÷óâñòâèòåëüíîñòüþ 97% è ñïåöèôè÷íîñòüþ 92%. Ñíèæåííàÿ ïðîäóêöèÿ AMACR èìååò ïðîãíîñòè÷åñêóþ öåííîñòü äëÿ ïðåäñêàçàíèÿ áèîõèìè÷åñêèõ ðåöèäèâîâ ÐÏÆ è ñìåðòè îò ïîñëåäíåãî. Êîíöåíòðàöèè ìÐÍÊ è AMACR â ñûâîðîòêå êðîâè è ìî÷å îïðåäåëÿþò îáðàòíîòðàíñêðèïòàçíîé ÏÖÐ. Êîíöåíòðàöèÿ áåëêà AMACR â ñûâîðîòêå íèçêàÿ, íî îí áûë âûÿâëåí â ìî÷å Âåñòåðíáëîòòèíãîì. Ïîâûøåííûå êîíöåíòðàöèè àóòîàíòèòåë ê AMACR ïîìîãàþò â ðàçëè÷åíèè áîëüíûõ ÐÏÆ è çäîðîâûõ ëèö â èíòåðâàëå PSA 4–10 ìêã/ë. Ó ýòîãî òåñòà äèàãíîñòè÷åñêàÿ ÷óâñòâèòåëüíîñòü îêàçàëàñü 62%, à ñïåöèôè÷íîñòü 72%. Äëÿ ïîëíîãî âûÿñíåíèÿ ïîòåíöèàëà AMACR â êà÷åñòâå áèîìàðêåðà ÐÏÆ ïðîâîäÿòñÿ äîïîëíèòåëüíûå èññëåäîâàíèÿ. Активатор и рецептор урокиназы и плазминогена Ñ ïðîãðåññèåé ðàêà ñâÿçàíà äåãðàäàöèÿ âíåêëåòî÷íîãî ìàòðèêñà, â ýòîì ïðîöåññå ïðèíèìàåò ó÷àñòèå êàñêàä ðåàêöèé, âêëþ÷àþùèé àêòèâàöèþ óðîêèíàçû è ïëàçìèíîãåíà. Ïëàçìèíîãåí ïðåâðàùàåòñÿ â àêòèâíóþ ôîðìó ïëàçìèíà ÷åðåç àêòèâàöèþ ñåðèíîâîé ïðîòåèíàçû, èçâåñòíîé êàê àêòèâàòîð óðîêèíàçû è ïëàçìèíîãåí (uPA), è åå ñâÿçûâàíèå ñ ðåöåïòîðîì (uPAR ). Ïðîäåìîíñòðèðîâàíî ïîâûøåíèå êîíöåíòðàöèè uPA ó áîëüíûõ ÐÏÆ è ÄÃÏÆ â ñðàâíåíèè ñî çäîðîâûìè ëèöàìè, õîòÿ ñòàòèñòè÷åñêè äîñòîâåðíàÿ ñâÿçü ñ ÐÏÆ îòñóòñòâîâàëà. Êîìáèíàöèè âûÿâëåíèÿ èçîôîðì uPAR ñ âûÿâëåíèåì KLK2 è èçîôîðì PSA óëó÷øèëè, ïî ðåçóëüòàòàì àíàëèçà ñ èñïîëüçîâàíèåì îäíîïàðàìåòðè÷åñêèõ è ìíîãîïàðàìåòðè÷åñêèõ ìîäåëåé, ñïîñîáíîñòü ïðåäñêàçûâàòü ðåçóëüòàòû áèîïñèè ó áîëüíûõ ñ ïîâûøåííûìè êîíöåíòðàöèÿìè PSA. Ïîâûøåííûå êîíöåíòðàöèè uPAR â òêàíè ÐÏÆ àññîöèèðîâàíû ñ îñòåîáëàñòíûìè ìåòàñòàçàìè, à òàêæå ñ äàëåêî çàøåäøåé ïðîãðåññèé ÐÏÆ. Ïîâûøåíû êîíöåíòðàöèè uPa è uPAR â ñûâîðîòêå WWW.TERRAMEDIСA.SPB.RU ОБЗОРЫ êðîâè áîëüíûõ ÐÏÆ ñ ìåòàñòàçàìè â êîñòü.  ýòèõ èññëåäîâàíèÿõ ñîîáùàåòñÿ, ÷òî ïðåäîïåðàöèîííûå óðîâíè uPA â ïëàçìå ÿâëÿþòñÿ ïðåäñêàçàòåëüíûì ïðèçíàêîì ðåöèäèâîâ ïî áèîõèìè÷åñêèì ïðèçíàêàì è ìåòàñòàçèðîâàíèÿ è óêàçûâàþò íà íàëè÷èå îòäàëåííûõ ìåòàñòàçîâ íà ìîìåíò ëîêàëüíîé òåðàïèè. Äëÿ âûÿñíåíèÿ ïðîãíîñòè÷åñêîãî ïîòåíöèàëà uPa è uPAR íóæíû êðóïíûå ïðîñïåêòèâíûå èññëåäîâàíèÿ ïðîãðåññèè è ìåòàñòàçèðîâàíèÿ ÐÏÆ ïîñëå ïðåäîïåðàöèîííîãî îáñëåäîâàíèÿ. Инсулиноподобные факторы роста и связывающие их белки Èìååòñÿ ñâÿçü ìåæäó ÐÏÆ è ñûâîðîòî÷íûìè êîíöåíòðàöèÿìè èíñóëèíîïîäîáíûõ ôàêòîðîâ ðîñòà (IGF) è áåëêîâ, êîòîðûå èõ ñâÿçûâàþò (IGFBP). Ñåìåéñòâî IGF ñîñòîèò èç äâóõ áåëêîâ (IGF-1 , IGF-2), êîòîðûå ìîãóò ñâÿçûâàòüñÿ ñ äâóìÿ ðåöåïòîðàìè (IGFR1 è IGFR-2) è øåñòüþ ñâÿçûâàþùèìè áåëêàìè (IFFBP 1-6). Ïîâûøåííûå êîíöåíòðàöèè IGF-1 è ñíèæåííûå êîíöåíòðàöèè IGFBP-3 êîððåëèðóþò ñ ïîâûøåííûì ðèñêîì ðàçâèòèÿ ÐÏÆ. Êîíöåíòðàöèè IGF-1 âîçðàñòàþò ñ ïîâûøåíèåì ðèñêà ÐÏÆ íåçíà÷èòåëüíî, è â ýòîì îòíîøåíèè íå ïðåâîñõîäÿò PSA â êà÷åñòâå ìàðêåðà, îäíàêî ýòè ðåçóëüòàòû íå ïîëó÷èëè ïîäòâåðæäåíèÿ â äðóãèõ èññëåäîâàíèÿõ. Îñíîâíûì IGFBP, ïðîäóöèðóåìûì ïðîñòàòîé, ÿâëÿåòñÿ IGFBP-2, è îí òîæå ïîâûøàåòñÿ ïðè ÐÏÆ, õîòÿ â ëîêàëèçîâàííûõ îïóõîëÿõ åãî óðîâíè îáðàòíî êîððåëèðóþò ñ èõ ðàçìåðîì è ïðîãðåññèåé. Êîíöåíòðàöèÿ IGFBP-3 â ñûâîðîòêå îáðàòíî êîððåëèðóåò ñ íàëè÷èåì ìåòàñòàçîâ â êîñòü, íî ïðè ýòîì íåò ðàçíèöû ìåæäó áîëüíûìè ñ ëîêàëèçîâàííûì ÐÏÆ è çäîðîâûìè ëèöàìè. Слитные гены TMPRSS2:ERG и TMPRSS2:ETV1  ðàçâèòèè ðàêîâûõ çàáîëåâàíèé, îñîáåííî ãåìàòîëîãè÷åñêèõ, ïðèíèìàþò ó÷àñòèå ãåííûå ïåðåñòðîéêè. Îäíà òàêàÿ ïåðåñòðîéêà çàòðàãèâàåò ãåíû òðàíñêðèïöèîííûõ ôàêòîðîâ ERG (ãîìîëîã îíêîãåíà v-ets âèðóñà E26 ýðèòðîáëàñòîçà ó ïòèö) (ëîêóñ 21q22.2), ETV1 (âàðèàíò 1 ets) (ëîêóñ 7p21.1) è ãåí, êîäèðóþùèé çàÿêîðåííóþ â ìåìáðàíå ñåðèíîâóþ ïðîòåèíàçó TMPRSS2, êîòîðûé ëîêàëèçîâàí â ëîêóñå 21q22.3. Ïî ðåçóëüòàòàì àíàëèçà ïðîôèëÿ âûïàäàþùèõ öèòîãåíåòè÷åñêèõ ðåçóëüòàòîâ, ñâÿçàííûõ ñ ðàêîì (cancer outlier profile analysis, COPA ), ýòà ïåðåñòðîéêà ïðîèñõîäèò â 80% ñëó÷àåâ ÐÏÆ. Ñëèòíûé ïðîäóêò ýòèõ ãåíîâ âûÿâëÿåòñÿ ó 42% áîëüíûõ ÐÏÆ, ó 20% áîëüíûõ ñ èíòðàýïèòåëèàëüíîé íåîïëàçèåé ïðîñòàòû è ðåäêî – ïðè ÄÃÏÆ.  ïðîñïåêòèâíîì èññëåäîâàíèè, â êîòîðîì 252 áîëüíûõ ÐÏÆ íà ñòàäèè T1a/b íàáëþäàëè â òå÷åíèå 9 ëåò, ñëèòíûé ïðîäóêò TMPRSS2:ERG áûë áîëåå ñèëüíî, ÷åì TMPRSS2:ETV1, ñâÿçàí ñ èíäåêñîì ПОДПИСНОЙ ИНДЕКС 72075 Ãëèñîíà âûøå 7, ñ ìåòàñòàçàìè è ñî ñìåðòüþ îò ÐÏÆ. Èçîôîðìà TMPRSS2:ERG áûëà ïðîäåìîíñòðèðîâàíà ôëþîðåñöåíòíîé ãèáðèäèçàöèåé in situ â 80–95% îáðàçöîâ òêàíè ÐÏÆ è ìîæåò áûòü ïîòåíöèàëüíîé òåðàïåâòè÷åñêîé ìèøåíüþ. Âäîáàâîê, ñ íåáëàãîïðèÿòíûì ïðîãíîçîì ñâÿçàííîé îêàçàëàñü ïîâûøåííàÿ ïðîäóêöèÿ SPINK1, ñåðèíîâîé ïðîòåèíàçû, ìîãóùåé ñïîñîáñòâîâàòü èíâàçèè îïóõîëè ó áîëüíûõ, íåãàòèâíûõ ïî TMPRSS2:ETV1. Трансформирующий ростовый фактор-β1 Òðàíñôîðìèðóþùèé ðîñòîâûé ôàêòîð-β1 (TGF-β1) ÿâëÿåòñÿ ðîñòîâûì ôàêòîðîì øèðîêîãî äåéñòâèÿ, ó÷àñòâóþùèì âî ìíîæåñòâå ìîëåêóëÿðíûõ ïðîöåññîâ, òàêèõ êàê êëåòî÷íàÿ äèôôåðåíöèàöèÿ, èììóííûé îòâåò, àíãèîãåíåç è ïðîëèôåðàöèÿ. Èññëåäîâàíèÿ íà ìîäåëÿõ ÐÏÆ ïðîäåìîíñòðèðîâàëè ðîëü TGF-β1 â ïðîãðåññèè ÐÏÆ. Ïîâûøåííûå êîíöåíòðàöèè TGF-β1 â òêàíÿõ ÐÏÆ êîððåëèðóþò ñî ñòàäèåé è ñòåïåíüþ òðàíñôîðìàöèè è ñ ìåòàñòàçàìè â ëèìôàòè÷åñêèå óçëû. Ñ ïîìîùüþ èììóíîôåðìåíòíîãî àíàëèçà äëÿ îïðåäåëåíèÿ ïðåäîïåðàöèîííûõ êîíöåíòðàöèé TGF-β1 â ïëàçìå ïîêàçàíî, ÷òî óðîâåíü ýòîãî ôàêòîðà ïîâûøåí ó áîëüíûõ ÐÏÆ è êîððåëèðóåò ñ ýêñòðàêàïñóëÿðíûì ðàñïðîñòðàíåíèåì, èíâàçèåé â ñåìåííûå ïóçûðüêè, ìåòàñòàçàìè è áèîõèìè÷åñêèìè ðåöèäèâàìè. Òàêèì îáðàçîì, TGF-β1 ìîæåò áûòü ïîëåçíûì ïðîãíîñòè÷åñêèì ìàðêåðîì ÐÏÆ. Энхансер гомолога-2 белка Zeste EZH2 (ýíõàíñåð ãîìîëîãà-2 áåëêà Zeste äðîçîôèë) êîäèðóåò áåëîê, îòíîñÿùèéñÿ ê ñåìåéñòâó polycomb, ó÷àñòâóþùåìó â ðåãóëÿöèè ýêñïðåññèè ãåíîâ. Îïðåäåëåíèå ïðîôèëÿ ýêñïðåññèè áåëêîâ â òêàíÿõ ÐÏÆ, ïîëó÷åííûõ àóòîïñèåé, ïîêàçàëî, ÷òî ó áîëüíûõ, óìåðøèõ îò ìåòàñòàòè÷åñêîãî ÐÏÆ, EZH2 îáíàðóæèâàëè â ìåòàñòàçàõ ÐÏÆ â áî'ëüøèõ êîëè÷åñòâàõ, ÷åì â ëîêàëèçîâàííîì ÐÏÆ è ÄÃÏÆ. Ýòîò ìàðêåð ïðåâîñõîäèò ïðåäîïåðàöèîííûå êîíöåíòðàöèè PSA è ïîêàçàòåëü Ãëèñîíà â îïðåäåëåíèè ïðîãðåññèè ÐÏÆ. Ïðèìåíåíèå ýòîãî ìàðêåðà â ñî÷åòàíèè ñ e-êàäõåðèíîì ïðåäñêàçûâàåò ðåöèäèâû ÐÏÆ ïîñëå ìåñòíîé òåðàïèè. Ðàçðàáîòêà ñïîñîáîâ åãî îïðåäåëåíèÿ â ñûâîðîòêå äîëæíà ïîìî÷ü ïðè îöåíêå ýòîãî êàíäèäàòà â ìàðêåðû äëÿ èäåíòèôèêàöèè ïàöèåíòîâ ñ ðèñêîì ðàçâèòèÿ ìåòàñòàòè÷åñêîãî çàáîëåâàíèÿ. Гиперметилирование гена глутатион-S-трансферазы Ê ðàçâèòèþ ÐÏÆ ïðè÷àñòíî ãèïåðìåòèëèðîâàíèå ãåíîâ-ñóïðåññîðîâ îïóõîëåé ïî íóêëåîòèäíûì êëàñòåðàì CpG â èõ ïðîìîòîðàõ. Ôåðìåíò ãëóòàòèîí-Sòðàíñôåðàçà π çàùèùàåò ÄÍÊ îò ñâîáîäíîðàäèêàëüíîãî ïîâðåæäåíèÿ. Ñíèæåííàÿ ýêñïðåññèÿ ãåíà GSTP1 ïî 7 ОБЗОРЫ ïðè÷èíå ãèïåðìåòèëèðîâàíèÿ åãî ïðîìîòîðà íåèçìåí- è àññîöèèðîâàíû ñ ïðîãðåññèåé ÐÏÆ. Îíè ïðåäñêàíî îáíàðóæèâàåòñÿ ïðè ÐÏÆ, åå îïðåäåëåíèå â îñàä- çûâàþò íåçàâèñèìûé îò àíäðîãåíîâ ôåíîòèï ÐÏÆ. êå ìî÷è ìîæåò óêàçûâàòü íà íåîáõîäèìîñòü â áèîïñèè. Òàêèì îáðàçîì, êàê õðîìîãðàíèí `, òàê è ïåïòèäíûé Ýòîò àíàëèç óñîâåðøåíñòâîâàí äîáàâëåíèåì ìàññàæà ôàêòîð âûñâîáîæäåíèÿ ïðîãàñòðèíà ìîæíî èñïîëüïðîñòàòû ïåðåä ñáîðîì ìî÷è. Òàêèì æå îáðàçîì èç- çîâàòü äëÿ ìîíèòîðèíãà áîëüíûõ íà ïîçäíèõ ñòàäèÿõ íå÷óâñòâèòåëüíîãî ê ãîðìîíàì ÐÏÆ ñ ïðèçíàêàìè ó÷åíû öåëûå íàáîðû ãåíîâ, âêëþ÷àþùèå GSTP1. íåéðîýíäîêðèííîé äèôôåðåíöèàöèè. Секреторный белок 94 простаты и связывающий его белок Å-кадхерин Ìåæêëåòî÷íàÿ àäãåçèÿ èãðàåò âàæíóþ ðîëü â íîðÑåêðåòîðíûé áåëîê 94 ïðîñòàòû (PSP94 ), òàêæå èçâåñòíûé êàê β-ìèêðîñåìèíîïðîòåèí, ïðèñóòñòâóåò ìàëüíîì ïîñòðîåíèè òêàíè è ïðè êàíöåðîãåíåçå. â áîëüøèõ êîëè÷åñòâàõ â ñïåðìå è èãðàåò ðîëü â êëå- e-êàäõåðèí ÿâëÿåòñÿ ìîëåêóëîé êëåòî÷íîé àäãåçèè, òî÷íîé ïðîëèôåðàöèè è àïîïòîçå.  ñâÿçàííîì âèäå ïðîäóöèðóåìîé â ýïèòåëèàëüíûõ êëåòêàõ, åãî ïðîPSP94 ñóùåñòâóåò â âèäå êîìïëåêñà ñ PSP94-ñâÿçû- äóêöèÿ ýòèìè êëåòêàìè ÿâëÿåòñÿ ïðåäñêàçàòåëüíûì âàþùèì áåëêîì. Ñîîòíîøåíèå îáùåãî è ñâîáîäíîãî ïðèçíàêîì äëÿ ïðîãíîçà ÐÏÆ.  èììóíîãèñòîõèìè÷åñêîì èññëåäîâàíèè ïðîäåPSP94 è êîíöåíòðàöèÿ PSP94-ñâÿçûâàþùåãî áåëêà â ñûâîðîòêå ó áîëüíûõ ÐÏÆ ïîñëå ëîêàëüíîé îïåðàöèè ìîíñòðèðîâàíî, ÷òî ïðîäóêöèÿ e-êàäõåðèíà ñíèæåíà êîððåëèðóþò ñ ïîêàçàòåëåì Ãëèñîíà, áèîõèìè÷åñêèìè â 50% îïóõîëåé ÐÏÆ, òîãäà êàê â íîðìàëüíîé òêàïðèçíàêàìè ðåöèäèâîâ. Äëÿ îöåíêè ýòîò êàíäèäàòà â íè ïðîñòàòû ïðîäóêöèÿ e-êàäõåðèíà ðàñïðåäåëåíà áèîìàðêåðû âñå åùå òðåáóþòñÿ áîëüøèå ïðîñïåêòèâ- ðàâíîìåðíî.  äàëüíåéøèõ èññëåäîâàíèÿõ ïðîäóêöèÿ e-êàäõåðèíà áûëà àññîöèèðîâàíà ñî ñòåïåíüþ íûå èññëåäîâàíèÿ. òðàíñôîðìàöèè, ñòàäèåé îïóõîëè è âûæèâàåìîñòüþ Богатый цистеином секреторный белок 3 áîëüíûõ. Åãî ñíèæåííàÿ ïðîäóêöèÿ, ïî äàííûì èììóíîãèñòîõèìè÷åñêîãî àíàëèçà, ñâÿçàíà ñ ñîêðàùåÁîãàòûé öèñòåèíîì ñåêðåòîðíûé áåëîê 3 (CRISP-3) íèåì æèçíè áîëüíûõ ÐÏÆ. îáðàçóåòñÿ â ìóæñêèõ ïîëîâûõ ïóòÿõ, ãäå ó÷àñòâóåò â ñîçðåâàíèè ñïåðìû. Åãî áîëüøèå êîëè÷åñòâà âûÿâëåАннексин А3 íû â ïëàçìå ñïåðìû. Âäîáàâîê, îêðàøèâàíèå òêàíè Àííåêñèí 3 (ANXA3 ), ÷ëåí áåëêîâîãî ñåìåéñòâà ïðîñòàòû íà CRISP-3 ïîêàçàëî âîçðàñòàíèå åãî óðîâàííåêñèíîâ, ÿâëÿåòñÿ ñâÿçûâàþùèì êàëüöèé áåëêîì. íÿ ïðè ñèëüíî òðàíñôîðìèðîâàííûõ èíòðàýïèòåëèANXA3 ó÷àñòâóåò â àêòèâàöèè èììóííîãî îòâåòà, à òàêàëüíûõ íåîïëàçèÿõ â íåñêîëüêèõ ïðîáàõ òêàíè ÐÏÆ. æå â ðåãóëÿöèè ïðîíèöàåìîñòè ìåìáðàí è ìèãðàöèè Àññîöèàöèÿ ìåæäó CRISP-3 è ÐÏÆ áûëà ïðîâåðåíà â ëèìôîöèòîâ. Íåäàâíî ANXA3 áûë èññëåäîâàí èììóñâÿçè ñ îïðåäåëåíèåì β-ìèêðîñåìèíîïðîòåèíà â òêàíîãèñòîõèìè÷åñêèìè ìåòîäàìè â êà÷åñòâå ïåðñïåêòèâíÿõ, ïîëó÷åííûõ ïðè ðàäèêàëüíîé ïðîñòàòýêòîìèè. Îêàçàëîñü, ÷òî CRISP-3 ÿâëÿåòñÿ íåçàâèñèìûì ïðåä- íîãî òêàíåâîãî ìàðêåðà äëÿ ïðîãíîçà ÐÏÆ. Áûëà âûñêàçàòåëüíûì ïðèçíàêîì ðåöèäèâîâ ÐÏÆ. Òàêèì îá- ÿâëåíà åãî ñíèæåííàÿ ïðîäóêöèÿ â ÐÏÆ â ñðàâíåíèè ðàçîì, ýòîò áåëîê ìîæíî ñ÷èòàòü íîâûì òêàíåâûì ÄÃÏÆ, èíòðàýïèòåëèàëüíîé íåîïëàçèåé è çäîðîâûìè òêàíÿìè. Ñ ïîìîùüþ îïðåäåëåíèÿ ANXA3 ìîæíî ñòðàìàðêåðîì äëÿ ïðîãíîçà ÐÏÆ. òèôèöèðîâàòü áîëüøóþ ãðóïïó áîëüíûõ ïðîìåæóòî÷íîãî ðèñêà íà ïîäãðóïïû âûñîêîãî è íèçêîãî ðèñêà. Маркеры нейроэндокринной дифференциации Ïåïòèä õðîìîãðàíèí `, êîòîðûé ïðîäóöèðóåòñÿ íåéðîýíäîêðèííûìè êëåòêàìè ïðîñòàòû, â íàñòîÿùåå âðåìÿ èñïîëüçóþò â äèàãíîñòèêå ÐÏÆ è ïðîãíîçèðîâàíèè â ñëó÷àÿõ îïóõîëåé ïðîñòàòû, èìåþùèõ ïðèçíàêè íåéðîýíäîêðèííîé äèôôåðåíöèàöèè. Ïîâûøåíèå êîíöåíòðàöèè õðîìîãðàíèíà ` â ñûâîðîòêå êîððåëèðóåò ñ ïðîãðåññèåé ÐÏÆ, íåçàâèñèìîãî îò àíäðîãåíîâ, è ïëîõîãî ïðîãíîçà. Îíî ïðåäøåñòâóåò ïîâûøåíèþ PSA è óëó÷øàåò äèàãíîñòè÷åñêóþ ñïåöèôè÷íîñòü â ñðàâíåíèè ñ fPSA. Ïåïòèäíûé ôàêòîð âûñâîáîæäåíèÿ ïðîãàñòðèíà ÿâëÿåòñÿ ðîñòîâûì ôàêòîðîì, êîòîðûé îáðàçóåòñÿ â íåéðîýíäîêðèííûõ òèïàõ ÐÏÆ. Åãî ïîâûøåííûå êîíöåíòðàöèè âûÿâëåíû ïðè ìåòàñòàòè÷åñêîì ÐÏÆ 8 Антиген стволовых клеток предстательной железы Àíòèãåí ñòâîëîâûõ êëåòîê ïðîñòàòû (PSCA) ÿâëÿåòñÿ ìåìáðàííûì ãëèêîïðîòåèíîì, âåñüìà ñïåöèôè÷åñêè ïðîäóöèðóåìûì â ïðîñòàòå. PSCA âûÿâëåí â òêàíÿõ ÐÏÆ èììóíîãèñòîõèìè÷åñêèìè ìåòîäàìè, à åãî ÐÍÊ íàéäåíà â îáðàçöàõ êðîâè. Ïîâûøåííàÿ ïðîäóêöèÿ PSCA êîððåëèðóåò ñ ïîâûøåííûì ðèñêîì ÐÏÆ, áîëåå âûñîêèì êîýôôèöèåíòîì Ãëèñîíà, áîëåå âûñîêîé ñòàäèåé è íàëè÷èåì ìåòàñòàçîâ. PSCA òàêæå èññëåäîâàí â êà÷åñòâå òåðàïåâòè÷åñêîé ìèøåíè, îäíàêî äëÿ ïîäòâåðæäåíèÿ êëèíè÷åñêîé ïðèìåíèìîñòè ýòîãî ìàðêåðà òðåáóþòñÿ áîëåå îáøèðíûå àïðîáàöèîííûå èññëåäîâàíèÿ. WWW.TERRAMEDIСA.SPB.RU ОБЗОРЫ Гепсин Ãåïñèí ÿâëÿåòñÿ ìåìáðàííîé ñåðèíîâîé ïðîòåàçîé, âïåðâûå èäåíòèôèöèðîâàííîé â áèáëèîòåêàõ êÄÍÊ ïå÷åíè.  áîëüøèõ êîëè÷åñòâàõ îí îáðàçóåòñÿ â òêàíÿõ ïðîñòàòû. Èññëåäîâàíèÿ ïðîôèëÿ ýêñïðåññèè ìÐÍÊ ãåïñèíà ïðîäåìîíñòðèðîâàëè ïîâûøåííóþ ýêñïðåññèþ åãî ãåíà â 90 % ÐÏÆ. Íàáëþäàåòñÿ ñèëüíîå èììóíîãèñòîõèìè÷åñêîå îêðàøèâàíèå íà ãåïñèí â èíòðàýïèòåëèàëüíûõ êàðöèíîìàõ ïðîñòàòû è åãî ïðåèìóùåñòâåííîå îáðàçîâàíèå ïðè ÐÏÆ, à íå ÄÃÏÆ. Äëÿ ïîëíîãî âûÿñíåíèÿ äèàãíîñòè÷åñêîãî ïîòåíöèàëà ãåïñèíà òðåáóþòñÿ äàëüíåéøèå èññëåäîâàíèÿ íà îáðàçöàõ êðîâè è ìî÷è. Интерлейкин 6 и его рецептор Èíòåðëåéêèí 6 (IL-6 ) ÿâëÿåòñÿ öèòîêèíîì, êîòîðûé ïðîäóöèðóåò êëåòêè ìíîãèõ òèïîâ, îí ó÷àñòâóåò â èììóííîì îòâåòå è â ðåàêöèè îñòðîé ôàçû. Ïîâûøåííûå êîíöåíòðàöèè IL-6 è åãî ðåöåïòîðîâ ïðîäåìîíñòðèðîâàíû ïðè ìåòàñòàòè÷åñêîì è íåçàâèñèìîì îò àíäðîãåíîâ ÐÏÆ, îí ïðåäëîæåí â êà÷åñòâå êàíäèäàòà â ìàðêåðû ïðîãðåññèðîâàíèÿ ÐÏÆ. Ìíîãîîáåùàþùèå ðåçóëüòàòû äàëè èññëåäîâàíèÿ IL-6 â êîìáèíàöèè ñ TGF-β1 äëÿ äèàãíîñòèêè ÐÏÆ. Циркулирующая опухолевая ДНК Äèññåìèíàöèÿ îïóõîëåâûõ êëåòîê ÿâëÿåòñÿ íåîáõîäèìûì óñëîâèåì ìåòàñòàçèðîâàíèÿ, è ðàííåå âûÿâëåíèå òàêèõ êëåòîê â öèðêóëèðóþùåé êðîâè ìîæåò áûòü ïîëåçíûì äëÿ ïðîãíîçà áîëüíûõ ÐÏÆ. Îïóõîëåâûå êëåòêè ìîæíî âûÿâëÿòü â îáðàòíîòðàíñêðèïòàçíîé ÏÖÐ, êîòîðàÿ îêàçàëàñü äîñòàòî÷íî ÷óâñòâèòåëüíîé äëÿ ïîâûøåíèÿ äèàãíîñòè÷åñêîé òî÷íîñòè îïðåäåëåíèÿ ñòàäèè ÐÏÆ, ïðåäñêàçàíèÿ ðåöèäèâîâ ñ ïîìîùüþ ìàðêåðîâ, ñïåöèôè÷íûõ äëÿ ïðîñòàòû. Аутоантитела Èçâåñòíî, ÷òî èììóííàÿ ñèñòåìà îòâå÷àåò íà íåêîòîðûå îïóõîëåâûå àíòèãåíû óñèëåíèåì ïðîäóêöèè àóòîàíòèòåë. Ñîîáùàåòñÿ î ãóìîðàëüíûõ îòâåòàõ íà áåëîê-1, âçàèìîäåéñòâóþùèé ñ õàíòèíãòèíîì, íà ïðîñòàñîìå è íà AMACR. Ñ èñïîëüçîâàíèåì ôàãîâîãî äèñïëåÿ è áåëêîâûõ ìèêðî÷èïîâ â ðàìêàõ íîâîãî ïîäõîäà «èììóíîìèêà ðàêà» óäàëîñü èäåíòèôèöèðîâàòü àóòîàíòèòåëà ê ïåïòèäàì, ïðîèñõîäÿùèì èç òêàíåé ÐÏÆ. Áûë ñîçäàí 22-ïåïòèäíûé ôàãîâûé äèñïëåé, ïîçâîëèâøèé îòëè÷èòü 69 îáðàçöîâ ñûâîðîòêè êðîâè áîëüíûõ ÐÏÆ îò 66% êîíòðîëåé ïðè äèàãíîñòè÷åñêîé ñïåöèôè÷íîñòè 88,2% è ÷óâñòâèòåëüíîñòè 81% ñ ïëîùàäüþ ïîä êðèâîé ROC 0,93, ÷òî ëó÷øå, ÷åì ïðè èñïîëüçîâàíèè PSA (0,80). Ïðîâîäÿòñÿ èññëåäîâàíèÿ ïî äàëüíåéøåé àïðîáàöèè ýòîãî ìåòîäà íà áîëåå ìíîãî÷èñëåííîé êîãîðòå.  íåäàâíåì èññëåäîâàíèè ïðèìåíåí òàêîé æå ïîäõîä, çàòåì ïðîâåäåí ПОДПИСНОЙ ИНДЕКС 72075 àíàëèç áèîëîãè÷åñêèõ ïóòåé âçàèìîäåéñòâèÿ ñîîòâåòñòâóþùèõ ôàêòîðîâ äëÿ îïðåäåëåíèÿ ìåõàíèçìîâ ïðîãðåññèè ÐÏÆ. Îäíîé èç ïðîáëåì çäåñü ÿâëÿåòñÿ íåîáõîäèìîñòü ïóíêöèîííîé áèîïñèè, êîòîðàÿ ñàìà ïî ñåáå ìîæåò âûçûâàòü èììóííûé îòâåò. Номограммы Íîìîãðàììû ÿâëÿþòñÿ ñðåäñòâîì ìíîãîôàêòîðíîãî àíàëèçà ñî÷åòàíèé òàêèõ ïðèçíàêîâ, êàê ñòåïåíü òðàíñôîðìàöèè/ñòàäèÿ îïóõîëè è óðîâíè áèîìàðêåðîâ äëÿ îáåñïå÷åíèÿ ñòàíäàðòèçàöèè ñïîñîáîâ âûðàáîòêè ëå÷åáíîé òàêòèêè. Îíè îñíîâàíû íà ïðèíöèïàõ äîêàçàòåëüíîé ìåäèöèíû äëÿ ïðèíÿòèÿ ðåøåíèé íà êàæäîé ñòàäèè ëå÷åíèÿ áîëåçíè. Öåííîñòü íîìîãðàìì îïðåäåëÿåòñÿ ýôôåêòèâíîñòüþ è ðàçâåðíóòîñòüþ. Äëÿ ÐÏÆ ðàçðàáîòàíû ìíîãî÷èñëåííûå íîìîãðàììû, â òîì ÷èñëå ó÷èòûâàþùèå TGF-β1 è IL-6 äëÿ ðåöèäèâîâ ïî áèîõèìè÷åñêèì ïðèçíàêàì, à òàêæå íîìîãðàììû äëÿ ïðåäñêàçàíèÿ ðåçóëüòàòîâ áèîïñèè. Многопараметрические тесты/ нейрональные сети Äëÿ óëó÷øåíèÿ ïðåäñêàçàíèÿ ïðè ìíîãèõ çàáîëåâàíèÿõ øèðîêî èñïîëüçóþò êîìáèíàöèè áèîìàðêåðîâ. Âñå ëþäè ðàçíûå, è áîëåçíåííûå ñîñòîÿíèÿ ó íèõ òàêæå ðàçëè÷íû. Òàêèì îáðàçîì, ìíîãîïàðàìåòðè÷åñêèå òåñòû äîëæíû áûòü áîëåå àäåêâàòíûìè äëÿ ïîïóëÿöèîííîãî ñêðèíèíãà, ÷åì îòäåëüíûé ìàðêåð. Íåäàâíî áûëà ïðîâåðåíà ïàíåëü èç 45 áèîìàðêåðîâ, âêëþ÷àþùàÿ àäèïîêèíû, ìåòàëëîïðîòåèíàçû, ìîëåêóëû àäãåçèè è ðîñòîâûå ôàêòîðû. Ïîêàçàòåëè â ñûâîðîòêå îïðåäåëÿëè äî ïîñòàíîâêè äèàãíîçà ó ëèö îäíîé âîçðàñòíîé ãðóïïû è ñðàâíèâàëè ìåæäó ñëó÷àÿìè, êîãäà â äàëüíåéøåì äèàãíîç ÐÏÆ áûë èëè íå áûë ïîñòàâëåí. Ïðè ýòîì íå óäàëîñü ïîêàçàòü, ÷òî òàêàÿ ïàíåëü ïðåâîñõîäèò «êàëüêóëÿòîð» ôàêòîðîâ ðèñêà, ðàçðàáîòàííûé â ðàìêàõ ïðîåêòà «Èçó÷åíèå ïðîôèëàêòèêè ðàêà ïðîñòàòû». Äëÿ ìîäåëèðîâàíèÿ ñëîæíûõ îòíîøåíèé ìåæäó ðàçíûìè ôàêòîðàìè è èäåíòèôèêàöèè ðàçíûõ ïàòòåðíîâ äàííûõ èñïîëüçîâàëè ìåòîä íåéðîííûõ ñåòåé. Íàïðèìåð, äëÿ ÐÏÆ îöåíèâàëè ðàçíûå êîìáèíàöèè êàëëèêðåèíîâûõ áèîìàðêåðîâ. Протеомные паттерны Ñ íåäàâíèõ ïîð ïîïóëÿðíûì ïîäõîäîì ê èäåíòèôèêàöèè íîâûõ áèîìàðêåðîâ ñòàë âûñîêîïðîèçâîäèòåëüíûé ïðîòåîìíûé àíàëèç áèîëîãè÷åñêèõ æèäêîñòåé. Ñ ýòîé öåëüþ èñïîëüçîâàëè ìàññ-ñïåêòðîìåòðèþ ñ ïîâåðõíîñòíûì óñèëåíèåì ïðè èîíèçàöèè ëàçåðíûì èçëó÷åíèåì â ñî÷åòàíèè ñ ãàçîõðîìàòîãðàôè÷åñêèì îïðåäåëåíèåì âðåìåíè ïðîëåòà èîíîâ (surfaceenhanced laser desorption/ionization time-of-flight mass spectrometry, SELDI-TOF-MS).  ñëó÷àå ÐÏÆ 9 ОБЗОРЫ èñïîëüçîâàëè åùå è àëãîðèòì äåðåâà ðåøåíèé äëÿ èäåíòèôèêàöèè ñî÷åòàíèé ïèêîâ, ñïîñîáíûõ äèôôåðåíöèðîâàòü áîëüíûõ è çäîðîâûõ ëèö ïðè äèàãíîñòè÷åñêîé ÷óâñòâèòåëüíîñòè è ñïåöèôè÷íîñòè 83 è 97%, ñîîòâåòñòâåííî. Ïðè èññëåäîâàíèè 266 îáðàçöîâ ñûâîðîòêè ó áîëüíûõ ÐÏÆ è çäîðîâûõ, áûëà äîñòèãíóòà äèàãíîñòè÷åñêàÿ ÷óâñòâèòåëüíîñòü 95 % è ñïåöèôè÷íîñòü 78%. Ïðè èñïîëüçîâàíèè óñîâåðøåíñòâîâàííîãî àëãîðèòìà äåðåâà ðåøåíèé íà äðóãîì ìàññèâå äàííûõ áûëà äîñòèãíóòà äèàãíîñòè÷åñêàÿ ÷óâñòâèòåëüíîñòü 97% è ñïåöèôè÷íîñòü 97%. Ïîëåçíîñòü òàêîãî ïîäõîäà ïðîäåìîíñòðèðîâàíà è äðóãèìè èññëåäîâàíèÿìè. Îäíàêî îí ïîïàë ïîä ñêðóïóëåçíóþ ïðîâåðêó Íàöèîíàëüíîãî ïðîòèâîðàêîâîãî èíñòèòóòà ÑØÀ, ãäå áûëà ó÷ðåæäåíà Èññëåäîâàòåëüñêàÿ ñåòü ïî ðàííåìó âûÿâëåíèþ ÐÏÆ, êîòîðàÿ ïðîâåëà èññëåäîâàíèå ñ ó÷àñòèåì ìíîãèõ ó÷ðåæäåíèé, ðåçóëüòàòû êîòîðîãî áûëè íåäàâíî îïóáëèêîâàíû. Õîòÿ íà I ñòàäèè áûëà ïîäòâåðæäåíà àíàëèòè÷åñêàÿ âîñïðîèçâîäèìîñòü òàêîãî ïîäõîäà, íà II ñòàäèè, ïðîâåäåííîé ïî ñõåìå «ñëó÷àé-êîíòðîëü», íå óäàëîñü ïîêàçàòü, ÷òî îí îáåñïå÷èâàåò ïðåäñêàçàíèå ÐÏÆ âî âñåõ ó÷ðåæäåíèÿõ. Ýòó íåóäà÷ó îòíåñëè ê ïðåàíàëèòè÷åñêèì, àíàëèòè÷åñêèì è áèîèíôîðìàöèîííûì èñêàæåíèÿì, óæå îïèñàííûì â ëèòåðàòóðå. Òàêèì îáðàçîì, ìîæíî çàêëþ÷èòü, ÷òî âíåäðåíèå àíàëèçîâ êðîâè íà PSA ðåâîëþöèîíèçèðîâàëî äèàãíîñòèêó è ëå÷åíèå ÐÏÆ. Îäíàêî âñå åùå ñóùåñòâóþò ïðîòèâîðå÷èÿ ïî âîïðîñó, ñíèæàåò ëè ñêðèíèíã íà PSA ñìåðòíîñòü îò ÐÏÆ è ðèñêè, ñâÿçàííûå ñ èçáûòî÷íûì ÷èñëîì ïîëîæèòåëüíûõ äèàãíîçîâ. Ñóùåñòâóþò ñâèäåòåëüñòâà ïðèìåíèìîñòè ìíîæåñòâåííûõ ìàðêåðîâ äëÿ áîëåå ïîëíîé õàðàêòåðèçàöèè ôåíîòèïîâ îïóõîëåé ïðîñòàòû âî âñåé ìóæñêîé ïîïóëÿöèè. Ïðèìåíåíèå ìíîãî÷èñëåííûõ ìàðêåðîâ â ñî÷åòàíèè ñ êëèíè÷åñêèìè è äåìîãðàôè÷åñêèìè äàííûìè äîëæíî ïîìî÷ü â ïðåäñêàçàíèè òîãî, êàêèå ïàöèåíòû íàõîäÿòñÿ ïîä ðèñêîì ðàçâèòèÿ ÐÏÆ, è â îöåíêå ïðîãíîçîâ äëÿ íèõ. Íîâûå èññëåäîâàòåëüñêèå âîçìîæíîñòè äîëæíû ïîìî÷ü â âûÿâëåíèè íîâûõ ìàðêåðîâ, îäíàêî êëþ÷åâûì äëÿ ïîëó÷åíèÿ âîñïðîèçâîäèìûõ è íåèñêàæåííûõ ðåçóëüòàòîâ îñòàåòñÿ ïðèìåíåíèå íàäëåæàùèõ ñõåì èññëåäîâàíèÿ è àíàëèçà êëèíè÷åñêèõ äàííûõ. qC,“%* ,2!=23!/ “. " %!,',…= …% ,“2%#…,* qC,“%* ,2!=23!/ “%2!, …= “=L2 www.terramedica.spb.ru 10 WWW.TERRAMEDIСA.SPB.RU g ОБЗОРЫ Литература 1. Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin 2007;57:43–66. 2. McDavid K, Lee J, Fulton JP, Tonita J, Thompson TD. Prostate cancer incidence and mortality rates and trends in the United States and Canada. Public Health Rep 2004;119:174 –86. 3. Thompson IM, Ankerst DP, Chi C, Lucia MS, Goodman PJ, Crowley JJ, et al. Operating characteristics of prostate-specific antigen in men with an initial PSA level of 3.0 ng/mL or lower. JAMA 2005;294:66–70. 4. Aihara M, Lebovitz RM, Wheeler TM, Kinner BM, Ohori M, Scardino PT. Prostate specific antigen and Gleason grade: an immunohistochemical study of prostate cancer. J Urol 1994;151:1558 –64. 5. Bunting PS. Screening for prostate cancer with prostate-specific antigen: beware the biases. Clin Chim Acta 2002;315:71–97. 6. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level �4.0 ng per milliliter. N Engl J Med 2004;350:2239 –46. 7. Pepe MS, Etzioni R, Feng Z, Potter JD, Thompson ML, Thornquist M, et al. Phases of biomarker development for early detection of cancer. J Natl Cancer Inst 2001;93:1054 –61. 8. McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM. Reporting recommendations for tumor marker prognostic studies (REMARK). J Natl Cancer Inst 2005;97:1180 –4. 9. Finne P, Auvinen A, Ma.a.tta.nen L, Tammela TL, Ruutu M, Juusela H, et al. Diagnostic value of free prostate-specific antigen among men with a prostatespecific antigen level of <3.0 µg per liter. Eur Urol 2008;54:362–70. 10. Stephan C, Jung K, Lein M, Diamandis EP. PSA and other tissue kallikreins for prostate cancer detection. Eur J Cancer 2007;43:1918–26. 11. Recker F, Kwiatkowski MK, Piironen T, Pettersson K, Huber A, Lummen G, Tscholl R. Human glandular kallikrein as a tool to improve discrimination of poorly differentiated and non-organ-confined prostate cancer compared with prostate-specific antigen. Urology 2000;55:481–5. 12. Stephan C, Jung K, Nakamura T, Yousef GM, Kristiansen G, Diamandis EP. Serum human glandular kallikrein 2 (hK2) for distinguishing stage and grade of prostate cancer. Int J Urol 2006;13: 238–43. 13. Haese A, Graefen M, Steuber T, Becker C, Noldus J, Erbersdobler A, et al. Total and Gleason grade of data, or preparation or approval of manuscript. 4/5 cancer volumes are major contributors of human kallikrein 2, whereas free prostate specific antigen is largely contributed by benign gland volume in serum from patients with prostate cancer or benign prostatic biopsies. J Urol 2003; 170:2269–73. 14. Steuber T, Vickers AJ, Haese A, Becker C, Pettersson K, Chun FK, et al. Risk assessment for biochemical recurrence prior to radical prostatectomy: significant enhancement contributed by human glandular kallikrein 2 (hK2) and free prostate specific antigen (PSA) in men with moderate PSA-elevation in serum. Int J Cancer 2006;118: 1234–40. 15. Elgamal AA, Holmes EH, Su SL, Tino WT, Sim¬mons SJ, Peterson M, et al. Prostate-specific membrane antigen (PSMA): current benefits and future value. Semin Surg Oncol 2000;18:10 –6. 16. Mincheff M, Zoubak S, Makogonenko Y. Immune responses against PSMA after gene-based vaccination for immunotherapy-A: results from immunizations in animals. Cancer Gene Ther 2006;13: 436–44. 17. Diamandis EP, Okui A, Mitsui S, Luo LY, Soosaipillai A, Grass L, et al. Human kallikrein 11: a new biomarker of prostate and ovarian carcinoma. Cancer Res 2002;62:295–300. 18. Stephan C, Meyer HA, Cammann H, Nakamura T, Diamandis EP, Jung K. Improved prostate cancer detection with a human kallikrein 11 and percentage free PSA-based artificial neural network. Biol Chem 2006;387:801–5. 19. Hessels D, Klein Gunnewiek JM, van Oort I, Karthaus HF, van Leenders GJ, van Balken B, et al. DD3(PCA3)-based molecular urine analysis for the diagnosis of prostate cancer. Eur Urol 2003; 44:8–15. 20. Groskopf J, Aubin SM, Deras IL, Blase A, Bodrug S, Clark C, et al. APTIMA PCA3 molecular urine test: development of a method to aid in the diagnosis of prostate cancer. Clin Chem 2006;52: 1089–95. 21. van Gils MP, Hessels D, van Hooij O, Jannink SA, Peelen WP, Hanssen SL, et al. The time-resolved fluorescence-based PCA3 test on urinary sediments after digital rectal examination; a Dutch multicenter validation of the diagnostic performance. Clin Cancer Res 2007;13:939 –43. 22. Marks LS, Fradet Y, Deras IL, Blase A, Mathis J, Aubin SM, et al. PCA3 molecular urine assay for prostate cancer in men undergoing repeat biopsy. Urology 2007;69:532–5. 23. Laxman B, Morris DS, Yu J, Siddiqui J, Cao J, Mehra R, et al. A firstgeneration multiplex biomarker analysis of urine for the early detection of prostate cancer. Cancer Res 2008;68:645–9. 24. Uetsuki H, Tsunemori H, Taoka R, Haba R, Ishikawa M, Kakehi Y. Expression of a novel biomarker, EPCA, in adenocarcinomas and precancerous lesions in the prostate. J Urol 2005;174:514 –8. 25. Paul B, Dhir R, Landsittel D, Hitchens MR, Getzenberg RH. Detection of prostate cancer with a blood-based assay for early prostate cancer antigen. Cancer Res 2005;65:4097–100. 26. Leman ES, Cannon GW, Trock BJ, Sokoll LJ, Chan DW, Mangold L, et al. EPCA-2: a highly specific serum marker for prostate cancer. Urology 2007; 69:714–20. 27. Diamandis EP. POINT: EPCA-2: a promising new serum biomarker for prostatic carcinoma? Clin Biochem 2007;40:1437–9. 28. Rhodes DR, Barrette TR, Rubin MA, Ghosh D, Chinnaiyan AM. Metaanalysis of microarrays: interstudy validation of gene expression profiles reveals pathway dysregulation in prostate cancer. Cancer Res 2002;62:4427–33. 29. Jiang Z, Wu CL, Woda BA, Iczkowski KA, Chu PG, Tretiakova MS, et al. Alpha-methylacyl-CoA racemase: a multi-institutional study of a new prostate cancer marker. Histopathology 2004;45: 218–25. 30. Rubin MA, Bismar TA, Andren O, Mucci L, Kim R, Shen R, et al. Decreased alpha-methylacyl CoA racemase expression in localized prostate cancer is associated with an increased rate of biochemical recurrence and cancer-specific death. Cancer Epidemiol Biomarkers Prev 2005;14:1424–32. 31. Zehentner BK, Secrist H, Zhang X, Hayes DC, Ostenson R, Goodman G, et al. Detection of alpha-methylacyl-coenzyme-A racemase transcripts in blood and urine samples of prostate cancer patients. Mol Diagn Ther 2006;10:397– 403. 32. Rogers CG, Yan G, Zha S, Gonzalgo ML, Isaacs WB, Luo J, et al. Prostate cancer detection on urinalysis for alpha methylacyl coenzyme A racemase protein. J Urol 2004;172:1501–3. 33. Sreekumar A, Laxman B, Rhodes DR, Bhagavathula S, Harwood J, Giacherio D, et al. Humoral immune response to alpha-methylacyl-CoA racemase and prostate cancer. J Natl Cancer Inst 2004;96:834–43. 34. McCabe NP, Angwafo FF III, Zaher A, Selman SH, Kouinche A, Jankun J. Expression of soluble urokinase plasminogen activator receptor may be related to outcome in prostate cancer patients. Oncol Rep 2000;7:879 –82. 35. Steuber T, Vickers A, Haese A, Kattan MW, Eastham JA, Scardino PT, et al. Free PSA isoforms and intact and cleaved forms of urokinase plasminogen activator receptor in serum improve selection of patients for prostate cancer biopsy. Int J Cancer 2007;120:1499–504. 36. Miyake H, Hara I, Yamanaka K, Gohji K, Arakawa S, Kamidono S. Elevation of serum levels of urokinase-type plasminogen activator and its receptor is associated with disease progression and prognosis in patients with prostate cancer. Prostate 1999;39:123–9. 37. Shariat SF, Roehrborn CG, McConnell JD, Park S, Alam N, Wheeler TM, Slawin KM. Association of the circulating levels of the urokinase system of plasminogen activation with the presence of prostate cancer and invasion, progression, and metastasis. J Clin Oncol 2007;25:349–55. 38. Chan JM, Stampfer MJ, Giovannucci E, Gann PH, Ma J, Wilkinson P, et al. Plasma insulin-like growth factor-I and prostate cancer risk: a prospective study. Science 1998;279:563–6. 39. Harman SM, Metter EJ, Blackman MR, Landis PK, Carter HB. Serum levels of insulin-like growth factor I (IGF-I), IGF-II, IGF-binding protein-3, and prostate-specific antigen as predictors of clinical prostate cancer. J Clin Endocrinol Metab 2000; 85:4258–65. 40. Shariat SF, Lamb DJ, Kattan MW, Nguyen C, Kim J, Beck J, et al. Association of preoperative plasma levels of insulin-like growth factor I and insulin-like growth factor binding proteins-2 and -3 with prostate cancer invasion, progression, and metastasis. J Clin Oncol 2002;20:833–41. 41. Tomlins SA, Rhodes DR, Perner S, Dhanasekaran SM, Mehra R, Sun XW, et al. Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science 2005;310:644 –8. 42. Laxman B, Tomlins SA, Mehra R, Morris DS, Wang L, Helgeson BE, et al. Noninvasive detection of TMPRSS2:ERG fusion transcripts in the urine of men with prostate cancer. Neoplasia 2006;8:885–8. 43. Demichelis F, Fall K, Perner S, Andren O, Schmidt F, Setlur SR, et al. TMPRSS2:ERG gene fusion associated with lethal prostate cancer in a watchful waiting cohort. Oncogene 2007;26:4596–9. 11 44. Tomlins SA, Rhodes DR, Yu J, Varambally S, Mehra R, Perner S, et al. The role of SPINK1 in ETS rearrangement-negative prostate cancers. Cancer Cell 2008;13:519–28. 45. Shariat SF, Menesses-Diaz A, Kim IY, Muramoto M, Wheeler TM, Slawin KM. Tissue expression of transforming growth factor-β1 and its receptors: correlation with pathologic features and biochemical progression in patients undergoing radical prostatectomy. Urology 2004;63:1191–7. 46. Ivanovic V, Melman A, Davis-Joseph B, Valcic M, Geliebter J. Elevated plasma levels of TGF-beta 1 in patients with invasive prostate cancer. Nat Med 1995;1:282–4. 47. Shariat SF, Walz J, Roehrborn CG, Montorsi F, Jeldres C, Saad F, Karakiewicz PI. Early postoperative plasma transforming growth factor-β1 is a strong predictor of biochemical progression after radical prostatectomy. J Urol 2008;179:1593–7. 48. Varambally S, Dhanasekaran SM, Zhou M, Barrette TR, Kumar-Sinha C, Sanda MG, et al. The polycomb group protein EZH2 is involved in progression of prostate cancer. Nature 2002;419: 624–9. 49. Rhodes DR, Sanda MG, Otte AP, Chinnaiyan AM, Rubin MA. Multiplex biomarker approach for determining risk of prostate-specific antigen-defined recurrence of prostate cancer. J Natl Cancer Inst 2003;95:661–8. 50. Gonzalgo ML, Nakayama M, Lee SM, De Marzo AM, Nelson WG. Detection of GSTP1 methylation in prostatic secretions using combinatorial MSP analysis. Urology 2004;63:414 –8. 51. Crocitto LE, Korns D, Kretzner L, Shevchuk T, Blair SL, Wilson TG, et al. Prostate cancer molecular markers GSTP1 and hTERT in expressed prostatic secretions as predictors of biopsy results. Urology 2004;64:821–5. 52. Nam RK, Reeves JR, Toi A, Dulude H, Trachtenberg J, Emami M, et al. A novel serum marker, total prostate secretory protein of 94 amino acids, improves prostate cancer detection and helps identify high grade cancers at diagnosis. J Urol 2006;175:1291–7. 53. Bjartell A, Johansson R, Bjork T, Gadaleanu V, Lundwall A, Lilja H, et al. Immunohistochemical detection of cysteine-rich secretory protein 3 in tissue and in serum from men with cancer or benign enlargement of the prostate gland. Prostate 2006;66:591–603. 54. Bjartell AS, Al Ahmadie H, Serio AM, Eastham JA, Eggener SE, Fine SW, et al. Association of cysteine-rich secretory protein 3 and β-microseminoprotein with outcome after radical prostatectomy. Clin Cancer Res 2007;13:4130 –8. 55. Taplin ME, George DJ, Halabi S, Sanford B, Febbo PG, Hennessy KT, et al. Prognostic significance of plasma chromogranin A levels in patients with hormone-refractory prostate cancer treated in Cancer and Leukemia Group B 9480 study. Urology 2005;66:386–91. 56. Fracalanza S, Prayer-Galetti T, Pinto F, Navaglia F, Sacco E, Ciaccia M, et al. Plasma chromogranin A in patients with prostate cancer improves the diagnostic efficacy of free/total prostate-specific antigen determination. Urol Int 2005;75:57–61. 57. Yashi M, Nukui A, Kurokawa S, Ochi M, Ishikawa S, Goto K, et al. Elevated serum progastrin-releasing peptide (31–98) level is a predictor of short response duration after hormonal therapy in metastatic prostate cancer. Prostate 2003;56: 305–12. 58. Yashi M, Muraishi O, Kobayashi Y, Tokue A, Nanjo H. Elevated serum progastrin-releasing peptide (31–98) in metastatic and androgen-independent prostate cancer patients. Prostate 2002;51:84–97. 59. Umbas R, Schalken JA, Aalders TW, Carter BS, Karthaus HF, Schaafsma HE, et al. Expression of the cellular adhesion molecule E-cadherin is reduced or absent in high-grade prostate cancer. Cancer Res 1992;52:5104–9. 60. Umbas R, Isaacs WB, Bringuier PP, Schaafsma HE, Karthaus HF, Oosterhof GO, et al. Decreased E-cadherin expression is associated with poor prognosis in patients with prostate cancer. Cancer Res 1994;54:3929–33. 61. Wozny W, Schroer K, Schwall GP, Poznanovic S, Stegmann W, Dietz K, et al. Differential radioactive quantification of protein abundance ratios between benign and malignant prostate tissues: cancer association of annexin A3. Proteomics 2007;7:313–22. 62. Gu Z, Thomas G, Yamashiro J, Shintaku IP, Dorey F, Raitano A, et al. Prostate stem cell antigen (PSCA) expression increases with high Gleason score, advanced stage and bone metastasis in prostate cancer. Oncogene 2000;19:1288–96. 12 63. Gu Z, Yamashiro J, Kono E, Reiter RE. Antiprostate stem cell antigen monoclonal antibody 1G8 induces cell death in vitro and inhibits tumor growth in vivo via a Fc-independent mechanism. Cancer Res 2005;65:9495–500. 64. Stephan C, Yousef GM, Scorilas A, Jung K, Jung M, Kristiansen G, et al. Hepsin is highly over expressed in and a new candidate for a prognostic indicator in prostate cancer. J Urol 2004;171:187–91. 65. Dhanasekaran SM, Barrette TR, Ghosh D, Shah R, Varambally S, Kurachi K, et al. Delineation of prognostic biomarkers in prostate cancer. Nature 2001;412:822–6. 66. Shariat SF, Andrews B, Kattan MW, Kim J, Wheeler TM, Slawin KM. Plasma levels of interleukin-6 and its soluble receptor are associated with prostate cancer progression and metastasis. Urology 2001;58:1008–15. 67. Nakashima J, Tachibana M, Horiguchi Y, Oya M, Ohigashi T, Asakura H, Murai M. Serum interleukin 6 as a prognostic factor in patients with prostate cancer. Clin Cancer Res 2000;6:2702–6. 68. Shariat SF, Kattan MW, Traxel E, Andrews B, Zhu K, Wheeler TM, Slawin KM. Association of pre-and postoperative plasma levels of transforming growth factor �1 and interleukin 6 and its soluble receptor with prostate cancer progression. Clin Cancer Res 2004;10:1992–9. 69. Hara N, Kasahara T, Kawasaki T, Bilim V, Obara K, Takahashi K, Tomita Y. Reverse transcription-polymerase chain reaction detection of prostatespecific antigen, prostate-specific membrane antigen, and prostate stem cell antigen in one milliliter of peripheral blood: value for the staging of prostate cancer. Clin Cancer Res 2002;8:1794–9. 70. Wang X, Yu J, Sreekumar A, Varambally S, Shen R, Giacherio D, et al. Autoantibody signatures in prostate cancer. N Engl J Med 2005;353:1224–35. 71. Taylor BS, Pal M, Yu J, Laxman B, Kalyana-Sundaram S, Zhao R, et al. Humoral response profiling reveals pathways to prostate cancer progression. Mol Cell Proteomics 2008;7:600–11. 72. Shariat SF, Walz J, Roehrborn CG, Zlotta AR, Perrotte P, Suardi N, et al. External validation of a biomarker-based preoperative nomogram predicts biochemical recurrence after radical prostatectomy. J Clin Oncol 2008;26:1526– 31. 73. Chun FK, Briganti A, Graefen M, Porter C, Montorsi F, Haese A, et al. Development and external validation of an extended repeat biopsy nomogram. J Urol 2007;177:510–5. 74. Karakiewicz PI, Hutterer GC. Predictive models and prostate cancer. Nat Clin Pract Urol 2008;5: 82–92. 75. Parekh DJ, Ankerst DP, Baillargeon J, Higgins B, Platz EA, Troyer D, et al. Assessment of 54 biomarkers for biopsy-detectable prostate cancer. Cancer Epidemiol Biomarkers Prev 2007;16: 1966–72. 76. Stephan C, Xu C, Finne P, Cammann H, Meyer HA, Lein M, et al. Comparison of two different artificial neural networks for prostate biopsy indication in two different patient populations. Urology 2007;70:596 –601. 77. Adam BL, Qu Y, Davis JW, Ward MD, Clements MA, Cazares LH, et al. Serum protein fingerprinting coupled with a pattern-matching algorithm distinguishes prostate cancer from benign prostate hyperplasia and healthy men. Cancer Res 2002;62:3609–14. 78. Petricoin EF III, Ornstein DK, Paweletz CP, Ardekani A, Hackett PS, Hitt BA, et al. Serum proteomic patterns for detection of prostate cancer. J Natl Cancer Inst 2002;94:1576 –8. 79. Qu Y, Adam BL, Yasui Y, Ward MD, Cazares LH, Schellhammer PF, et al. Boosted decision tree analysis of surface-enhanced laser desorption/ ionization mass spectral serum profiles discriminates prostate cancer from noncancer patients. Clin Chem 2002;48:1835–43. 80. Ornstein DK, Rayford W, Fusaro VA, Conrads TP, Ross SJ, Hitt BA, et al. Serum proteomic profiling can discriminate prostate cancer from benign prostates in men with total prostate specific antigen levels between 2.5 and 15.0 ng/ml. J Urol 2004;172:1302–5. 81. McLerran D, Grizzle WE, Feng Z, Thompson IM, Bigbee WL, Cazares LH, et al. SELDI-TOF MS whole serum proteomic profiling with IMAC surface does not reliably detect prostate cancer. Clin Chem 2008;54:53–60. 82. Diamandis EP. Mass spectrometry as a diagnostic and a cancer biomarker discovery tool: opportunities and potential limitations. Mol Cell Proteomics 2004;3:367–78.