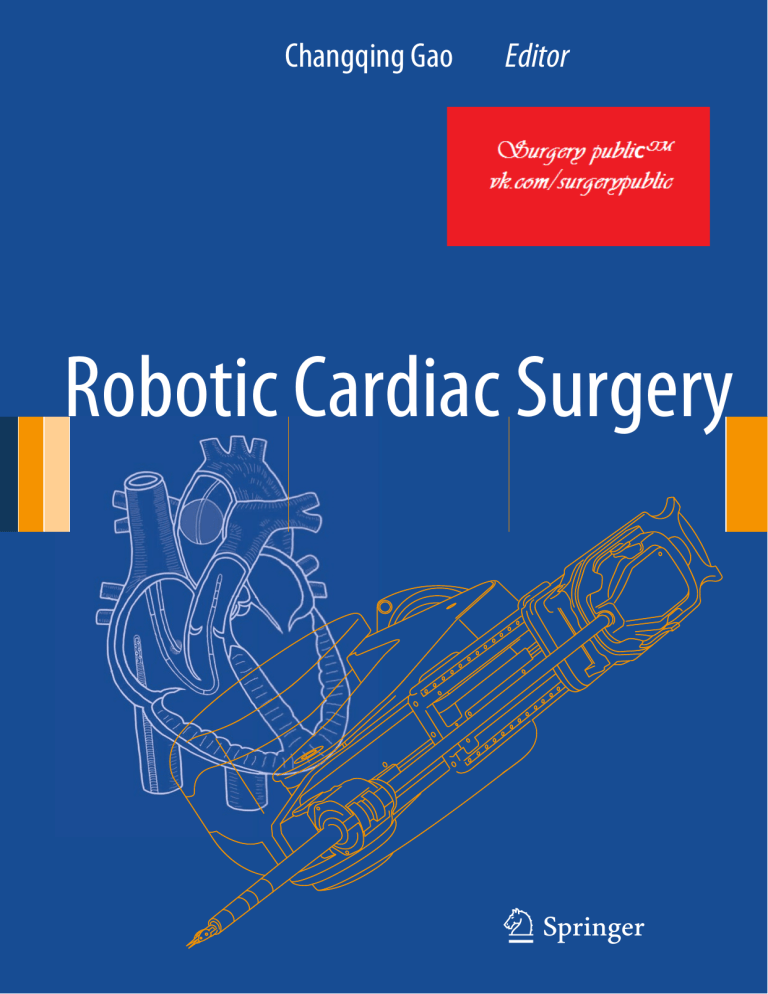
Changqing Gao Editor Robotic Cardiac Surgery 123 Robotic Cardiac Surgery Changqing Gao Editor Robotic Cardiac Surgery Editor Changqing Gao, MD Department of Cardiovascular Surgery PLA General Hospital Beijing Peoples’s Republic of China ISBN 978-94-007-7659-3 ISBN 978-94-007-7660-9 DOI 10.1007/978-94-007-7660-9 Springer Dordrecht Heidelberg New York London (eBook) Library of Congress Control Number: 2013954804 © Springer Science+Business Media Dordrecht 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifically for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provisions of the Copyright Law of the Publisher's location, in its current version, and permission for use must always be obtained from Springer. Permissions for use may be obtained through RightsLink at the Copyright Clearance Center. Violations are liable to prosecution under the respective Copyright Law. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. While the advice and information in this book are believed to be true and accurate at the date of publication, neither the authors nor the editors nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein. Printed on acid-free paper Springer is part of Springer Science+Business Media (www.springer.com) Foreword Robotic Cardiac Surgery is a comprehensive academic compilation of experience with robotic surgery in all phases of cardiac surgery as well as an extensively illustrated manual of how to do robotic cardiac surgery for several forms of acquired and congenital heart disease. The author, Dr. Changqing Gao, is an experienced robotic surgeon who has published much of his work in the peer-reviewed literature around the world and has held several excellent meetings and clinics to teach surgeons around the world how to do robotic cardiac surgery safely and effectively. One of the main principles illustrated in the book is in order to achieve excellent results utilizing robotic cardiac surgery you have to have excellent results in the conventional approach throughout all aspects of acquired and congenital heart surgery. It has been documented that experienced surgeons will become the leaders in the field of robotic cardiac surgery. Dr. Gao and his colleagues are very experienced surgeons, and their robotic surgery techniques and results are of the highest quality and are well documented in the pages of this book. Under acquired heart disease, primarily a robotic approach to mitral and tricuspid repair and replacement are discussed. The results of robotic surgical treatment for atrial septal defects and other smaller defects are outlined in the congenital section. The use of robotics for the take-down of the left internal mammary artery in performing CABG either by itself or with hybrid revascularization in conjunction with the placement of drug eluting or bare metal stents in other arteries is described in great detail. Hybrid revascularization stems from early work with minimally invasive valve surgery and single vessel lesions managed by a percutaneous coronary stent rather than a CABG and followed by a minimally invasive valve operation. This is now carried to the next step with robotic surgery performing a LIMA to the left anterior descending artery in combination with percutaneous coronary stents for some less important arterial obstructions. Again, the results are quite good and the techniques are extensively illustrated in this book. The last section is robotic left ventricular epicardial lead implantation, an area that may be helpful in the treatment of heart block or other arrhythmogenic entities that require cardiac rhythm therapy. All chapters are beautifully illustrated so as to enhance the reader’s understanding of robotic operations. Chapters in the book are primarily written by expert surgeons, anesthesiologists and cardiologists in China where this technology has had very good results. This book will be a landmark in presenting large clinical series results of conventional operations treated by robotic technology. Lawrence H. Cohn, MD Harvard Medical School v Preface Since robotic technology was introduced into the cardiac surgical field in 1998, the dream of cardiac surgeons to perform cardiac procedures in the closed chest has come true. With an outlook into the future, the PLA General Hospital took the lead to install the first da Vinci S Surgical System in China in 2006. The surgical team of the PLA General Hospital has started the cutting-edge techniques of minimally invasive robotic surgery in China. Our team had gone through tremendous trial investigations and hard work before they finally succeeded in using da Vinci S Surgical System in China. After working persistently with da Vinci S Surgical System for 7 years, we now can perform the whole range of closedchest heart procedures that da Vinci S Surgical System was designed for. Exceeding and renovating the desired techniques designed for the System, the surgeons of the team created new surgical techniques and standards, and completed the most types of robotic cardiac surgery on the globe. So far, the team has performed 700 cases all of which were successful. We were eager to share our experience with other surgical teams around the world. We established the National and International Training Center for Robotic Cardiac Surgery in Beijing, China. The center has provided training programs for groups of cardiac surgical professionals from other countries and regions like Japan, Singapore, Brazil, Korea, Hong Kong and Taiwan. Advances in robotic heart surgery in China have exerted far-reaching impacts in Asia and even around the world. China has a tremendous patient base and a large pool of talented and innovative surgeons with extensive surgical experience. For sure, the full potential of da Vinci surgery will be realized through the increased exchanges between Chinese surgeons and their counterparts around the world. We have written this book to record the landmark, to share our experience and to acknowledge the care and help given by our mentors and colleagues from all parts of the world. Beijing, People’s Republic of China Changqing Gao, MD vii Biography Dr. Changqing Gao is currently the Vice President of the PLA General Hospital, the Chairman and Professor of the Department of Cardiovascular Surgery, Director of the Institute of Cardiac Surgery, the National Training Center for Robotic Cardiac Surgery, International Training Center for da Vinci Surgery, and International Cooperation and Research Center for Robotic Cardiac Surgery. Dr. Gao has performed over 4,000 cases of cardiovascular surgery and has become a nationrenowned expert in the surgical field. His professional interests include acquired heart disease, mitral and aortic valve repair/replacement, and aneurysms of the thoracic aorta. He has a special interest in complex coronary artery bypass, off-pump coronary artery bypass, left ventricular aneurysms, and minimally invasive cardiac surgery. Dr. Gao is a pioneering surgeon in robotic cardiac surgery in Asia. He has completed 700 cases of robotic cardiac surgery with da Vinci Surgical Systems since 2007. He has been a recipient of many research grants and fellowship, and numerous awards for his excellence and achievements in science and technology. He is currently the principal investigator in a number of major clinical research projects in China. Dr. Gao is the Executive Councilor of the Asian Society for Cardiovascular and Thoracic Surgery (ASCVTS), Board of Director of ISMICS and the Minimally Invasive Robotic Association (MIRA), Charter member of the Society of Robotic Surgery (SRS), Member of AATS, STS and EACTS, Councilor of the Chinese Medical Association, Vice President and Secretary General of the Chinese Society of Thoracic and Cardiovascular Surgery, Vice President of the Chinese Association of Cardiovascular Surgeons, President of the Beijing Society of Cardiac Surgery, and Executive Councilor of the Beijing Medical Association. ix x Dr. Gao is the Co-editor of the Journal of Robotic Surgery of USA, Board member of the Heart Surgery Forum, Board member of Innovations, Associate Editor-in-chief of the Journal of Thoracic and Cardiovascular Surgery, Editor-in-chief of the Chinese Journal of Extracorporeal Circulation, and Associate Editor-in-chief of the Chinese Journal of Thoracic and Cardiovascular Surgery. He also holds membership of the editorial boards of many influential medical journals. Biography Acknowledgement The authors gratefully acknowledge the assistance of the following individuals and organizations whose contributions made publication of this book possible: PLA General Hospital, PLA Medical School, Beijing, China Karen Zhao, MA Junlan Yan, RN Jiali Wang, BS Jiachun Li, BS Guopeng Liu, MS Yue Zhao, RN Lixia Li, RN Bojun Li, MD Shengli Jiang, MD Rong Rong, MD xi Contents 1 Overview of Robotic Cardiac Surgery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Changqing Gao 1 2 Anesthesia for Robotic Cardiac Surgery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Gang Wang and Changqing Gao 15 3 Intraoperative Transesophageal Echocardiography in Robotic Cardiac Surgery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Yao Wang and Changqing Gao 33 Peripheral Cardiopulmonary Bypass Establishment for Robotic Cardiac Surgery. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Cangsong Xiao and Changqing Gao 49 4 5 Robotic Surgery in Congenital Heart Diseases . . . . . . . . . . . . . . . . . . . . . . . . . . . Changqing Gao and Ming Yang 61 6 Totally Robotic Myxoma Excision . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Changqing Gao and Ming Yang 83 7 Robotic Mitral Valve Surgery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Changqing Gao and Ming Yang 93 8 Robotic Coronary Bypass Graft on Beating Heart. . . . . . . . . . . . . . . . . . . . . . . . 111 Changqing Gao and Ming Yang 9 Hybrid Coronary Revascularization . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 135 Mukta C. Srivastava, Bradley Taylor, David Zimrin, and Mark R. Vesely 10 Robotic Left Ventricular Epicardial Lead Implantation . . . . . . . . . . . . . . . . . . . 141 Changqing Gao, Chunlei Ren, and Ming Yang Index . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 147 xiii Contributors Changqing Gao, MD Department of Cardiovascular Surgery, PLA General Hospital, Beijing, People’s Republic of China Chunlei Ren Department of Cardiovascular Surgery, PLA General Hospital, Beijing, People’s Republic of China Mukta C. Srivastava, MD Division of Cardiology, University of Maryland Medical Center, Baltimore, MD, USA Bradley Taylor, MD Division of Cardiology, University of Maryland Medical Center, Baltimore, MD, USA Mark R. Vesely, MD Division of Cardiology, University of Maryland Medical Center, Baltimore, MD, USA Gang Wang, MD Department of Cardiovascular Surgery, PLA General Hospital, Beijing, People’s Republic of China Yao Wang, MD Department of Cardiovascular Surgery, PLA General Hospital, Beijing, People’s Republic of China Cangsong Xiao, MD Department of Cardiovascular Surgery, PLA General Hospital, Beijing, People’s Republic of China Ming Yang, MD Department of Cardiovascular Surgery, PLA General Hospital, Beijing, People’s Republic of China David Zimrin, MD Department of Medicine, University of Maryland School of Medicine, Baltimore, MD, USA xv 1 Overview of Robotic Cardiac Surgery Changqing Gao Abstract It has been the dream of cardiac surgeons to perform cardiac procedures in the closed chest that would offer patients the same benefits as those that open-incision procedures do. The revolutionary minimally invasive surgery has certainly satisfied some of the desires of cardiac surgeons but they have never been as satisfactory as what cardiac surgical robots can ever have been. Minimally invasive cardiac surgery has grown in popularity over the past two decades. And minimally invasive videoscope has been the most used approach. Minimally invasive techniques can provide patients with more advantages in recovery process than open procedures. The 2-D camera of endoscope causes impaired visualization, absence of the depth of the surgical field, and difficulty for complete precise manipulation by surgeons. The drive for robotic surgery is rooted in the desire to overcome the shortcomings of endoscopic surgery and expand the benefits. Robotic technology was introduced into the cardiac surgical field in 1998. AESOP (Automated Endoscopic System for Optimal Positioning) and ZEUS, two surgical robotic systems, were approved by the FDA for clinical use in 1994 and 2001 respectively. In January 1999, Intuitive launched the da Vinci Surgical System, and in 2000, it became the first robotic surgical system cleared by the FDA for general laparoscopic surgery. In the following years, the FDA cleared the da Vinci Surgical System for cardiac procedures. The robotic technique has been successfully used in atrial septal defect repair on arrest or beating heart, mitral valve repair or replacement, coronary bypass graft, myxomas resection, atrial fibrillation ablation, left ventricular epicardial lead placemen and aortic surgery. Early results are encouraging with evidence that patients experience little blood transfusion, shorter hospital stay, sooner return to preoperative function levels and improve quality of life with robotic surgery than with sternotomy. However, long-term results are needed to determine if robotic techniques could become the new standards in cardiac surgery. While conventional video endoscopic techniques were revolutionary in their own right, they were hampered by limited instrument maneuverability and 2-D visualization. These technological shortcomings took away the wrist-like motion of the human hand and the depth perception of human C. Gao, MD Department of Cardiovascular Surgery, PLA General Hospital, No. 28 Fuxing Road, Beijing 100853, People’s Republic of China e-mail: gaochq301@yahoo.com eyes, and necessitated the design of new procedures which were adapted to the technology. Robotics represents yet another revolution in the application of minimally invasive techniques to surgery. Robotics by virtue of wrist-like instrument maneuverability and 3-D visualization has returned the advantages of the human wrist and eyes to the field of minimally invasive surgery. For the first time in the history of minimally invasive surgery, operations which were designed to be performed by open incisions can be replicated using minimal access C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_1, © Springer Science+Business Media Dordrecht 2014 1 2 C. Gao techniques today. Actually, robotic cardiac surgery became feasible in the late 1990s of the last century. Over the last 10 years, robotic surgery has been increasingly recognized by surgeons throughout the world. In fact, da Vinci Surgical System has brought about a real revolution in many surgical fields. In China, da Vinci surgery has been enthusiastically embraced by surgeons and robotic cardiac surgery is developing particularly fast. In 2007, the da Vinci S was first introduced to China, at the PLA General Hospital (301), where the first robotic cardiac surgery in China was performed. Since then, over 640 cases of robotic cardiac surgery have been performed at the Cardiovascular Surgery Department, such as totally endoscopic coronary artery bypass on beating heart, minimally invasive direct coronary artery bypass grafting on beating heart, hybrid coronary revascularization, mitral valve repair, mitral valve replacement, tricuspid repair, myxoma resection, atrial septal defect repair, ventricular septal defect repair, left ventricular lead implantation, and so on. And the surgical results are excellent as expected. Our experience shows that with a well-trained robotic team and after a substantial learning curve, surgeons could achieve optimal outcomes in robotic surgeries, and continued development of expertise, technical skills and vigilance of long term outcomes will prepare surgeons for future advancements. We have to emphasize that the da Vinci Surgical System is a surgical tool, and the kind of surgical procedures the surgeon can perform depends on surgeon’s own experience, not on da Vinci! China has an enormous patient base and a large pool of talented and innovative surgeons with extensive surgical experience. For sure, the full potential of da Vinci surgery will be realized through increased exchanges between Chinese surgeons and their counterparts in other countries. 1.1 History of Minimally Invasive Surgery Minimally invasive surgeries are procedures that avoid use of open invasive procedures for the same purpose in favor of closed or local surgery, and are carried out through the skin or through a body cavity or anatomical opening. These procedures generally involve use of laparoscopic devices and remote-control manipulation of instruments with indirect observation of the surgical field through an endoscope or similar device [1]. As the most representative procedures of minimally invasive surgery, laparoscopic surgery was initiated from cholecystectomy, and was first reported in Germany (1985) and France (1987) more than two decades ago [2–5]. In contrast to open procedures, advantages to patients with laparoscopic surgery include reduced hemorrhage, smaller incision, less pain, reduced risks of infections, shortened hospital stay and faster return to everyday living. Although these advantages seem attractive, technical and mechanical natures of the current laparoscopic equipment determine the inherent limitations of laparoscopic surgery, such as fulcrum effect, limited degrees of motion (4 degrees of freedom), loss of haptic feedback (force and tactile), counterintuitive visual feedback, and compromised dexterity. The desire to overcome these limitations motivated engineers and researchers to develop surgical robots while expanding the benefits of minimally invasive surgery. A robot is a mechanical or virtual intelligent agent that can perform tasks automatically or with guidance, typically by remote control. The attempts to create artificial machines and automata have a history of more than 2,000 years. Derived from Slavic term Robota, meaning “forced labor, chore,” the term robot was coined in 1920 and introduced to the public by the Czech writer Karel Čapek in his play R.U.R. (Rossum’s Universal Robots) [6]. Since then, robots evolved throughout the twentieth Century, and entered realms such as industry, military, aerospace, marine navigation, etc. It was a landmark in 1961 when the first industrial robot was online in a General Motors automobile factory in New Jersey (Rover Ranch, 2005), which announced the entrance of robots to mainstream human life. 1.2 History of Robotic Systems Computer-enhanced instruments have been developed to provide telemanipulation and micromanipulation of tissues with 6 degrees of freedom to allow free orientation in confined spaces. The use of a robot-assisted surgical procedure was first documented in 1985, and PUMA 560 was used by Kwoh et al. to perform neurosurgical biopsies with CT guidance [7]. The same system was used for soft-tissue surgery 3 years later, in the transurethral resection of the prostate (TURP) for benign prostatic hyperplasia [8]. In 1988, the PROBOT, developed at Imperial College London, was used to perform prostatic surgery by Dr. Senthil Nathan at Guy’s and St Thomas’ Hospital, London. Simultaneously, RoboDoc, the first surgical robotic system was developed by the Integrated Surgical Supplies Ltd. of Sacramento, CA. RoboDoc was used to perform total hip replacements in 1992 [9] with confirmed ability to precisely core out the femoral shaft with 96 % precision, whereas a standard hand broach provided only 75 % accuracy [10]. Despite its failure to receive FDA approval, RoboDoc found extensive applications in Europe and Japan. 1 Overview of Robotic Cardiac Surgery 3 Computer Motion, Inc.®, a medical robotics company was founded in 1989 by Yulun Wang, PhD, an electrical engineering graduate of the University of California, Santa Barbara with funding from the U.S. government and private industry. Computer Motion, Inc.® launched AESOP® (Automated Endoscopic System for Optimal Positioning), a robotic telescope manipulator, and the robotic surgical system ZEUS® [11, 12]. The two robotic systems were approved by the FDA for clinical use in 1994 and 2001 respectively [12] (Figs. 1.1 and 1.2). 1.3 Fig. 1.1 The AESOP surgical system a Fig. 1.2 The Zeus surgical system The da Vinci Surgical System Frederic H. Moll, MD, a physician with a keen business sense saw the commercial value of the emerging robotic technology, acquired the license to the robotic surgical system pioneered by the NASA-SRI team, and started a company called Intuitive Surgical Inc.® in 1995. In January 1999, Intuitive launched the da Vinci Surgical System, which in 2000 became the first robotic surgical system accredited by the FDA for general laparoscopic surgery. In the following years, the FDA accredited the da Vinci Surgical System for thoracoscopic surgery, cardiac procedures performed with adjunctive incisions, urologic, gynecologic, pediatric and transoral otolaryngology procedures. The Intuitive Surgical Inc.® merged with Computer Motion, Inc.® in June of 2003, strengthening its intellectual property holdings [13]. b 4 C. Gao Fig. 1.3 The dual consoles of da Vinci Si at PLA General Hospital The da Vinci Surgical System consists of three components: (1) surgical console, (2) patient cart, and (3) vision cart (Figs. 1.3, 1.4, and 1.5). The system provides the following advantages to the surgeons: three-dimension visualization, control of endoscopic instrument, and control of the camera. It enables direct real-time movement of endoscopic instrument by the operating surgeons and allows the surgeons to use techniques of open surgery during endoscopic procedures. The surgeon console is physically removed from the patient and allows the surgeon to sit comfortably (Fig. 1.6), resting the arms ergonomically while immersing himself/herself in the three-dimensional high-definition videoscopic image with the depth of the field through the view port. The surgeon controls the micro-instruments using the master controller. The medical signal, such as, ECG, oxygen saturation, and cardiac echo can be seen through stereo viewer in the surgical field (Fig. 1.7). Furthermore, various messages are displayed on the stereo viewer using icons and text. These enable the surgeon to monitor the status of the instruments and the arms without removing his/her head from the console. Fig. 1.4 Patient cart The master controllers are used by the surgeon to control the instruments, the instruments arms, and the camera. The foot switches consists of instrument clutch, camera control clutch, camera focus, and electrocautery control. The armrest switches on the left and right armrests are used to control the motion and scaling of the robotic arms. And they are replaced by a touch screen panel in da Vinci Si Surgical System (Figs. 1.8 and 1.9). Wrist and finger movements are digitally registered in computer memory, and then transferred to the instrument cart, where the synchronous end-effectors or micro instruments provide tremor-free movements with 7 degrees of freedom (Fig. 1.10). The instrument cart holds three arms in the first version (da Vinci®) and four arms in more recent models (da Vinci S® and da Vinci Si®) (Fig. 1.11). One arm supports the dual 5-mm diameter cameras to generate 3-D 1 Overview of Robotic Cardiac Surgery 5 Fig. 1.5 Vision cart Fig. 1.7 The medical signal can be seen through the stereo viewer during the surgery Fig. 1.6 The surgeon sits at the console at PLA General Hospital image and the other two or three arms are for wrist-like articulations equipped with EndoWrist Instruments that are designed to provide surgeons with natural dexterity and full range of motion. 6 C. Gao Fig. 1.8 The surgeon console and its components of da Vinci S Surgical System The patient cart that rolls on wheels, is moved into the operative field, and is positioned over the patient. The robotic arms are designed like the human arm with a shoulder, an elbow, and a wrist. The instruments are attached to a carriage on the robotic arm. The carriage moves the instrument in and out a cannula at the tip of the arm. The cannula acts as the port that is introduced into the patient and carries the robotic instruments. The patient cart is connected with cables to the surgeon console. The vision cart consists of the left eye camera control unit, right eye camera control unit, light source, video synchronizer and focus controller, assistant monitor, and various recordings and insufflation devices specific to the surgical application. Using the most advanced technology available today, the da Vinci Surgical System enables surgeons to perform Fig. 1.9 A touch screen panel in da Vinci Si Surgical System replaces the traditional buttons at PLA General Hospital 1 Overview of Robotic Cardiac Surgery 7 Fig. 1.11 The four arms of da Vinci Si Surgical System docked at PLA General Hospital Fig. 1.10 The “wrist” instrument provides the natural dexterity and full range of motion delicate and complex operations through a few tiny incisions with an increased vision, precision, dexterity and control. 1.4 Operating Room Configuration and System Setup The da Vinci Surgical System consists of three main components: the Surgeon Console, the Patient Cart and the Vision Cart. The components should be arranged well in the operating room for maximum safety and ergonomic benefit (Fig. 1.12). The Surgeon Console is placed outside of the sterile field and is oriented where the Surgeon Console operator will have a view of the operative field and a clear line of communication with the Patient Cart operator (Fig. 1.12). The Patient Cart is draped prior to moving into place for surgery. The draped arms should be covered by an additional sterile coat (Fig. 1.13) to prevent coming into contact with non-sterile objects or impede traffic. Once the Patient Cart is draped, and the patient is positioned, prepared, draped and ports are placed, use the Patient Cart motor drive to help move the cart into the sterile field. The Vision Cart is placed adjacent to the Patient Cart, just outside of the sterile field, to allow the Patient Cart Operator to see the component displays (Fig. 1.14). The Vision Cart should be close enough to the Patient Cart to allow unrestricted camera cable movement during surgery. The components of da Vinci Surgical System are connected by three main cables. The three cables can be distinguished by their diameter and color. The cables should be arranged so that they are out of the path of OR traffic, including other equipment, to avoid damaging the cables or creating an obstacle or hazard. Usually, a two-person team is assigned to handle nonsterile components: a scrub nurse and a circulating nurse drape the arms. The arms are draped systematically, allowing movement from left to right or right to left. Using the clutch buttons, the circulating nurse should move each straightened arm to provide plenty of room to maneuver around the arm. Once an arm is draped, the scrub nurse should move the draped arm away from the undraped arms and prepare to drape the next arm. The preoperative management is critical to the success of robotic heart surgery. The patient should be positioned 8 C. Gao Fig. 1.12 The components of da Vinci Surgical System are arranged in the OR for clear communication at PLA General Hospital Fig. 1.13 The draped arms are covered by an additional sterile coat to avoid contamination prior to docking the da Vinci Surgical system. The operating table should be easily moved prior to driving the Patient Cart into position. For robotic-assistant cardiac surgery, there are two opposite approaching routs, the left and the right chest walls. The surgical side of the patient’s chest is elevated at approximately 30° and with the arm tucked at the side (Figs. 1.15 and 1.16). Port placement is the key to a successful da Vinci procedure. The goals of port placement are to avoid Patient Cart arms collisions and maximize the range of motion for instruments and endoscope. The improper port placement may cause serious injury to the patient. Examples of port placement recommendations for cardiac surgery are provided in Figs. 1.6 and 1.7. Initial port location should be selected giving consideration to the procedure, specific anatomy, and the type of components being used. 1 Overview of Robotic Cardiac Surgery 9 Fig. 1.14 The Vision Cart is placed adjacent to the Patient Cart, to allow the Patient Cart Operator to see the component displays at PLA General Hospital Fig. 1.16 The patient position for left approach of da Vinci cardiac surgery with left side of the chest elevated at 30° and with the left arm tucked at the side Fig. 1.15 The patient position for right approach of da Vinci cardiac surgery with right side of the chest elevated at 30° and with the right arm tucked at the side Placement of the right ports: a 12-mm endoscopic trocar is placed into the right thoracic cavity through the incision made at 2–3 cm lateral to the nipple in the fourth intercostal space (ICS). A 1.5-cm incision is used as a working port in the same ICS for the patient-side surgeon. Additionally two 8-mm port incisions are made in the second and sixth ICS to allow insertion of the left and right instrument arms. The right instrument arm generally is positioned 4–6 cm lateral to the working port in the sixth ICS. The fourth arm trocar is placed in the midclavicular line in the 4th or 5th ICS (Fig. 1.17). Placement of the left ports: Three trocars were placed in the 3rd, 5th and 7th intercostal spaces that located about 3 cm lateral of the midclavicular line (Fig. 1.18). Docking is the process of moving the Patient Cart up to the OR table and connecting the Patient Cart arms to the patient. Once the cannulas are inserted in the patient, the 10 C. Gao Fig. 1.17 Recommendatory ports placement for right approach of da Vinci cardiac surgery Fig. 1.19 The Patient Cart is moved into the sterile field Fig. 1.18 Recommendatory ports placement for robotic coronary artery bypass graft Patient Cart motor is moved into the sterile field (Fig. 1.19). Communication is critical when docking the Patient Cart. Use the instrument arm or camera port clutch button to bring the cannula mount to the cannula. If there are two instrument arms on one side, ensure that the instrument arm closest to the camera arm has adequate range of motion while minimizing collisions (Fig. 1.20). 1.5 Robotic Cardiac Surgery Cardiac surgery has been conventionally performed via median sternotomy for the convenience of adequate exposure and surgeons’ generous access to the heart and surrounding vessels. Since the notion of minimally invasive Fig. 1.20 Instrument arm closest to the camera arm has adequate range of motion surgery was introduced to cardiovascular surgery, surgeons are keen on developing less invasive methods without any compromise on accessibility and dexterity thus resulting in paradigm shift in cardiac surgery. With the application of surgical robotic systems, surgeons are enabled to improve dexterity and perform ambidextrous sutures in the limited space. The procedures have hitherto been successfully performed such as mitral valve reconstruction and replacement, coronary revascularization, atrial fibrillation surgery, left ventricular lead placement, intra-cardiac tumor resection, congenital surgery, etc. 1 Overview of Robotic Cardiac Surgery 1.5.1 Robotic Mitral Valve Surgery The Intuitive surgical system was originally designed for cardiovascular surgery, of which the first clinical application in human was performed by Carpentier on May 7, 1998, to repair an atrial septal defect by mini-thoracotomy. And he subsequently performed the first truly endoscopic mitral valve repair by an early prototype of da Vinci in the same year [14]. Such pioneering work was soon followed by a series of totally robotic cardiovascular surgery, announcing a vitally important innovation which might later be a thorough revolution in cardiovascular surgery. The first complete mitral valve repair using da Vinci system was performed by Chitwood in May 2002 that encouraged initial attempts phase I [15] and phase II [16] US Food and Drug Administration (FDA) trials which subsequently led to the approval of the da Vinci system for mitral valve surgery in November 2002. At specialized medical centers, totally robotic mitral valve repair has become a standardized procedure. Surgeons perform conventional mitral valve repair techniques such as quadrangular leaflet resections, leaflet sliding-plasties, edge-to-edge approximations, chordal transfers, polytetrafluoroethylene neochordal replacement, reduction annuloplasties, and annuloplasty band insertions. The transthoracic Chitwood clamp (Scanlan International, Minneapolis, Minnesota, USA) is applied across the ascending aorta, as substitution for endoaortic occlusion balloon yielding decreased morbidity, total operative and cross-clamp times and cost [17], as well as less common aortic dissections [18]. The novel EndoWrist atrial retractor (Intuitive Surgical Inc) manipulated by a four-arm da Vinci Surgical System (Intuitive Surgical Inc, Sunnyvale, CA) allows dynamic exposure of the valve structures and minimized aortic valve distortion, resulting in more efficient antegrade cardioplegia delivery and reduced air entry in the aortic root [19]. The introduction of the above-mentioned newer robotic instrumentation facilitated robotic mitral repair. Furthermore, simpler repair techniques such as the ‘American correction’ [20], the ‘haircut posterior leafletplasty’ [21], premeasured artificial neochordea [22], and the running annuloplasty suture technique [23] facilitated complex procedures which result in shorter operative times and excellent outcomes. Since technology and techniques keep improving, it is likely that more reproducible and preferable results will be achieved. 1.5.2 Robotic Coronary Revascularization The da Vinci system found its first clinical application for coronary surgery in May 1998 by Mohr who harvested the left internal mammary artery (LIMA) as bypass graft for 11 hand-sewn anastomosis through a small left thoracotomy [24]. The scope of robot-assisted coronary operations has hitherto ranged from internal mammary artery (IMA) harvest with a hand-sewn anastomosis, performed on pump through a median sternotomy or mini-thoracotomy (minimally invasive direct coronary artery bypass (MIDCAB)), to multivessel off-pump totally endoscopic coronary bypass (TECAB). In 1998, Loulmet et al. were the first to report a completely endoscopic LIMA to left anterior descending artery (LAD) coronary bypass procedure [25]. Since most patients who are apt to undergo coronary artery bypass surgery have multivessel diseases, the development of endoscopic multiple bypass grafting is mandatory. Thus further development in technology and surgical techniques have been prompted by patients’ needs to facilitate the progression from single-vessel LIMA to LAD to recently quadruplevessel bypass on beating heart TECAB [26] and triple-vessel bypass on arrested heart TECAB [27]. Multivessel revascularization graft configurations can include combinations of single, sequential, T, or Y grafts, generally based on one or both IMAs [28] and can be combined with percutaneous coronary interventions, which is termed as hybrid coronary revascularization. Besides ever advancing anastomotic techniques, novel suture technologies such as self-closing surgical nitinol microclips termed U-Clip (Coalescent Surgical, Sunnydale, CA, USA), endoscopic stabilizer (Intuitive Surgical, USA) and target vessel identification systems will likewise facilitate TECAB procedures. 1.5.3 Robotic Congenital Surgery Totally endoscopic close-chest congenital surgery can be achieved through several 8–15-mm microincisions on the right thoracic wall. This procedure benefits from the ever rapidly advancing robotic technology. Torracca et al. were the first to report a small cohort of patients undergoing robotic atrial septal defect (ASD) repair in Europe [29]. Argenziano et al. demonstrated that ASDs in adults could be closed safely and effectively using totally endoscopic robotic approaches with a median cross-clamp time of 32 min in 2003 [30], and robotic ASD repair subsequently gained its FDA approval. Although patent ductus arteriosus closure and vascular ring repair have also been successfully completed robotically [31], ASD repairs remain the most common totally robotic congenital surgery. Till June 2012, the authors’ team have completed a series of 130 ostium secundum ASD repairs, of which 76 cases were completed on beating heart. Besides atrial septal defect repair on beating heart [32], we have further initiated robotic congenital surgical procedures such as atrial septal defect repair plus tricuspid valve repair on beating heart, partial anomalous pulmonary venous con- 12 C. Gao nection correction, ventricular septal defect repair [33] and ostium primum defect repair. The feasibility and effectiveness of robotic congenital surgery have been proved and the optimal results encouraged our team to extend the use of this technology to patients with more complicated congenital heart diseases. 1.5.4 Atrial Fibrillation Surgery Various energy sources have been introduced to simplify the traditional ‘cut and sew’ approach to allow development of less invasive therapies for atrial fibrillation. Full Cox-Maze III right and left lesion sets can be made with robotic assistance as an excellent alternate technology. Lesions can be significantly visualized to minimize the risks of gaps and bleeding, which may result in failures. Rodriguez E et al. described their experience of resecting the right-sided lesions on CPB while left-sided lesions were treated after opening the left atrium, and reported their cryolesion set in 2009 [36]. 1.5.6 Aortic Valve Surgery Experience with robotic aortic valve surgery is limited to a few case reports [39] with only some steps of the procedure performed robotically. In March 2010, the first in-human robot-assisted endoscopic aortic valve replacement was reported to be performed by Balkhy H. [40]. The reproducibility remains to be confirmed by more clinical trials. Robotic Intracardiac Tumor Resection Intracardiac tumors generally require active treatment by surgical resection to prevent thromboembolic complications, although they are uncommon and mostly benign. Resection can be achieved through either a left atriotomy or right atriotomy, with trans-septal approach if necessary, autologous pericardial patches can be used to repair septal defects following excision. The author and colleagues reported the currently largest series of consecutive patients with atrial myxoma undergoing robotic excision. Resection was achieved in all patients without surgical mortality or stroke. Follow-up echocardiograms up noted no recurrence or atrial septal defect [34]. Similarly, Woo et al. described successful excision of an aortic valve papillary fibroelastoma [35]. 1.5.5 1.5.7 Left Ventricular Epicardial Lead Implantation Implantation of the left ventricular lead is usually performed percutaneously via coronary sinus cannulation, advancing the lead into a major cardiac vein. This technique is associated with long fluoroscopy times and is limited by coronary venous anatomy. Early reports by DeRose et al. demonstrated the efficacy of robot-assisted LV lead implantation without complications or technical failures [37]. Though larger series of similar procedures have been reported [38], randomized studies comparing minimally invasive surgical approach with conventionally transvenous implantation is in progress. 1.6 Summary & Perspective Surgical robotics is a state-of-the-art technology that holds significant promises. As iteration toward a less-invasive surgical tool, robots allow surgeons to perform sophisticated cardiac surgical procedures that are otherwise limited only to conventionally median sternotomy. Surgical robots well demonstrate their unquestionable benefits over conventionally open surgery in items of decreased hospitalization time, lowered complication rates, reduced postoperative pain, improved cosmetic results, and faster return to normal daily activities. Furthermore, they overcome many of the obstacles of thoracoscopic surgery as they improve visualization with 3-D visioning in high definition, in-depth perception and up to 10× magnification, eliminate the fulcrum effect while restore more intuitive hand-eye coordination, increase maneuverability through elimination of physiological tremors and ability to scale motions, and moreover, ergonomically friendly design for stable and untiring surgical performance. Analogous to thoracoscopy, robotic systems are not yet available for spectrum of cardiac diseases as broad as surgeries through conventional thoracotomy. Contraindications are as follows. Optimal port location can occasionally be difficult in the presence of abnormal thoracic anatomy or cardiac dislocation. Patients with severe pleural adhesions secondary to prior thoracotomy or pleuritis may have higher potential of injury by introducing trocars and working with endoscopic instruments. Patients with severe peripheral artery diseases should be excluded for unfitness to perform femoro-femoral cardiopulmonary bypass. Furthermore, creation of pneumothorax by insufflating CO2 can lead to hemodynamic impairment. Thus patients who have poor cardiac functions and poor tolerance of high intrathoracic pressures may not be the ideal candidates. In respect to the ever-advancing surgical robotic systems, with a price tag of several million dollars, their costs seem prohibitive, let alone the costs of maintenance and upgrading. Thus robotic cardiac surgeries are confined to some specialized centers though the number is expanding. Absence of haptic sensation and consequent loss of tactile feedback impair the manipulation of tissue as well as suturing material, which may be the most technical obstacle for surgeons 1 Overview of Robotic Cardiac Surgery to perform delicate suturing because of their inability to judge qualitatively. Lack of more compatible instruments for retraction, exposure and visioning increases the reliance on tableside assistance to perform certain part of the surgery such as knotting, retracting, replacing instruments, etc. Driven by the market as well as patient demands, an increasing number of centers compete to acquire and incorporate this advanced technology though considerable centers currently lack practical experience. To such centers, critical and objective evaluations are requisite for informed decision before hopping on the “robotic bandwagon” in haste, since surgical robot is only one of many tools that are prerequisite for successful cardiovascular surgery. Hitherto, there has been a paucity of data regarding longterm follow-up studies which are actually in urgent need to determine whether robotic techniques could become new standards in cardiovascular surgery. Much remains to be done before full potential of robotic cardiac surgery can be realized. Nevertheless, current disadvantages and obstacles will undoubtedly be remedied with time and improvement in both techniques and technology. Robotic surgery, of which the emergence and advancement embodies the humanistic evolution of medical science and technology, is often heralded as part of a natural and logical evolution of minimally invasive surgery. Since we are simply at one point on a continuum and robotic technologies as well as surgical techniques are progressing stepwise, the future of robotic cardiac surgery is limited only by imagination. References 1. Vernick W, Atluri P. Robotic and minimally invasive cardiac surgery. Anesthesiol Clin. 2013;31(2):299–320. 2. Reynolds Jr W. The first laparoscopic cholecystectomy. JSLS. 2001;5(1):89–94. 3. Mouret P. Celioscopic surgery. Evolution or revolution. Chirurgie. 1990;116(10):829–32. 4. Cuschieri A, Dubois F, Mouiel J, et al. The European experience with laparoscopic cholecystectomy. Am J Surg. 1991;161(3): 385–7. 5. Delaitre B, Testas P, Dubois F. Complications of cholecystectomy by laparoscopic approach. Apropos of 6512 cases. Chirurgie. 1992;118(1–2):92–9. 6. Nocks L. The robot: the life story of a technology. Westport: Greenwood Press; 2007. 7. Kwoh YS, Hou J, Jonckheere EA, Hayall S. A robot with improved absolute positioning accuracy for CT guided stereotactic brain surgery. IEEE Trans Biomed Eng. 1988;35(2):153–61. 8. Davies BL, Hibberd RD, Coptcoat MJ, Wickham JEA. A surgeon robot prostatectomy – a laboratory evaluation. J Med Eng Technol. 1989;13(6):273–7. 9. Cowley G. Introducing “Robodoc”. A robot finds his calling – in the operating room. Newsweek. 1992;120(21):86. 10. Satava RM. Surgical robotics: the early chronicles: a personal historical perspective. Surg Laparosc Endosc Percutan Tech. 2002;12: 6–16. 13 11. Marescaux J, Rubino F. The ZEUS robotic system: experimental and clinical applications. Surg Clin North Am. 2003;83(6):1305–15. 12. Satava RM. Robotic surgery: from past to future – a personal journey. Surg Clin North Am. 2003;83(6):1491–500. 13. Kypson AP, Chitwood WR. Robotic application in cardiac surgery. Int J Adv Robot Syst. 2003;1(2):87–92. 14. Carpentier A, Loulmet D, Aupecle B, et al. Computer assisted open heart surgery. First case operated on with success. C R Acad Sci III. 1998;321(5):437–42. 15. Nifong LW, Chu VF, Bailey BM, Maziarz DM, Sorrell VL, Holbert D, Chitwood Jr WR. Robotic mitral valve repair: experience with the da Vinci system. Ann Thorac Surg. 2003;75:438–42; discussion 43. 16. Nifong LW, Chitwood WR, Pappas PS, Smith CR, Argenziano M, Starnes VA, Shah PM. Robotic mitral valve surgery: a United States multicenter trial. J Thorac Cardiovasc Surg. 2005;129:1395–404. 17. Reichenspurner H, Detter C, Deuse T, et al. Video and roboticassisted minimally invasive mitral valve surgery: a comparison of the Port-Access and transthoracic clamp techniques. Ann Thorac Surg. 2005;79:485–90. 18. Jones B, Krueger S, Howell D, et al. Robotic mitral valve repair: a community hospital experience. Tex Heart Inst J. 2005;32:143–6. 19. Smith JM, Stein H, Engel AM, et al. Totally endoscopic mitral valve repair using a robotic-controlled atrial retractor. Ann Thorac Surg. 2007;84:633–7. 20. Lawrie G. Mitral valve: toward complete repairability. Surg Technol Int. 2006;15:189–97. 21. Chu M, Gersch K, Rodriguez E, et al. Robotic ‘haircut’ mitral valve repair: posterior leaflet-plasty. Ann Thorac Surg. 2008;85:1460–2. 22. Smith JM, Stein H. Endoscopic placement of multiple artificial chordae with robotic assistance and nitinol clip fixation. J Thorac Cardiovasc Surg. 2008;135:610–14. 23. Mihaljevic T, Jarrett CM, Gillinov AM, Blackstone EH. A novel running annuloplasty suture technique for robotically assisted mitral valve repair. J Thorac Cardiovasc Surg. 2010;139:1343–4. 24. Mohr FW, Falk V, Diegeler A, Autschbach R. Computer-enhanced coronary artery bypass surgery. J Thorac Cardiovasc Surg. 1999; 117:1212–15. 25. Loulmet D, Carpentier A, d’Attellis N, et al. Endoscopic coronary artery bypass grafting with the aid of robotic assisted instruments. J Thorac Cardiovasc Surg. 1999;118:4–10. 26. Srivastava S, Gadasalli S, Agusala M, et al. Beating heart totally endoscopic coronary artery bypass. Ann Thorac Surg. 2010;89: 1873–80. 27. Bonatti J, Schachner T, Wiedemann D, Weidinger F, et al. Factors -influencing blood transfusion requirements in robotic totally endoscopic coronary artery bypass grafting on the arrested heart. Eur J Cardiothorac Surg. 2011;39:262–7. 28. Eric JL, Rodriguez E, Chitwood WR. Robotic cardiac surgery. Curr Opin Anaesthesiol. 2011;24(1):77–85. 29. Torracca L, Ismeno G, Alfieri O. Totally endoscopic computerenhanced atrial septal defect closure in six patients. Ann Thorac Surg. 2001;72:1354–7. 30. Argenziano M, Oz MC, Kohmoto T, Morgan J, Dimitui J, Mongero L, Beck J, Smith CR. Totally endoscopic atrial septal defect repair with robotic assistance. Circulation. 2003;108 Suppl 1:II191–4. 31. Suematsu Y, Mora B, Mihaljevic T, del Nido P. Totally endoscopic robotic-assisted repair of patent ductus arteriosus and vascular ring in children. Ann Thorac Surg. 2005;80:2309–13. 32. Gao C, Yang M, Wang G, Wang J, Xiao C, Wu Y, Li J. Total endoscopic robotic atrial septal defect repair on the beating heart. Heart Surg Forum. 2010;13:E155–8. 33. Gao C, Yang M, Wang G, et al. Totally endoscopic robotic ventricular septal defect repair. Innovations. 2010;5(4):278–80. 34. Gao C, Yang M, Wang G, et al. Excision of atrial myxoma using robotic technology. J Thorac Cardiovasc Surg. 2010;139:1282–5. 14 35. Woo Y, Grand T, Weiss S. Robotic resection of an aortic valve papillary fibroelastoma. Ann Thorac Surg. 2005;80:1100–2. 36. Lehr EJ, Rodriguez E, Chitwood WR. Robotic cardiac surgery. Curr Opin Anaesthesiol. 2011;24(1):77–85. 37. Derose Jr JJ, Belsley S, Swistel DG, et al. Robotically assisted left ventricular epicardial lead implantation for biventricular pacing: the posterior approach. Ann Thorac Surg. 2004;77(4):1472–4. 38. Navia JL, Atik FA, Grimm RA, et al. Minimally invasive left ventricular epicardial lead placement: surgical techniques for heart C. Gao failure resynchronization therapy. Ann Thorac Surg. 2005;79(5): 1536–44. 39. Folliguet T, Vanhuyse F, Konstantinos Z, Laborde F. Early experience with robotic aortic valve replacement. Eur J Cardiothorac Surg. 2005;28:172–3. 40. Suri RM, Burkhart HM, Schaff HV. Robot-assisted aortic valve replacement using a novel sutureless bovine pericardial prosthesis: proof of concept as an alternative to percutaneous implantation. Innovations (Phila). 2010;5(6):419–23. 2 Anesthesia for Robotic Cardiac Surgery Gang Wang and Changqing Gao Abstract Robotic cardiac surgery presents anesthesiologists with new challenges and requires a necessary learning curve. The key issues of anesthesia for robotic cardiac surgery are respiratory and cardiovascular changes associated with the patient’s single-lung ventilation and CO2 pneumothorax, which may reduce cardiac output, increase pulmonary vascular resistance, resulting in hypoxemia and hemodynamic compromise. The magnitude of the physiological disturbances is influenced by the patient’s age, the patient’s underlying myocardial and respiratory function and the anesthetic agents administered. In addition, transesophageal echocardiography is needed for guidance of central venous cannula in establishing peripheral cardiopulmonary bypass. Undoubtedly, anesthesiologist plays a more important role in robotic cardiac surgery than in any other surgeries. This chapter describes anesthetic strategies and clinical experience for robotic cardiac surgery. Keywords Anesthetic strategies • Robotic cardiac surgery • da Vinci 2.1 Introduction Since the introduction of the da Vinci Surgical System (Surgical Intuitive, Inc, Mountain View, California, USA) more than 10 years ago, there has been a widespread interest in its use in minimally invasive surgery. Many of the difficulties and limitations of conventional endoscopic approaches have been overcome with the development of the da Vinci Surgical System. For the patient, a da Vinci procedure can offer all the potential benefits of a minimally invasive procedure in addition to a much smaller incision and a much smaller scar. Moreover, other possible benefits are reduced risk of infection, less pain and trauma, less bleeding and less need for blood transfusion, shortened length of stay in the hospital after the procedure and decreased recovery time [1]. Up to today, 18 sets of da Vinci Surgical Systems have been G. Wang, MD • C. Gao, MD (*) Department of Cardiovascular Surgery, PLA General Hospital, No. 28 Fuxing Road, Beijing 100853, People’s Republic of China e-mail: gaochq301@yahoo.com introduced to medical facilities in Mainland China, yet, very few reports have covered anesthetic implications or complications related to the use of this technology. The surgeons at the PLA General Hospital have completed over 640 cases of robotic cardiac surgeries since 2007, the largest cohort of da Vinci robotic cardiac surgeries so far in Asia. In order to keep pace with the developing technologies in this field, it is imperative for cardiac anesthesiologists to have a working knowledge of these systems to formulate an anesthetic plan, recognize potential difficulties and complications, provide safe patient care and adapt to the fast development of robotic cardiac surgery. Objectively speaking, the advent of robotic cardiac surgery has brought new challenges to both surgeons and the anesthesiologists. Publications have described in great detail the difficulties surgeons confront during these procedures [2, 3]. The use of the robotic system for cardiac surgeries, particularly offpump totally endoscopic coronary artery bypass (TECAB), is limited to only a few cardiac centers around the world. For robotic cardiac surgery, due attention should be given not only to anesthetic considerations like alterations imposed by C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_2, © Springer Science+Business Media Dordrecht 2014 15 16 G. Wang and C. Gao the surgical procedure, but also to the patient’s underlying status. Anesthesia for robotic cardiac surgery involves some peculiar perioperative anesthetic concerns which are related to respiratory and cardiovascular changes mainly associated with the patient’s one-lung ventilation (OLV) and CO2 insufflation (CO2 pneumothorax), the increased intrapleural pressure and the CO2 absorption and its general effects, which may reduce cardiac output (CO), increase pulmonary vascular resistance (PVR), resulting in hypoxemia and hemodynamic compromise [4]. In addition, the magnitude of the physiological disturbances associated with surgery is influenced by the patient’s age, the patient’s underlying myocardial and respiratory function and the anesthetic agents administered [5–7]. Apart from off-pump surgery, transesophageal echocardiography (TEE) is needed for guidance of central venous cannula in establishing peripheral cardiopulmonary bypass (CPB). Undoubtedly, anesthesiologist plays a more important role in robotic cardiac surgery than in any other surgeries [8]. Surgical procedures performed in cardiac surgery with the da Vinci Surgical System are as follows: 1. Left and right internal mammary artery harvest with – Totally endoscopic coronary artery bypass (TECAB) – Minimally invasive direct coronary artery bypass (MIDCAB) – Hybrid procedure (coronary artery bypass and stent placement) 2. Totally endoscopic ASD/VSD closure 3. Totally endoscopic mitral valve repair or replacement 4. Other atrial procedures – tricuspid valve repair, myxoma resection etc. 5. Atrial fibrillation ablation, left ventricular lead implantation 2.2 Preoperative Visit The prime goals of preoperative evaluation and therapy for patients before robotic cardiac surgery like other cardiac surgical procedures are to quantify and reduce intraoperative risks to patients during and after surgery. Preoperative evaluation and therapy enable the anesthesiologist to review the patient’s history and results of the preoperative examination, and explain the techniques of anesthesia and monitoring to the patient. The physical examination ensures that airway and chest anatomy should be suitable for insertion of a double-lumen tube to facilitate OLV. Thus, a patient who has documented difficulty with intubation, major scoliosis, or emphysematous chest may be identified in the preoperative clinic as unsuitable for this type of surgery. Awake intubation may be indicated in difficult airway in order to keep the patient breathing spontaneously. Preoperative pulmonary function test, arterial blood gases, and chest X-ray and computed tomographic scan are evaluated; these may provide information to predict whether the patient is suitable for prolonged OLV. On the other hand, preoperative evaluation and communication with the surgical team are necessary for determining the methods and techniques appropriate for induction, maintenance of anesthesia, airway management, and monitoring. The anesthesiologist should tell the patient to continue the necessary medications up to the morning of surgery, e.g. the antihypertensive and antianginal medications, and particularly beta-blockers, which should be continued throughout the perioperative period to decrease myocardial irritability and maintain a slow heart rate. The patients should withhold the morning dose of insulin and oral hypoglycemic medications on the day of the surgery. The anesthesiologist should confirm that the patient does not take aspirin and clopidogrel for at least 5–7 days prior to the surgery, unless the surgeon has specified otherwise [9, 10]. Electrolytes such as potassium and magnesium should be checked preoperatively and should be within normal range prior to anesthesia. 2.3 Patient Selection Aside from understanding the standard contraindications to cardiac surgical intervention, patient selection for robotic cardiac surgery involves a history and physical exam heavily weighted on uncovering factors affecting external and internal thoracic structures. The primary difference between robotic cardiac surgery and sternotomy cardiac surgery is the requirement for prolonged OLV and induced tension pneumothorax. Anesthesiologists should consider the physiologic responses of the patient to robotic cardiac surgery such as hemodynamics, gas exchange, ventilation-perfusion distribution, and echocardiographic or TEE examinations. Until recently, primarily ASA I to II patients have been considered for robotic cardiac surgery. Whether robotic cardiac surgery is suitable for patients with a compromised physical status has been an anesthesiologist consideration. To correctly establish the risks for these “sicker” patients, a more detailed knowledge of the physiologic changes associated with the procedure is indicated. Patients with severe chronic obstructive pulmonary disease (COPD) or asthma or major emphysematous bullae will be poor candidates to tolerate the hypercapnia, potential hypoxemia, and barotraumas resulting from OLV and CO2 pneumothorax. More details are suggested that patients with significant comorbidity, such as compromised pulmonary function tests, resting hypercapnia (>50 mmHg) and hypoxemia (PaO2 <65 mmHg on room air), those requiring additional cardiac procedures, left ventricular ejection fraction <40 %, and dense pleural or pericardial adhesions limiting visibility, are not considered for robotic surgery [11]. Cardiac status is even more important to patients undergoing 2 Anesthesia for Robotic Cardiac Surgery the robotic mitral valve surgery, because with long-standing diseases, patients may develop moderate, even severe cardiac malfunction and high pulmonary arterial pressure during surgery. As a result, patients may become very vulnerable because of OLV, CO2 pneumothorax and CPB. Mishra et al. [12] gave the suggestion of patient selection for TECAB as follows. Patients with significant comorbidity such as compromised pulmonary function, those that require additional cardiac procedures, LVEF <30 %, associated ventricular or aortic aneurysm surgery, or significant peripheral vascular disease precluding femoral CPB procedures, were not considered for robotic surgery. Other preoperative exclusion criteria included body mass index >35.0 kg · m−2, decompensated congestive heart failure (NYHA class III– IV), acute pulmonary edema, uncontrolled hypertension, and any coagulopathy, or history of acute myocardial infarction within 30 days [12]. Usually, in patients with COPD, pulmonary function should be optimized with the aid of bronchodilators, steroids and physiotherapy. Buggeskov and colleagues [13] found that the patients with COPD may be impaired by hypoxemia and systemic inflammatory response during the CPB. For smokers, it is necessary to stop smoking for at least 2 weeks. It was demonstrated that arterial oxygen tension showed significant reduction in heavy smokers in comparison with nonsmokers during OLV [14]. Because of the relatively small number of da Vinci Surgical Systems deployed for cardiac Fig. 2.1 Properly positioned left double-lumen endobronchial tube is confirmed by a fiberoptic bronchoscope 17 surgery to this date, we can assume that as more procedures will be performed using robotic technique and the anesthesiologists will become more familiar with the use of the robotic equipment, it can be expected that there will be more changes in patient-selection criteria. 2.4 OLV and CO2 Insufflation OLV can be established with several methods The simplest method of providing OLV is to intubate double-lumen endotracheal tube, such as Robertshaw tube, Carlens, White, Bryce-Smith, etc. All have two lumina, one terminating in the trachea and the other in the mainstem bronchus. Left Robertshaw tube is most widely used. The advantage of double-lumen endotracheal tube is that it is easy to apply for suction and/or CPAP to either lung. In addition, there are three kinds of single-lumen endotracheal tube with a built-in bronchial blocker. These are achieved by using an Arndt Blocker (wire-guided), a Univent tube, or a Fogarty catheter. Bronchial blockers have been used to establish OLV by using a balloon catheter inflated to occlude the bronchus of the lung being operated on. Tube patency and position should be checked (Fig. 2.1). Secretions may be blocking the tube lumen. Looking at the capnograph trace, if it is changed, it could be concluded as a general rule that the tube has been moved. Even if you have 18 G. Wang and C. Gao One-lung CPAP device Right angle connector Adjustable settings (5−20 cm H2O) Clamp to nonventilated lung (not supplied) 15 mm adaptor Anesthesia breathing circuit To nonventilated lung Endobronchial tube To ventilated lung Fig. 2.2 Application of CPAP to the non-ventilated lung carefully tied it in place, movement may occur during manipulation by surgeons and TEE. Bronchoscopy will confirm this and allow the tube to be repositioned. OLV is initiated prior to insertion of trocar to prevent lung injury. Respiratory changes may occur during the OLV and the CO2 insufflation. Firstly, ventilation-perfusion relationship may be altered by the modified lateral decubitus position in the anesthetized patient during two-lung ventilation. Perfusion is normally distributed preferentially to dependent regions of the lung because of the hydrostatic gradient imposed by gravity to the benefit of the overall ventilation to perfusion ratio (V/Q) maintained. Nevertheless, general anesthesia, neuromuscular blockade, and mechanical ventilation increase V/Q mismatch. Secondly, intrapleural CO2 insufflation positive pressure constricts the lung, reducing compliance, functional residual capacity (FRC) and tidal volume. OLV may cause further damage to ventilatory conditions by limiting the ventilation of the nondependent lung and create an obligatory right-to-left transpulmonary shunt through the nondependent lung [5, 15, 16]. Last, hypercapnia may occur during OLV and pneumothorax, partly due to CO2 absorption across the pleura, and partly because of a mechanical constriction on the pulmonary parenchyma, reducing tidal volume, FRC, total lung capacity and pulmonary compliance [6, 17, 18]. Because of the above changes, it is not uncommon for a patient to desaturate during OLV. If this happens, the first thing needed is to give the patient a larger breath by hand with sustained pressure at the end of the breath, or applying positive end expiratory pressure (PEEP) to the ventilated lung. That may help to prevent the small airways from closing. Usually 5 cm H2O is enough to keep the saturation up without pushing the peak inspiratory pressure too high (above 40 cm H2O). In fact, if PEEP is too high, blood is diverted to the collapsed lung and the shunt is increased, which will worsen the hypoxemia. Meanwhile, it needs to sure that the patient’s blood pressure has not dropped because dropping of blood pressure may also be the cause of desaturation. If severe hypoxemia occurs or airway pressure increases significantly, double-lumen endotracheal tube position should be checked at once with fiberoptic bronchoscope to ensure its proper placement. Add continuous positive airway pressure (CPAP 5–10 cm H2O, 5 L/min) to collapsed lung may help to reduce shunt, divert blood to the ventilated lung effectively and to improve oxygenation (Fig. 2.2). When necessary, reinflating the collapsed lung to return to two-lung ventilation temporarily is always an option. Medication to decreased intrapulmonary shunt due to the collapsed lung include using almitrine (12 μg/kg/min for 10 min followed by 4 μg/kg/min) [19] and inhaled nitric oxide that enhance hypoxic pulmonary vasoconstriction (HPV) [20]. It must be noted that pressure of 5–10 cm H2O will not immediately inflate an already collapsed and atelectatic lung and it may not be very helpful to increase oxygenation right away. Therefore, it is necessary to reinflate the lung with higher airway pressure and then use CPAP to keep lung at a constant level of inflation. High frequency jet ventilation is 2 Anesthesia for Robotic Cardiac Surgery another method and keeps the lung almost immobile helping with operating conditions [21]. Currently, the definition of permissive hypercapnia has been approved by more and more clinicians. The literature generally agrees that CO2 should be allowed to rise while reducing tidal volume and minute ventilation in order to prevent alveolar overdistention or the propagation of lung injury [22, 23]. The use of excessive airway pressures may increase pulmonary vascular resistance in the dependent lung and increase flow through the nondependent lung. Therefore, the lungs should be protected against high airway pressures during OLV with intrapleural CO2 insufflation, by carefully balancing tidal volume, respiratory rate, minute ventilation and PETCO2 [17, 23–26]. In clinical conditions, PETCO2 that shows the tendency to increase during the course of the OLV and CO2 pneumothorax and sometimes is higher than the normal range, is nevertheless always within the ranges foreseen for moderate permissive hypercapnia [22]. During OLV, arterial oxygenation may markedly decrease because of an increased intrapulmonary shunt due to the collapsed lung. Therefore, it is necessary to increase FiO2 to over 0.5 during OLV and CO2 pneumothorax. The increase of FiO2 is the principal measure allowing an adequate oxygenation. Hypoxic pulmonary vasoconstriction (HPV), a physiologic defense mechanism that serves to divert blood away from poorly ventilated lung regions, is a second way to maintain oxygenation during OLV by restricting pulmonary blood flow to the nondependent lung. OLV management should be reduced to the minimum in any clinical conditions that might directly vasodilate hypoxically constricted lung vessels, such as the presence of infection, vasodilator drug infusion and the use of certain anesthetics (Table 2.1) [12, 27, 28]. Intravenous anesthesia does not influence HPV, while isoflurane, desflurane and sevoflurane have been shown to have less effect on HPV than halothane. To limit their effects on oxygenation, inhalation agents should be used at minimal concentration or less [17, 25]. Also, the intraoperative hypoxia can be reduced by delivering lowflow oxygen to the nondependent lung through a doublelumen bronchial tube or a bronchial blocker with a distal port [15, 27]. CO2 insufflation causes significant circulatory perturbations, alone or in combination with OLV. Cardiovascular function is impaired proportionally to intrathoracic CO2 pressure [29]. An excessive positive pressure results in significant hemodynamic compromise which reduces preload, stroke volume, cardiac index, mean arterial pressure and reflex tachycardia [16, 30, 31]. Therefore, in early stage, the intrapleural pressure is monitored directly via an 18-gauge IV cannula and pressure transducer to avoid excessive pressure generation [10]. Nevertheless, slow increase of the intrathoracic CO2 pressure, limitation of CO2 insufflating 19 Table 2.1 Anesthesiology interventions that modify HPV (Reproduced with permission from Nagendran et al. [28]) Decrease HPV Dextran volume replacement Halothane Halothane and verapamil Nifedipine Alkalosis (respiratory or metabolic) Nitroprusside Hypothermia Pregnancy Increase HPV Lateral decubitus position Thoracic epidural anesthesia Propofol Lidocaine High-frequency positive pressure ventilation Neutral to HPV Propofol Enflurane Isoflurane Fentanyl pressure, and cardiovascular function optimization (by fluid administration or possible use of inotropic agents) are effective to minimize the hemodynamic changes with only a slight reduction in the preload, but without any major effects on cardiac output and mean arterial pressures [25, 30, 32]. So the hemodynamic compromise is generally well tolerated by the patients with normal cardiac function. A correct way is that the intrapleural insufflation is always performed in stages and the desired intrathoracic pressure should never be attained in less than 1 min. A recent study on adult thoracoscopy compares OLV with intrapleural CO2 insufflation in respect of the hemodynamic and respiratory effects. The investigation shows a reduction in cardiac index due to intrapleural insufflation that is statistically greater than that provoked by OLV, while the variations in the oxygenation index are statistically greater during OLV with respect to intrapleural insufflation [33]. In one word, intrapleural CO2 insufflation brings about hemodynamic changes characterized by a fall in systolic and diastolic blood pressure greater than in OLV. On the other hand, respiratory endangerment arises due to a greater rise in PETCO2 in patients undergoing OLV than in those where more intrapleural insufflation is applied [34]. In patients with preoperative pulmonary abnormalities, PETCO2 is statistically higher both during OLV and after pleural cavity deflation. The restrictive, obstructive and mixed ventilatory defects need careful ventilatory strategies. In such cases high intraoperative airway pressure should be avoided and a small increase in PETCO2 is preferable [35]. 20 G. Wang and C. Gao Table 2.2 Hemodynamic changes after induction of anesthesia with hypnotics [39] HR MBP SVR PAP PVR PAO RAP CI SV LVSWI dP/dt Diazepam −9 ± 13 % 0–19 % −22 ± 13 % 0–10 % 0–19 % Unchanged Unchanged Unchanged 0−8 % 0–36 % Unchanged Droperidol Unchanged 0–10 % −5–15 % Unchanged Unchanged +25 ± 50 % Unchanged Unchanged 0–10 % Unchanged – Etomidatea −5 ± 10 % 0–17 % −10 ± 14 % −9 ± 8 % −18 ± 6 % Unchanged Unchanged −20 ± 14 % 0–20 % 0–33 % 0–18 % Ketamine 0–59 % 0 ± 40 % 0 ± 33 % +44 ± 47 % 0 ± 33 % Unchanged +15 ± 33 % 0 ± 42 % 0–21 % 0 ± 27 % Unchanged Lorazepam Unchanged −7–20 % −10–35 % – Unchanged – Unchanged 0 ± 16 % Unchanged – – Midazolam −14 ± 12 % −12–26 % 0–20 % Unchanged Unchanged 0–25 % Unchanged 0–25 % 0–18 % −28–42 % 0–12 % Propofol −10 ± 10 % −10–40 % −15–25 % 0–10 % 0–10 % Unchanged 0–10 % −10–30 % −10–25 % −10–20 % Decreased CI cardiac index, dP/dt first derivative of pressure measured over time, HR heart rate, LVSWI left ventricular stroke work index, MBP mean blood pressure, PAP pulmonary artery pressure, PVR pulmonary vascular resistance, PAO pulmonary artery occluded pressures, RAP right atrial pressure, SV stroke volume, SVR systemic vascular resistance a The larger deviations are in patients with valvular disease 2.5 Induction and Maintenance of Anesthesia The hemodynamics stability should be taken into consideration in cardiac anesthetic selection (Table 2.2). Today cardiac anesthesia is still based on fentanyl or sufentanil, in combination with etomidate, midazolam, and muscle relaxats for induction and trachea intubation with a double-lumen endotracheal tube. Longer acting muscle relaxants i.e. pancuronium or pipecuronium may subsequently be supplemented to ensure patient paralysis after port placement [36, 37], because patient movement with robotic arms in situ may be devastating [38]. There is no single strategy to be recommended for maintenance of anesthesia; hypnotics (midazolam or propofol), opioids and volatile anesthetics are used in different combinations. The dose and selection of anesthetic agents must provide adequate anesthesia and analgesia during induction and surgery, and attenuate the hemodynamic responses to laryngoscopy and surgery. For robotic cardiac surgery, dosages and the type of the drugs that are to be used depend on the desire of ‘fast-track’ – extubation in the operating room or, more commonly, several hours after arrival in the ICU (Table 2.3). High-dose opioids based anesthetic management of the cardiac surgical patients, with more stable hemodynamics providing a long-term mechanical ventilation, has been supplanted by protocols using low-dose fentanyl, sufentanil, or alfentanil [41, 42], to facilitate early extubation. Sufentanil is used in combination with midazolam, propofol and inhaled anesthetics to provide more stable hemodynamics when it is compared with fentanyl-based anesthetic protocols. Sufentanil has a half-life of about 20–40 min and allows patients to awaken within hours of completion of the operation. Remifentanil is a short-acting, esterase-metabolized without any active metabolites, rapidonset μ-opioid receptor agonist, with a context-sensitive half-life of 3–5 min that Table 2.3 Recommended induction doses [40] Drug Induction dose Hypnotics Propofol 1–2 mg/kg Thiopental 2–4 mg/kg Etomidate 0.15–0.3 mg/kg Opioids Fentanyl 3–10 μg/kg Sufentanil 0.1–1 μg/kg Remifentanil 0.1–0.75 μg/kg/min or bolus 0.5–1 μg/kg Muscle relaxants Cisatracurium 70–100 μg/kg Vecuronium 70–100 μg/kg Pancuronium 70–100 μg/kg Rocuronium 0.3–1.2 mg/kg Succinylcholine 1–2 mg/kg Maintenance of anesthesia in critically ill patients Sedative/hypnotic agent Propofol 20–100 μg/kg/min Lorazepam 2–4 mg (25–50 μg/kg) Diazepam 4–8 mg (50–100 μg/kg) Midazolam 0.25–0.5 μg/kg/min An opioid infusion Remifentanil 0.05–0.1 μg/kg/min Fentanyl 0.03–0.1 μg/kg/min Sufentanil 0.01 μg/kg/min Dexedetomidine 0.5–1 μg/kg/h may be beneficial in shorter operations and in elderly patients [43–45]. It provides stable hemodynamics in high-risk cardiac surgical patients. Remifentanil-propofol combination is usually selected for patients who can be extubated promptly after surgery. Thus, propofol has not been shown to increase overall hospital costs [46]. Midazolam has been shown to have an average elimination half-life of 10.6 h in patients recovering from cardiac 2 Anesthesia for Robotic Cardiac Surgery surgery [47]. Although early extubation can be achieved in patients receiving midazolam throughout surgery, most groups limit its use to the pre-bypass period. Propofol providing stable hemodynamics at the recommended doses of infusion 2–4 mg/kg/h and continue it in the ICU [4, 8]. Propofol decreases systemic blood pressure and systemic vascular resistance because of its strong vasodilator properties. The major advantage of using propofol is the early extubation leading to shortening the length of stay in ICU. When the patient is stable, propofol is turned off and the patient is allowed to awaken [48]. Cason et al. [49] first described the term anesthetic preconditioning in 1997, by showing protective effect of isoflurane applied shortly before ischemia. Since then numbers of experimental studies revealed the cardioprotective efficacy of volatile anesthetics [50]. Agents commonly used include isoflurane, enflurane, desflurane, and sevoflurane, which are generally given during CPB to maintain anesthesia and reduce blood pressure, and allow to decrease the doses of intravenous medications. Desflurane and sevoflurane have less lipid solubility with a rapid onset of action and are quickly reversible, allowing for early extubation. A recent meta-analysis the choice of desflurane and sevoflurane results in better outcome in terms of mortality and cardiac morbidity in cardiac surgical patients [51]. Although the exact mechanism of preconditioning of volatile anesthetics is not yet known, the cardiac depressant effects that reduces myocardial oxygen demand, were demonstrated to have direct cardioprotective effects [50]. Nitrous oxide is contraindicated because it reduces the amount of oxygen that can be delivered and may also increase pulmonary arterial pressures. Muscle relaxants are given throughout the operation to minimize patient movement and suppress shivering during hypothermia. Pancuronium offsetting the bradycardia effect of high-dose opioids has been the prefered neuromuscular blocker, however it has also been shown to have potential to produce a tachycardia causing myocardial ischemia during induction. In contrast, vecuronium and pipecuronium have very few hemodynamic effects. Rocuronium is a short-acting neuromuscular blocker with a rapid onset of action and vagolytic properties. It provides more adequate conditions especially for fast track anesthesia due to its less residual blockade and shorter time to extubation [52]. Atracurium does not undergo renal elimination and is the best agent to be used in patient with renal insufficiency [53]. 2.6 Anesthetic Technique In robotic cardiac surgery, anesthesiologist should be versed in cardiac and thoracic anesthesia and familiar with the skills required for TEE and nonsternotomy CPB. Strategies of respiratory management are the key point of anesthesia 21 involving OLV and CO2 pneumothorax. However, OLV and CO2 pneumothorax can be the cause of hemodynamic instability and should be closely monitored. CO2 insufflation in the chest cavity will lead to an increase in peak airway pressure, particularly during OLV. Usually, double lumen tube is mostly used for OLV and should be replaced by a single lumen tube following surgery. However, care must be taken that swelling of the glottis and pharynx resulting from intubation and TEE might make reintubation difficult. In a few cases in which the airway is deemed to be difficult, Univent tube or bronchial blocker should be used, and optimal position is achieved with the use of a fiberoptic bronchoscope [54]. Although they do not allow CPAP or suction to the collapsed lung, they do not need to be replaced at the end of surgery. They may be placed more easily in patients who are difficult to intubate or who have a small glottis opening, which often would not accommodate the large double lumen tube. TEE guidance of cannula during peripheral cardiopulmonary bypass is crucial to success. Femoral-Femoral bypass is the most commonly used technique. Complications from arterial cannulation are reduced when TEE is used to confirm the location of the arterial wire within the aorta. Venous cannulae must also be guided into the inferior vena cava and into the superior vena cava [55]. Also, the surgeons now rely almost exclusively on high-quality intraoperative TEE imaging to plan mitral valve repair. A saline test is performed intraoperatively to confirm the echocardiographic findings, and occasionally measure the valve segments directly [56]. Because the side cart is close to the patient’s head, there is limited access to the patient’s airway and neck. Anesthesiologist and the bed-side assistant must be guarded against patient-robot collision during surgery, which is defined as a limitation in the free movement of the robot’s telemanipulated arms by interference with the patient’s body [57]. After the robot is engaged, the patient’s body position cannot be changed. The surgical team should be capable of rapidly disengaging the robotic device if an airway or anesthesia emergency arises. An optimal surgical position is that the patients are placed in an incomplete side-up position at a 30° angle right or a left lateral decubitus position. Positioning the arm of the elevated side along the side with gentle elbow flexion has reduced conflict with robotic arms and decreased risks of a brachial plexopathy. It is important to take care of avoidance of unnecessary stretching of the elevated side arm because it can produce damage to the brachial plexus. A recent case report [58] described a brachial plexus injury in an 18-year-old male after robot-assisted thoracoscopic thymectomy. In this report the left upper limb was in slight hyperabduction. In some centers, the arm of the elevated side is hanged above the head. The elevated arm should be protected by using a sling resting device [59]. Before the arm of the robot is in the chest cavity, a complete lung collapse must be maintained throughout the 22 procedure. Robotic surgery with the da Vinci Surgical System does not allow for changes in patient position on the operating table once the robot has been docked. Close communication between the surgeon and anesthesiologist in relation to the positioning and functioning of the robot is mandatory. As the heart is limited by the minithoracotomy approach, cardiac defibrillation must be provided by means not requiring direct epicardial contact. External defibrillator pads are placed on the back and the opposite chest wall. Successful termination of ventricular fibrillation (VF) by electrical defibrillation is dependent on the delivery of sufficient electrical current through the heart to depolarize a critical mass of myocardial tissue [60–62]. Transmyocardial current is directly related to the energy delivered, and inversely related to transthoracic electrical impedance (TTI) [63]. Because air and CO2 in the chest act as electrical insulators, they can increase both TTI and defibrillation thresholds [64]. There are other proofs, pneumothorax has been linked to repeated failed defibrillation and increased energy requirements during induced VF with implantable cardioverter-defibrillator placement [65–67]. In these cases, resolution of pneumothorax results in improvement in defibrillation thresholds. Hatton et al. [68] reported a case of multiple failed defibrillation attempts during robot-assisted LIMA harvest during OLV that VF might be resulted from inadvertent pericardial application of electrocautery. The 4th time of external defibrillation attempt with resumption of two-lung ventilation and decompression of the iatrogenic pneumothorax, the patient was successfully defibrillated. The bulk of the robot is positioned over the abdomen and chest. Although the incidence of airway or serious cardiovascular events are no greater in robot-assisted surgery, if they do occur, the position of the robot will interfere with effective cardiopulmonary resuscitation and airway interventions [69]. The theatre team should practice an emergency drill for the removal of the robotic cart. The successful use of the robot to assist in surgery depends upon excellent communication among all members of the theatre team. The surgeon sits behind a console, away from the site of operation, but must communicate effectively with both anesthetic staff and his operative assistant at the patient’s bedside. The special care must be taken to ensure that transfer of information is precise and clear. This is aided by the addition of audio speakers to the video tower that transmits the operating surgeon’s voice. The postoperative course is usually uneventful. On arrival in the cardiac surgery ICU, all patients remain sedated (usually with propofol) until hemodynamics become completely stable and with minimal blood drainage. The incidence of complications is low. Blood transfusion is not normally required as intraoperative blood loss is very low, but significant hemorrhage may be insidious and the patient should be G. Wang and C. Gao carefully monitored in the immediate postoperative period. Postoperative analgesic considerations are similar to those corresponding non-robotic operations. 2.7 Anesthesia Consideration of Robotic Assisted CABG on Beating Heart For robotic assisted CABG on beating heart, fast-track anesthesia with early extubation appears to be normal, which can involve either extubation immediately at the conclusion of surgery or within a few hours of arrival in the ICU. The goal of minimally invasive coronary artery bypass grafting is to perform the entire anastomosis endoscopically and avoid CPB. The result is to reduce postoperative morbidity, length of hospital stay, and overall cost. Advances and experience in beating heart surgery have aided this approach. The first closed-chest CABG surgery with the aid of robotic instruments was performed on human in June 1998 [70]. Thereafter, the technique of robotic assisted CABG has achieved perfection. Technical advances in minimally invasive surgery have enabled CABG to be performed through very small ports. Sternotomy alone carries a finite risk of morbidity from an inflammatory response, but it is less than that of exposure to cardiopulmonary bypass [71, 72]. Robotic assisted CABG on beating heart (off-pump) includes two kinds of surgeries: TECAB and MIDCAB in which the left internal mammary artery (LIMA) is harvested robotically and direct anastomosis through a small left anterior thoracotomy incision (6 cm) [73–75]. Although the anesthetic concerns in managing robotic assisted CABG operation are similar to those of any patient requiring surgical revascularization, this surgical technique requires greater communication and coordination between the surgical team and the anesthesiologist. The anesthesiologist in this setting must provide both hemodynamic stability and relative bradycardia. Because the minithoracotomy incision permits only limited access to the heart, the anesthesiologist must give early warning of impending cardiovascular collapse and the need for emergent institution of CPB. So a perfusionist should always be prepared in the operating room in the event of the need for CPB. Performance of the distal anastomosis involves the use of a myocardial stabilizer designed to isolate a small segment of myocardium with the relevant coronary artery, and proximal and distal silastic sutures to control back-bleeding [10]. Intracoronary shunts are often used to facilitate anastomosis and maintain distal perfusion, particularly to the target vessel that the myocardium perfusion still depends on. But putting the intracoronary shunt into the target vessel is not easy in TECAB surgery and it may disturb the anastomosis with continuous suture or U-clip. Alternatively, it can be done to provide ischemic preconditioning to assess 2 Anesthesia for Robotic Cardiac Surgery the possibility of not using intracoronary shunt during the anastomosis, a 5 min test occlusion of the LAD is conducted before coronary arteriotomy [76]. If this is well tolerated, the LIMA to LAD anastomosis is completed without CPB. If signs of ventricular dysfunction appear, median sternotomy may be performed, and the patient can be placed on CPB, or alternatively, femoral-femoral CPB may be initiated. In our institution, the details of anesthesia are as follows [4, 8]. Patients are prepared and draped as for conventional cardiac surgery, permitting sternotomy in case of need. All cardiac medications should be continued up to the day of surgery. Patient monitoring consists of standard electrocardiogram leads II and V5 and a right radial artery catheter placed under local anesthesia before induction. Intubation is performed with a left-sided double-lumen endotracheal tube and correct placement is confirmed by both auscultation and fiberoptic bronchoscopy. After intubation, a pulmonary artery catheter is placed in the right internal jugular vein (RIJV). A two-lumen central venous catheter is also placed in the RIJV in all patients. TEE probe is placed after all central catheters are inserted. This anesthetic protocol permits patients to be entered into an early extubation and fast-track recovery protocol. Postoperative analgesia is administered with intravenous sufentanil. It is important that throughout the operation the heart rate remains slow and stable. The combined use of nitroglycerin and beta-blockade minimizes the possibility of myocardial ischemia during the period of vascular occlusion. If systemic hypotension occurs as a consequence of the procedure or from the anti-ischemia therapies, small amounts of phenylephrine or norepinephrine are administered to transiently augment vascular tone and restore systemic pressure. The effects of drug administration on the cardiac index, pulmonary artery pressures, and ventricular function as assessed by TEE are closely monitored. Usually, CO2 insufflation and OLV increase central venous pressure and pulmonary artery pressure by a small amount [77]. For the multivessel revascularization indication, both internal thoracic arteries (ITA) may be used for grafting of the LAD, diagonal branch, right circumflex, and right coronary artery. Bilateral ITA grafting is feasible but appears to be very challenging and time consuming. Such a procedure should be accepted only for very special indications [78]. For harvesting both ITA, insufflation of the left hemithorax is sufficient to expose the right internal mammary artery because of the leftward position of the heart and the improved angle of sight. If the right side pleural is broken, both sides of intrapleural CO2 positive pressure may cause further damage to ventilatory conditions by limiting the ventilation of the right lung and increased CO2 absorption across the pleura, and this may result in hypercapnia and tachycardia more easily. To control heart rate slower and stable is 23 difficult in the situation. Most patients studied tolerate bilateral pneumothorax well for periods less than 1 h [79]. Graft patency is usually evaluated intra-operatively using direct measurement of blood flow by means of a Doppler flow meter. The blood flow measured is thus dependent on systemic blood pressure and distal coronary run-off. 2.8 Anesthesia Considerations of Minimally Invasive Mitral Valve Surgery with da Vinci Surgical System Technological innovations are improving minimally invasive mitral valve surgery as da Vinci Surgical System becomes a feasible, safe and effective option in mitral valve surgery [80, 81]. It is claimed that the robotic mitral valve repair and replacement allow complete anatomic correction of all categories of leaflet prolapses, enhance visualization of the valve which can afford a high mitral valve repair rate, offer excellent freedom from adverse events, decrease ventilation time and length of stay [82, 83], and have excellent early-term and mid-term results [84]. The preoperative considerations required for anesthesiologists is to evaluate and estimate the cardiac and lung functions of the patients, as well as the change of pathophysiology of heart, the tolerance to OLV and CO2 pneumothorax, and the effect of CPB. All these need adapt the prudent strategy to manipulation of the infusion, use of inotropic and reasonable ventilation management in order to maintain the stable of hemodynamic and effective deal with hypoxemia. From the induction of anesthesia to start the CPB, it is crucial to maintain stable hemodynamic and oxygenation. An understanding and an appreciation of pathophysiologic changes associated with mitral stenosis and mitral insufficiency form the foundation of anesthetic management in this kind of patients. With long-standing mitral valve disease, the elevated left atrium pressure leads to passive increases in pulmonary arterial and venous pressure. During surgery the CO2 pneumothorax is needed which may artificially create a positive intrathoracic pressure and results in relative hypovolemia by reduce the venous return. In addition, most patients with valve heart disease have increased dependency and sensitivity to ventricular preload. The adequate intravascular fluid is not only benefit to keep heart rate in an optimal range but also to maintain the cardiac preload. Tachycardia has detrimental effects on mitral stenosis because of the decreased time for diastolic filling. For mitral insufficiency patients, especially with ventricular distention, the inotropic (dopamine or epinephrine) is often used to maintain a stable hemodynamic condition. Hypoxemia may occur during OLV, especially in the post-CPB phases. The following factors may contribute to Hypoxemia. Firstly, left OLV is more harmful to 24 oxygenation. Slinger et al. [85] found that the side of position to be one of the important factor in predicting hypoxemia during OLV, which may be relevant to the fact that the right lung is larger than the left one. A recently study also found that, while ventilating with an FiO2 of 1, mean arterial oxygen tension was approximately 280 mmHg on the left-sided as compared with approximately 170 mmHg on the right-sides thoracic operation during OLV [86]. Secondly, the airway is narrowed because of the use of double-lumen endotracheal tube, prolonging alveolar emptying time. Some alveoli are over inflated and damaged because of the high inspiratory pressures during OLV resulting in alveolar edema [38]. Fortunately, the hypoxic pulmonary vasoconstriction (HPV) is beneficial to reduce the perfusion of the nonventilation lung and improving oxygenation [87]. It is demonstrated that the level of tidal volume during OLV could be maintained just as that during twolung ventilation without positive end-expiratory pressure, targeting normalization of CO2 [88, 89]. Thereby, it is reasonable to keep the tidal volume as in two-lung ventilation and regulate the respiratory rate (10–15 bpm) to maintain the PETCO2 in 40 mmHg. The TEE is crucial for proper placement of the catheter, such as the femoral venous (IVC) and internal jugular venous (SVC), and the transthoracic aortic root cannulation in robotic mitral valve surgery. The TEE can not only contribute to complete de-airing of the cardiac chambers before coming off CBP so that coronary air embolism and subsequent right or left ventricular dysfunction are minimized, but also help to assess the quality of the mitral valve procedure and the status of aortic valve. The CO2 insufflation is adopted, which has the advantage of creating high carbon dioxide levels in the left cardiac chambers, potentially reducing the risk of air embolism. It is claimed that the neurologic deficits could result from inadequate deairing or retained particulate embolus from the operative field [90]. Therefore, to ensure removal of all source of potential embolus, the surgeon should be very careful with broken sutures and other debris encountered during the procedure. It is found that the nodal arrhythmia frequently appear after termination of CPB. The potential cause of the phenomenon is not explicit. The thin muscular wall of the right atrium possesses less resistance to mechanical shift and ischemia injury resulting from OLV and intrathoracic CO2 positive pressure, and that eventually leads to dysfunction of sinoatrial node. A similar situation has been that OLV can add strain on the right ventricle in patients with preexisting dysfunction leading to decompensation, and the persistent hypoxemia during OLV will increase sympathetic tone and can lead to arrhythmia promotion [91]. Sometimes, the nodal arrhythmia is harmful to maintaining of the circulatory stability, so cardiac pacemaker may be needed temporarily. G. Wang and C. Gao Fortunately, in our series, most patients automatically regained sinus rhythm at 30–60 min after CPB is stopped. Since CPB is typically associated with hemodilution, hypothermia, and nonpulsatile blood flow, the cross-sectional area and the flow profile of the cerebral vessels may not remain constant during hypothermic CPB [92]. The conditions of hypothermic CPB may potentially damage the cerebral blood flow when the peripheral CPB is established through the femoral arterial and venous. So it is worth stressing that the ventilation should restart as early as possible before weaning off the CPB, especially when the perfusion volume is being reduced. We observed that hypoxemia mostly occurred after terminating CPB during OLV [4], at this point surgeons are engaged with identifying and controlling any bleeding. The following factors may be responsible for hypoxemia: (1) Blood contact with artificial surfaces during CPB that may provoke systemic cytokine-mediated inflammatory, lung ischemia and reperfusion injury with increases in immunologic mediators and CPB-induced non-physiologic laminar perfusion, are considered reasons for postoperative hypoxemia [93, 94]. These injuries mostly lead to a postoperative pulmonary interstitial edema and abnormal gas exchange. (2) The intrapulmonary shunting through the collapsed nondependent lung and ventilation/perfusion mismatch in the dependent lung can become most serious after terminating CPB. Other studies also found similar results that terminating CPB during OLV significantly impaired oxygenation and may expose patients to critical low oxygen for a period of time [during OLV significantly decreased PaO2/FiO2 from 50.8 (12.1) kPa after induction to 24.1 (14.9) kPa], after returning to double lung ventilation PaO2/FiO2 significantly increased to near baseline values [95]. (3) Some studies proved that neutralization of heparin with protamine is inducing activation of the classic pathway complement system, action which is correlated with postoperative pulmonary shunt fraction [96, 97]. Therefore, it is intelligent to deliver oxygen intermittently to the collapsed lung to improve oxygenation in terms of SpO2 lower than 90 % with 100 % of FiO2. If this method does not improve oxygenation, it would be effective to use continuous positive airway pressure (CPAP) (5–10 cm H2O) to the non-independent lung by expanding the nonventilation lung and keeping it expanded during prolonged OLV for prevention and treatment of hypoxemia [98]. It is suggested that routine CPAP not only can improve oxygenation but also be beneficial in reducing to the nonventilated lung [99]. In addition, increasing PEEP up to 10 cm H2O may be needed throughout the operation to achieve adequate oxygenation. However, when above methods are not improving oxygenation, the anesthesiologist should ask the surgeon to stop the hemostasis and temporarily restore two lung ventilation until SpO2 returns to the normal range. 2 Anesthesia for Robotic Cardiac Surgery 2.9 Monitoring of Cardiovascular System Standard perioperative monitoring includes pulse oximetry, electrocardiogram (ECG), PETCO2, invasive blood pressure measurement, temperature and urine output. The ECG often involves using leads II and V5 and using automated ST-segment monitoring. Visual inspection of the ECG on the monitor has low sensitivity in diagnosing ischemic changes. Modern ECG monitors can provide automatic ST segment analysis for the detection of ischemia, which depends on the computer’s ability to accurately set the isoelectric and J-point reference points. Before induction of general anesthesia and after local anesthesia, a radial arterial cannula is inserted into the radial artery for blood sampling and pressure monitoring. If an endoaortic occlusion device is used, bilateral radial arterial catheters are required to monitor correct balloon placement. Patient risk factors and comorbid conditions often necessitate real-time, beat-to-beat assessment of arterial perfusion pressure and arterial blood gases. Furthermore, during nonpulsatile CPB, intraarterial catheter allows continuous monitoring of arterial blood pressure and interval blood gas sampling. We suggest pulse oximeter and arterial blood pressure monitoring in the contralateral arm to the surgical approach. A central venous catheter is a reasonable consideration as a monitor of central venous pressure. Central venous catheters, in addition to monitoring CVP, provide portals for volume replacement, pharmacologic therapy, and insertion of other invasive monitors such as pulmonary artery (PA) catheter. CVP monitoring has its limitations as at times it becomes erratic due to compression of the major vessels and heart itself by robotic instruments. The values should be noted when there are no obvious compressions of major vessels or heart directly. Moreover, trends may be more important than single values. Also pneumothorax increases the CVP by about 6–8 mmHg. Therefore, it is reasonable to administer fluid to maintain the urine output of more than 0.5 ml/kg/h during the perioperative period, although randomized studies are lacking at this time to confirm this statement [100]. Thus, urine output should be measured to aid in fluid management during long procedures. PA catheter is usually introduced percutaneously via the RIJV into the pulmonary artery by pressure tracing, because the RIJV provides ease of approach and optimal distance from the operative field. It is used to measure CVP, PAP, PCWP, and CO. Most centers report routine use of PA catheters. In some cases an endopulmonary vent catheter is placed by the anesthesiologist to function as an indirect left atrial drainage catheter. Because OLV and pneumothorax could decrease lung volumes, impair ventilation, and increase CO2 absorption, airway pressures, ventilatory volumes, capnography, 25 compliance, and arterial blood gas monitoring can be very crucial. Bispectral (BIS) analysis to monitor depth of anesthesia can be used to titrate and minimize the amount of medication required to maintain adequate anesthesia (aiming for a target value of less than 60) while preventing awareness to assist in fast-tracking patients [101, 102]. This is useful during bypass when hemodilution increases the effective volume of distribution and may necessitate redosing of anesthetic medications. Near-infrared spectral analysis aids in ensuring adequate brain protection and leg perfusion with alternative cannulation strategies [103]. After induction of anesthesia, a TEE probe is introduced into the esophagus. Use of TEE is indicated for positioning of percutaneous arterial, venous, and coronary sinus catheters in robotic operations. 2.10 Establishment of Peripheral Cardiopulmonary Bypass With the development of the da Vinci Surgical System, robotic cardiac surgery could be performed safely with modified perfusion management. Modified perfusion technology including smaller arterial and venous cannulae, transthoracic clamp, endoaortic balloon clamping devices and assisted venous drainage has facilitated peripheral CPB greatly [104]. Ultrasound guided RIJV access now is a recommended practice (Figs. 2.3 and 2.4) and TEE is critical for assessment of venous cannula positioning, retrograde cardioplegia cannula position (if used), and intra-aortic balloon occlusion device positioning (if used). Femoral-Femoral bypass is the most commonly used technique. Complications from arterial cannulation are reduced when TEE is used to confirm the location of the arterial wire within the aorta. Femoral arterial cannula is positioned using a modified Seldinger guidewire technique under TEE guidance. The axillary artery cannulation may be more appropriate for patients with peripheral atherosclerosis [105]. Vascular injuries from femoral cannulation include arterial occlusion, localized arterial injuries, and aortic dissections. Major aortic dissection is rare, but devastating, and occurs in 1–2 % of patients [106–109]. To avoid these complications, preoperative screening for peripheral vascular disease may include noninvasive plethsmography, computed tomography, or selective angiography. Venous cannulae must also be guided up the superior vena cava (SVC) and into the inferior vena cava (IVC). Care must be exercised to prevent the cannulae from crossing the atrial septum, which may result in poor venous return, an obscured surgical field and possible perforation of the left atrium. There are two techniques for endovenous drainage cannula. One is administration of Carpentier Bicaval G. Wang and C. Gao 26 Fig. 2.3 Ultrasonic guidance catheter placement in RIJV Fig. 2.5 A 16-gauge conduct catheter placed in the RIJV by the anesthesiologist Puncture point 2 RIJV RCA Fig. 2.4 Ultrasound imaging of the RIJV, anterior and lateral to the right carotid artery (RCA) femoral cannula in the right femoral vein. Another is venous drainage consisted of a single-stage venous drainage cannula in the right femoral vein and a smaller cannula positioned in the RIJV by the anesthesiologist (Figs. 2.5 and 2.6). The latter is used for SVC drainage during CPB. These two methods of venous drainage cannulation require guide by the TEE. A 15F–17F wire-bound Biomedicus cannula (Medtronic Inc, MI, USA) is inserted into the RIJV using the Seldinger technique and positioned at the atrial/SVC junction after systemic heparization to obtain an activated clotting time (ACT) >480 s. The femoral vein cannula size is determined by the patient’s body surface area and circulatory requirements. The correct position of the cannulae is checked by TEE. Jugular venous cannula (JVC) and femoral venous cannula (FVC) are joined to each other with a ‘Y’ connector, which makes up the venous inlet to the CPB circuit. Fig. 2.6 The conduct catheter in the RIJV replaced with SVC drainage cannula by surgeon The long, relatively small venous cannula may result in impaired venous drainage. If the cannula is not snared, blood may enter the right ventricle, be pumped through the lungs and into the systemic arterial tree, resulting in shunting if the lungs are not ventilated. Although arterial blood gases drawn from the patient will show desaturation, those from the CPB circuit will not. If the SVC is snared, then blood will pool into the venous system causing a rise in jugular venous pressure and a reduction in cerebral perfusion pressure. This may be dramatic with jugular pressures of 40 mmHg and systemic pressures of only 50–60 mmHg resulting in cerebral perfusion pressures of only 10–20 mmHg. To recognize this occurrence, SVC pressures should be monitored during CPB [110]. In peripheral CPB, access for direct insertion of largebore cannula is not feasible. For this reason, gravity-assisted 2 Anesthesia for Robotic Cardiac Surgery venous drainage is often inadequate [111]. This can lead to poor surgical visualization and distention of the myocardium leading to poor patient outcomes [112]. So it is almost necessary to use the assisted drainage in peripheral CPB. Assisted drainage improves siphoning of venous blood return flow to the CPB machine. A variety of methods can be used to improve assisted venous drainage, but, most commonly, kinetic-assisted (KAVD), Vacuum-assisted venous drainage (VAVD) and roller-assisted venous drainage are used [104, 113]. Cirri et al. [114] compared the vacuumassisted drainage and kinetic-assisted drainage with centrifugal pump in respect of hemolysis on CPB. They found an increase in hemoglobinuria and a decreased platelet count in the vacuum-assisted drainage group, and concluded that the red cell and platelet damage were reduced when the kineticassist mode of venous drainage was used. The major disadvantage associated with kinetic-assisted venous drainage was the entrainment of macrobubbles in the venous line, requiring manual clearing of the centrifugal pump. When VAVD was clinically applied for the first time, many problems were encountered. Some initial cases resulted in inadvertent air emboli to the patient [115]. With the use of a vacuum regulator (the Hamlet Box), Munster et al. [112] showed that VAVD could be used in a safe manner. Up to now, vacuum-assisted venous drainage is the popular practice in most centers although kinetic-assisted venous drainage has been shown to be physiologically superior. VAVD utilizes a standard vacuum suction source connected to a hard-shell venous reservoir, which creates suction in the entire drainage system and increases venous return. It requires close regulation of the vacuum source to avoid negative pressure variations; excessive VAVD can cause trauma to the blood components in addition to cracking or imploding of the venous reservoir. Regulators must be used to maintain precise vacuum pressures. Moreover, positive and negative pressure relief valves must be incorporated into the reservoir to prevent overpressure and depression (implosion), and to ensure consistent extracorporeal flow rates [116]. On commencement, partial CPB is initiated using gravity drainage, then VAVD is started and its speed is increased progressively to reach the maximum active venous return, and venous return augmented by applying a monitored negative pressure of approximately 40 mmHg. Pressures >70 mmHg can cause the chattering phenomenon with incomplete blood drainage by the venous cannulae. The blood can be sucked by the pulmonary artery vent, which has a pressure relief valve that prevents excessive negative pressure. The amount of blood aspirated through this vent is an indicator of optimal venous cannula positioning, with flows <100 ml/min indicating complete CPB support [111]. LaPietra et al. [117] examined the potential for the transmission of air emboli with VAVD or KAVD. They concluded 27 that a centrifugal pump had air-handling disadvantages when used for KAVD alone, but when used as an arterial pump in combination with VAVD it resulted in fewer emboli post arterial filter. So, the standard of practice for most centers is VAVD [118]. In vitro studies suggest that air embolization during CPB may be increased when blood entering the venous reservoir is turbulent, such as is found during low blood volume levels of the reservoir and high pump flow rates [119, 120]. VAVD at 40 mmHg does not significantly increase gaseous microemboli activity when compared with gravity siphon venous drainage at 4 L/min flow rates [121]. When used with appropriate care, VAVD does not appear to significantly increase air microemboli and is not associated with an increased neurological risk following valvular surgery [122, 123]. VAVD at 40 mmHg is a safe, simple, and effective technique in cases of minimally invasive cardiac surgery; when used with appropriate care, it does not appear to significantly increase air microemboli and is not associated with increased neurological risks following valvular surgery [111]. Air removal is particularly difficult in robotic cardiac surgery. The cardiac apex cannot be elevated, and difficulty exists in manipulating the heart. The intracardiac air tends to be retained along dorsal interventricular septum and right pulmonary veins [38]. Use of CO2 insufflation into the hemithorax tends to displace any air from the exposed areas of the heart and this is supplemented by hand ventilation to expel air from the pulmonary veins. Weaning off CPB is done after resume of double-lung ventilation and under TEE guidance following standard practices as for the type of surgery with conventional CPB. The femoral artery and vein are closed primarily, and the RIJV line is removed and pressure is held. 2.11 Aortic Occlusion and Cardioplegia Protection of the myocardium from prolonged cross-clamp and bypass times can be performed using transthoracic aortic clamp (Fig. 2.7), or using the endoaortic balloon occlusion (Fig. 2.8). The transthoracic aortic cross-clamp (Chitwood clamp) is passed through an incision in the right axilla and applied to the ascending aorta, and care should be taken not to injure the pulmonary artery or the left atrial appendage [124]. Standard antegrade cold blood cardioplegia solution provides reliable myocardial protection. The transthoracic clamp has been shown to be less expensive, and decrease operating time with fewer complications than the endoaortic balloon method [125, 126]. We have had no aortic injuries from the transthoracic clamp in over 400 cases. This method has resulted in great success with no ensuing complications [127]. Nevertheless, for most ASD repair operations, we use the technique of beating heart without cross-clamping the 28 Fig. 2.7 The transthoracic aortic cross-clamp Fig. 2.8 The endoaortic balloon occlusion catheter system aorta. It is shown that to perform on-pump ASD repairs on the beating heart without cross-clamping the aorta is feasible, safe, and effective [128]. Alternatively, the endoaortic catheter system includes a 17F or 21F Remote Access Perfusion catheter (Fig. 2.8) with an aortic occlusion balloon, and it functions as an aortic cross clamp and antegrade cardioplegia delivery, and for active suctioning and deairing at the termination of CPB. The major advantage of this system is for redoing operations [110]. The endoaortic clamp inflated to a pressure of greater than 300 mmHg usually provides complete occlusion of the aorta [129] and antegrade cardioplegia is delivered. The aortic cannula is positioned in the ascending aorta, 2 cm above the aortic valve, with TEE guidance. The endoaortic balloon is inflated with a volume equal to the G. Wang and C. Gao diameter of the sinotubular junction of the aorta. Residual flow around the balloon can be seen and monitored with color flow on TEE. Pump flows may need to be reduced during cross clamping for both transthoracic and endoaortic, for proper placement and prevention of damage to the aorta. The endoaortic balloon catheter may be exchanged, if it for example ruptures accidentally, which may happen especially in mitral surgery when placing sutures in the mitral ring. When this happens, the endoaortic balloon clamp immediately becomes insufficient. The balloon may be replaced. The balloon itself is less stable because it has to be re-positioned more often and requires an experienced surgeon for re-positioning [130]. The migration of the occlusion balloon can lead to obstruction of the innominate artery, causing cerebral hypoperfusion and neurological injury. The use of bilateral radial arterial lines is useful in detecting the migration of the occlusion balloon toward the innominate artery. Occasionally the balloon may migrate proximally obstructing the coronary arteries, causing myocardial dysfunction [131]. Proximal migration of the balloon can be seen most easily with TEE, preventing balloon herniation through the aortic valve. Usually balloon migration does not lead to aortic valve dysfunction. The aortic root pressure should be maintained below the systemic arterial blood pressure to avoid balloon movement. Venting the heart properly and limiting cardioplegic flow are two strategies to avoid balloon migration. Use of the endoaortic balloon catheter should be avoided in heavily atherosclerotic aorta for fear of migration and embolization of plaque. Reichenspurner et al. [125] demonstrated increased morbidity, total operative and crossclamp times, and cost for the endoaortic balloon versus the transthoracic clamp. Aortic dissection is more common with the endoaortic balloon technique [132]. Early detection of aortic dissection by increased line pressure monitored by the perfusionist, a dissection membrane seen in echocardiography, or the surgeon’s direct vision, should always lead to immediate weaning from CPB and conversion to median sternotomy [130]. Improvements in design and use of the TEE for placement have reduced the complication rates for this device. Hypothermic ventricular fibrillation can be used when aortic access is limited, such as in reoperations. Deairing can be a problem with minimally invasive cardiac surgery. The flooding of CO2 into the surgical field has resulted in a decrease in air emboli [133, 134]. Suction on the aortic root cannula and TEE confirmation may also help to minimize emboli. As the necessary accompaniment, the anesthesiologist places an endopulmonary vent and endocoronary sinus catheter for retrograde cardioplegia through the RIJV [135–137] (Fig. 2.9). The endopulmonary vent catheter allows passive 2 Anesthesia for Robotic Cardiac Surgery 29 Endoaortic clamp Endocoronary sinus catheter Endopulmonary vent Endovenous drainage cannula Fig. 2.9 Diagrammatic representation of heartport endocoronary sinus catheter, endoaortic clamp, endopulmonary vent and endovenous drainage cannula venting of the pulmonary artery at approximately 50 ml/min. On inflating the endocoronary sinus catheter balloon a previously right atrial trace is changed to a right ventricular trace [38]. The use of a pulmonary vent catheter and an endocoronary sinus catheter is routinely but not mandatory. The cannulation of endocoronary sinus catheter for retrograde cardioplegia is the most complex manipulation that requires guide by the TEE and C-arm X-ray. 2.12 Summary • The status of endoscopic approaches is clear, but its future development is not predicted clearly. The da Vinci Surgical System as a new technology is being accepted by more and more surgeons. In the field of cardiac surgery, the administration of the da Vinci Surgical System possesses some particularity required to make more changes accordingly. Nifong and Chitwood [124] have reported in their editorial views regarding anesthesia and robotics: that a team approach with expertise in these procedures involving nurses, anesthesiologists, and surgeons with an interest in robotic procedures is required. Therefore, the learning and training are necessary for the operation team enabling the robotic cardiac surgery to be routinely achieved with standard methods. In Kernstine’s report [138], one among the recommendations to improve efficiency is the “use of an experienced anesthesiologist who can efficiently intubate and manage single-lung ventilation and hemodynamically support the patient during the procedure.” Finally, to summarize the clinical application and results of robotic cardiac surgery in recent years, using the opinion of Lehr et al. [56]: Early results of robotic cardiac surgical procedures are encouraging with evidence demonstrating fewer blood transfusions, shorter hospital stay, faster return to preoperative function levels, and improved quality of life compared with those having a sternotomy. • Robotic mitral valve repair and total endoscopic coronary artery bypass surgery have become standardized procedures at specialized centers. • Success of a robotic program is highly dependent on the skill sets, experience, and dedication of the entire team. • Stepwise progression of robotic technology and procedure development will continue to make robotic operations simpler and more efficient. References 1. Deeba S, Aggarwal R, Sain P, et al. Cardiac robotics: a review and St. Mary’s experiences. Int J Med Robot Comput Assist Surg. 2006;2:16–20. 2. Boehm D, Reichenspurner H, Gulbins H, et al. Early experience with robotic technology for coronary artery surgery. Ann Thorac Surg. 1999;68:1542–6. 3. LaPietra A, Grossi EA, Derivaux C, et al. Robotic-assisted instruments enhance minimally invasive mitral valve surgery. Ann Thorac Surg. 2000;70:835–8. 4. Wang G, Gao C, Zhou Q, et al. Anesthesia management of totally endoscopic atrial septal defect repair with a robotic surgical system. J Clin Anesth. 2011;23:621–5. 5. Haynes SR, Bonner S. Anaesthesia for thoracic surgery in children. Paediatr Anaesth. 2000;10:237–51. 6. Peden CJ, Prys-Roberts C. Capnothorax: implications for the anaesthetist. Anaesthesia. 1993;48:664–6. 7. Tobias JD. Anaesthetic implications of thoracoscopic surgery in children. Paediatr Anaesth. 1999;9:103–10. 8. Wang G, Gao C, Zhou Q, et al. Anesthesia management for robotically assisted endoscopic coronary artery bypass grafting on beating heart. Innovations (Phila). 2010;5:291–4. 9. Gibbs NM, Weightman WM, Thrackray NM, et al. The effects of recent aspirin ingestion on platelet function in cardiac surgery patients. J Cardiothorac Vasc Anesth. 2001;15:55–9. 10. Weightman WM, Gibbs NM, Weidmann CR, et al. The effect of preoperative aspirin-free interval on red blood cell transfusion requirements in cardiac surgical patients. J Cardiothorac Vasc Anesth. 2002;16:54–68. 11. Murkin JM. Anesthesia for robotic heart surgery: an overview. Heart Surg Forum. 2001;4:311–14. 12. Mishra YK, Wasir H, Sharma KK, et al. Totally endoscopic coronary artery bypass surgery. Asian Cardiovasc Thorac Ann. 2006;14:447–51. 13. Buggeskov KB, Wetterslev J, Secher NH, et al. Pulmonary perfusion with oxygenated blood or custodiol HTK solution during cardiac surgery for postoperative pulmonary function in COPD patients: a trial protocol for the randomized, clinical, parallel group, assessor and data analyst blinded Pulmonary Protection Trial. Trails. 2013;14:1–11. 14. Ku CM, Slinger P, Waddell T. A novel method of treating hypoxemia during one-lung ventilation for thoracoscopic surgery. J Cardiothorac Vasc Anesth. 2009;23:850–2. 15. Beck DH, Doepfmer UR, Sinemus C, et al. Effects of sevoflurane and propofol on pulmonary shunt fraction during one-lung ventilation for thoracic surgery. Br J Anaesth. 2001;86:38–43. 30 16. Sfez M. Basic physiology and anesthesia. In: Bax NMA, Georgeson KE, Naimaldin A, Valla JS, editors. Endoscopic surgery in children. 1st ed. Berlin: Springer; 1999. p. 53–70. 17. Wasnick JD, Hoffman WJ, Acuff T, et al. Anesthetic management of coronary artery bypass via minithoracotomy with video assistance. J Cardiothorac Vasc Anesth. 1995;9:731–3. 18. Pfitzner J, Peacock MJ, McAleer PT. Gas movement in the nonventilated lung at the onset of single-lung ventilation for videoassisted thoracoscopy. Anaesthesia. 1999;54:437–43. 19. Dalibon N, Moutafis M, Liu N, et al. Treatment of hypoxemia during one-lung ventilation using intravenous almitrine. Anesth Analg. 2004;98:590–4. 20. Silva-Costa-Gomes T, Gallart L, Valles J, et al. Low- vs high-dose almitrine combined with nitric oxide to prevent hypoxia during open-chest one-lung ventilation. Br J Anaesth. 2005;95:410–16. 21. Waheedullah K, Konrad S. Hypoxemia during one-lung ventilation: prediction, prevention, and treatment. Anesthesiology. 2009;110: 1402–11. 22. Hickling KG. Permissive hypercapnia. Respir Care Clin N Am. 2002;8:155–69. 23. Laffey JG, O’Croinin D, McLoughlin P, et al. Permissive hypercapnia role in protective lung ventilator strategies. Intensive Care Med. 2004;30:347–56. 24. Petrat G, Weyandt D, Klein U. Anesthetic considerations in pediatric laparoscopic and thoracoscopic surgery. Eur J Pediatr Surg. 1999;9:282–5. 25. Tobias JD. Anaesthesia for minimally invasive surgery in children. Best Pract Res Clin Anaesthesiol. 2002;16:115–30. 26. Unzueta MC, Casas JI, Moral MV. Pressure-controlled versus volume-controlled ventilation during one-lung ventilation for thoracic surgery. Anesth Analg. 2007;104:1029–33. 27. Benumof JL. Anesthesia for thoracic surgery. 2nd ed. Philadelphia: WB Saunders Company; 1995. 28. Nagendran J, Stewart K, Hoskinson M, et al. An anesthesiologist’s guide to hypoxic pulmonary vasoconstriction: implications for managing single-lung anesthesia and atelectasis. Curr Opin Anaesthesiol. 2006;19:34–43. 29. Sato M, Muraji T, Asai T, et al. Hemodynamic effects of carbon dioxide insufflation of the thoracic cavity during thoracoscopic surgery. Pediatr Endosurg Innov Tech. 2002;6:185–9. 30. Tobias JD. Anesthetic management for pediatric laparoscopy and thoracoscopy. In: Lobe TE, Schropp KP, editors. Pediatric laparoscopy and thoracoscopy. 1st ed. Philadelphia: WB Saunders Company; 1994. p. 59–66. 31. Jones DR, Greaber GM, Tanguilig GG, et al. Effects of insufflation on hemodynamics during thoracoscopy. Ann Thorac Surg. 1993;55:1379–82. 32. Hammer GB, Harrison TK, Vricella LA, et al. Single lung ventilation in children using a new paediatric bronchial blocker. Paediatr Anaesth. 2002;12:69–72. 33. Brock H, Rieger R, Gabriel C, et al. Hemodynamic changes during thoracoscopic surgery. Anaesthesia. 2000;55:10–6. 34. Gentili A, Lima M, Derose R, et al. Thoracoscopy in children: anaesthesiological implications and case reports. Minerva Anestesiol. 2007;73:161–71. 35. Hammer GB, Fitzmaurice BG, Brodsky JB. Methods for singlelung ventilation in pediatric patients. Anesth Analg. 2000;91: 248–52. 36. D’Attellis N, Loulmet D, Carpentier A. Robotic-assisted cardiac surgery: anesthetic and postoperative considerations. J Cardiothorac Vasc Anesth. 2002;16:397–400. 37. Sugantha G. Anaesthesia for minimally invasive cardiac surgery. Best Pract Clin Anaesthesiol. 2002;16:63–80. 38. Chauhan S, Sukesan S. Anesthesia for robotic cardiac surgery: an amalgam of technology and skill. Ann Card Anaesth. 2010;13: 169–75. G. Wang and C. Gao 39. Reves JG, Glass PS, Lubarsky DA, et al. Intravenous anesthetics. In: Miller RD, Eriksson LI, Fleisher LA, et al., editors. Miller’s anesthesia. 7th ed. Philadelphia: Churchill Livingstone; 2009. p. 719–68. 40. Howie MB, Gravlee GP. Induction of anesthesia. In: Hansler Jr FA, Martin DE, Gravlee GP, editors. A practical approach to cardiac anesthesia. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 164–75. 41. Thomson IR, Harging G, Hudson RJ. A comparison of fentanyl and sufentail in patients undergoing coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2002;14:652–6. 42. Howie MB, Cheng D, Newman MF, et al. A randomized doubleblinded multicenter comparison of remifentanil versus fentanyl when combined with isoflurane/propofol for early extubation in coronary artery bypass graft surgery. Anesth Analg. 2001;92: 1084–93. 43. Howie MB, Michelson LG, Hug Jr CC, et al. Comparison of three remifentanil dose-finding regimens for coronary artery surgery. J Cardiothorac Vasc Anesth. 2003;17:51–9. 44. Geisler FE, de Lange S, Royston D, et al. Efficacy and safety of remifentanil on coronary artery bypass graft surgery: a randomized, double-blind dose comparison study. J Cardiothorac Vasc Anesth. 2003;17:60–8. 45. Cheng DC, Newman MF, Duke P, et al. The efficacy and resource utilization of remifentanil and fentanyl in fast-track coronary artery bypass graft surgery: a prospective randomized, double-blinded controlled, multi-center trial. Anesth Analg. 2001;92:1093–102. 46. Myles PS, Hunt JO, Fletcher H, et al. Remifentanil, fentanyl, and cardiac surgery: a double-blinded, randomized controlled trial of costs and outcomes. Anesth Analg. 2002;95:805–12. 47. Maitre PO, Funk B, Crevoisier C, et al. Pharmacokinetics of midazolam in patients recovering from cardiac surgery. Eur J Clin Pharmacol. 1989;37:161–6. 48. Engoren MC, Kraras C, Garzia F. Propofol-based versus fentanylisoflurane-bases anesthesia for cardiac surgery. J Cardiothorac Vasc Anesth. 1998;12:177–81. 49. Cason BA, Gamperl AK, Slocum RE, et al. Anesthetic-induced preconditioning: previous administration of isoflurane decreases myocardial infarct size in rabbits. Anesthesiology. 1997;87:1182–90. 50. Landoni G, Bignami E, Oliviero F, et al. Halogenated anesthetics and cardiac protection in cardiac and non-cardiac anesthesia. Ann Cardiac Anesthesia. 2009;12:4–9. 51. Landoni G, Calabrò MG, Marchetti C, et al. Desflurane versus propofol in patients undergoing mitral valve surgery. J Cardiothorac Vasc Anesth. 2007;21:672–7. 52. London MJ, Mittnacht A, Kaplan JA. Anesthesia for myocardial revascularization. In: Kaplan JA, editor. Essentials of cardiac anesthesia. Philadelphia: Saunders Elsevier; 2008. p. 293–326. 53. Berntman L, Rosberg B, Shweikh I, et al. Atracurium and pancuronium in renal insufficiency. Acta Anaesthesiol Scand. 1989;33: 48–52. 54. Campos JH. Progress in lung separation. Thorac Surg Clin. 2005;15:71–83. 55. Gao C, Yang M, Wang G, et al. Totally robotic resection of myxoma and atrial septal defect repair. Interact Cardiovasc Thorac Surg. 2008;7:947–50. 56. Lehr EJ, Rodriguez E, Chitwood WR. Robotic cardiac surgery. Curr Opin Anaesthesiol. 2011;24:77–85. 57. Nifong LW, Chu VF, Bailey B, et al. Robotic mitral valve repair: experience with the da Vinci system. Ann Thorac Surg. 2003;75:438–43. 58. Pandey R, Garg R, Chandralekha R. Robot-assisted thoracoscopic thymectomy: perianaesthetic concerns. Eur J Anaesthesiol. 2010;27:473–7. 59. Campos JH. An update on robotic thoracic surgery and anesthesia. Curr Opin Anaesthesiol. 2010;23:1–6. 2 Anesthesia for Robotic Cardiac Surgery 60. Geddes LA, Tacker WA, Rosborough J, et al. Electrical dose for ventricular defibrillation of small and large animals using precordial electrodes. J Clin Invest. 1974;53:310–19. 61. Zipes DP, Fischer J, King RM, et al. Termination of ventricular fibrillation in dogs by depolarizing a critical amount of myocardium. Am J Cardiol. 1975;36:37–44. 62. Lateef F, Lim SH, Anantharaman V, et al. Changes in chest electrode impedance. Am J Emerg Med. 2000;18:381–4. 63. Deakin CD, McLaren RM, Petley GW, et al. Effects of positive endexpiratory pressure on transthoracic impedance-implications for defibrillation. Resuscitation. 1998;37:9–12. 64. Furman S. Defibrillation threshold and pneumothorax. Pacing Clin Electrophysiol. 1998;21:337–8. 65. Schuchert A, Hoffmann M, Steffgen F, et al. Several unsuccessful internal and external defibrillations during active can ICD implantation in a patient with pneumothorax. Pacing Clin Electrophysiol. 1998;21:471–3. 66. Luria D, Stanton M, Eldar M, et al. Pneumothorax: an unusual cause of ICD defibrillation failure. Pacing Clin Electrophysiol. 1998;21:474–5. 67. Cohen TJ, Lowenkron DD. The effects of pneumothorax on defibrillation thresholds during pectoral implantation of an active can implantable cardioverter defibrillator. Pacing Clin Electrophysiol. 1998;21:468–70. 68. Hatton KW, Kilinski LC, Ramaiah C, et al. Multiple failed External defibrillation attempts during robot-assisted internal mammary harvest for myocardial revascularization. Anesth Analg. 2006;103:1113–14. 69. Parr KG, Talamini MA. Anesthetic implications of the addition of an operative robot for endoscopic surgery: a case report. J Clin Anesth. 2002;14:228–33. 70. Loulmet D, Carpentier A, D’Attellis N, et al. Endoscopic coronary artery bypass grafting with the aid of robotic-assisted instruments. J Thorac Cardiovasc Surg. 1999;118:4–11. 71. Ascione R, Lloyd CT, Underwood MJ, et al. Inflammatory response after coronary revascularization with or without cardiopulmonary bypass. Ann Thorac Surg. 2000;69:1198–204. 72. Mack MJ. Minimally invasive and robotic surgery. JAMA. 2001;285:568–72. 73. Srivastava S, Gadasalli S, Agusala M, et al. Robotically assisted beating heart totally endoscopic coronary artery bypass (TECAB). Is there a future? Innovations (Phila). 2008;3:52–8. 74. Argenziano M, Katz M, Bonatti J, et al. Results of the prospective multicenter trial of robotically assisted totally endoscopic coronary artery bypass grafting. Ann Thorac Surg. 2006;81: 1666–75. 75. Kappert U, Cichon R, Schneider J, et al. Technique of closed chest coronary artery surgery on the beating heart. Eur J Cardiothorac Surg. 2001;20:765–9. 76. Murry CE, Richard VJ, Relmer KA, et al. Ischemlc preconditioning slows energy metabolism and delays ultrastructural damage during a sustained ischemic episode. Circ Res. 1990;66:913–31. 77. Vassiliades Jr TA. The cardiopulmonary effects of single-lung ventilation and carbon dioxide insufflation during thoracoscopic internal mammary artery harvesting. Heart Surg Forum. 2002;5: 22–4. 78. Dogan S, Aybek T, Andreen E, et al. Totally endoscopic coronary artery bypass grafting on cardiopulmonary bypass with robotically enhanced telemanipulation: report of forty-five cases. J Thorac Cardiovasc Surg. 2002;123:1125–31. 79. Vassiliades Jr TA, Rogers EW, Nielsen JL, et al. Minimally invasive direct coronary artery bypass grafting: Intermediate-term results. Ann Thorac Surg. 2000;70:1063–5. 80. Athanasiou T, Ashrafian H, Rowland SP, et al. Robotic cardiac surgery: advanced minimally invasive technology hindered by barriers to adoption. Future Cardiol. 2011;7:511–22. 31 81. Suri RM, Burkhart HM, Rehfeldt KH, et al. Robotic mitral valve repair for all categories of leaflet prolapse: improving patient appeal and advancing standard of care. Mayo Clin Proc. 2011; 86:838–44. 82. Kypson AP, Nifong LW, Chitwood WR. Robotic mitral valve surgery. Surg Clin North Am. 2003;83:1387–403. 83. Suri RM, Antiel RM, Burkhart HM, et al. Quality of life after early mitral valve repair using conventional and robotic approaches. Ann Thorac Surg. 2012;93:761–9. 84. Rodriguez E, Chitwood WR. Robotics in cardiac surgery. Scand J Surg. 2009;98:120–4. 85. Slinger P, Suissa S, Triolet W. Predicting arterial oxygenation during one lung anaesthesia. Can J Anaesth. 1992;39:1030–5. 86. Schwarzkopf K, Klein U, Schreiber T, et al. Oxygenation during one-lung ventilation: The effects of inhaled nitric oxide and increasing levels of inspired fraction of oxygen. Anesth Analg. 2001;92:842–7. 87. Marshall BE, Marshall C, Frasch F, et al. Role of hypoxic pulmonary vasoconstriction in pulmonary gas exchange 1: Physiological concepts. Intensive Care Med. 1994;20:291–7. 88. Benumof J. Conventional and differential lung management of one-lung ventilation. In: Anesthesia for thoracic surgery. 2nd ed. Philadelphia: Saunders; 1994. p. 413–24. 89. Brodsky J, Fitzmaurice B. Modern anesthetic techniques for thoracic operations. World J Surg. 2001;25:162–6. 90. Cheng W, Fontana GP, De Robertis MA, et al. Is robotic mitral valve repair a reproducible approach? J Thorac Cardiovasc Surg. 2010;139:628–33. 91. Vernick WJ, Woo JY. Anesthetic considerations during minimally invasive mitral valve surgery. Semin Cardiothorac Vasc Anesth. 2012;16:11–24. 92. Nuttall GA, Cook DJ, Fulgham JR, et al. The relationship between cerebral blood flow and transcranial Doppler blood flow velocity during hypothermic cardiopulmonary bypass in adults. Anesth Analg. 1996;82:1146–51. 93. Apostolakis E, Filos KS, Koletsis E, et al. Lung dysfunction following cardiopulmonary bypass. J Card Surg. 2010;25:47–55. 94. Siepe M, Goebel U, Mecklenburg A, et al. Pulsatile pulmonary perfusion during cardiopulmonary bypass reduces the pulmonary inflammatory response. Ann Thorac Surg. 2008;86:115–22. 95. Kottenberg-Assenmacher E, Kamler M, Peters J. Minimally invasive endoscopic port-access intracardiac surgery with one lung ventilation: impact on gas exchange and anaesthesia resources. Anaesthesia. 2007;62:231–8. 96. Hill GE, Whitten CW, Landers DF. The influence of cardiopulmonary bypass on cytokines and cell-cell communication. J Cardiothorac Vasc Anesth. 1997;11:367–75. 97. Shastri KA, Logue GL, Stern MP, et al. Complement activation by heparin-protamine complexes during cardiopulmonary bypass: effect of C4A null allele. J Thorac Cardiovasc Surg. 1997;114: 482–8. 98. Yadav R, Chaturvedi A, Rath GP, et al. Application of indigenous continuous positive airway pressure during one lung ventilation for thoracic surgery. Saudi J Anaesth. 2011;5:438–9. 99. Karzai W, Schwarzkopf K. Hypoxemia during one-lung ventilation prediction, prevention, and treatment. Anesthesiology. 2009;110:1402–11. 100. Gamoso MG, Phillips-Bute B, Landolfo KP, et al. Off-pump versus on-pump coronary artery bypass surgery and postoperative renal dysfunction. Anesth Analg. 2000;91:1080–4. 101. Mourisse J, Booil L. Bispectral index detects period of cerebral hypoperfusion during cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2003;17:76–8. 102. Sebel PS. Central venous system monitoring during open heart surgery: an update. J Cardiothorac Vasc Anesth. 1998; 12:3–8. 32 103. Schachner T, Bonaros N, Bonatti J, et al. Near infrared spectroscopy for controlling the quality of distal leg perfusion in remote access cardiopulmonary bypass. Eur J Cardiothorac Surg. 2008;34:1253–4. 104. Sobieski MA, Slaughter MS, Hart DE, et al. Peripheral cardiopulmonary bypass with modified assisted venous drainage and transthoracic aortic crossclamp: optimal management for robotic mitral valve repair. Perfusion. 2003;18:307–11. 105. Bonatti J, Garcia J, Rehman A, et al. On-pump beating-heart with axillary artery perfusion: a solution for robotic totally endoscopic coronary artery bypass grafting? Heart Surg Forum. 2009;12: E131–3. 106. Nifong LW, Chitwood WR, Pappas PS, et al. Robotic mitral valve surgery: a United States multicenter trial. J Thorac Cardiovasc Surg. 2005;129:1395–404. 107. Casselman F, Van Slycke S, Wellens F, et al. Mitral valve surgery can now routinely be performed endoscopically. Circulation. 2003;108 Suppl 1:II48–54. 108. Greelish J, Cohn L, Leacche M, et al. Minimally invasive mitral valve repair suggests earlier operations for mitral valve disease. J Thorac Cardiovasc Surg. 2003;126:365–71. 109. Muhs B, Galloway A, Lombino M, et al. Arterial injuries from femoral artery cannulation with port access cardiac surgery. Vasc Endovascular Surg. 2005;39:153–8. 110. Kiaii B, Bainbridge D, Fernandes P. Surgical, anesthetic, perfusion-related advances in minimal access surgery. Semin Cardiothorac Vasc Anesth. 2007;11:282–7. 111. Colangelo N, Torracca L, Lapenna E, et al. Vacuum-assisted venous drainage in extrathoracic cardiopulmonary bypass management during minimally invasive cardiac surgery. Perfusion. 2006;21:361–5. 112. Munster K, Anderson U, Mikkelsen J, et al. Vacuum assisted venous drainage (VAVD). Perfusion. 1999;14:419–23. 113. Tatooles AJ, Pappas PS, Gordon PJ, et al. Minimally invasive mitral valve repair using the da Vinci robotic system. Ann Thorac Surg. 2004;77:1978–84. 114. Cirri S, Negri L, Babbini M, et al. Haemolysis due to active venous drainage during cardiopulmonary bypass: comparison of two different techniques. Perfusion. 2001;16:313–18. 115. Wilcox T, Mitchell S, Gorman D. Venous air in the bypass circuit: a source of arterial line emboli exacerbated by vacuum-assisted drainage. Ann Thorac Surg. 1999;68:1285–9. 116. Almany DK, Sistino JJ. Laboratory evaluation of the limitations of positive pressure safety valves on hardshell venous reservoirs. J Extra Corpor Technol. 2002;34:115–17. 117. LaPietra A, Grossi EA, Pua BB, et al. Assisted venous drainage presents risk of undetected air microembolism. J Thorac Cardiovasc Surg. 2000;120:856–63. 118. Jones TJ, Deal DD, Vernon JC, et al. Does vacuum-assisted venous drainage increase gaseous microemboli during cardiopulmonary bypass? Ann Thorac Surg. 2002;74:2132–7. 119. Markus H. Transcranial Doppler detection of circulating cerebral emboli. A review. Stroke. 1993;24:1246–50. 120. Mathan HJ, Parlea L, Dupuis JY, et al. Safety of deliberate intraoperative and postoperative hypothermia for patients undergoing coronary artery surgery: a randomized trial. J Thorac Cardiovasc Surg. 2004;127:1270–5. G. Wang and C. Gao 121. Colangelo N, Torracca L, Lapenna E, et al. Vacuum assisted venous drainage during peripheral cardiopulmonary bypass. Presented at the eleventh European Congress on extra-corporeal circulation technology. Orosei, Italy, 8–11 June 2005, abstract book, p. 31. 122. Wang S, Undar A. Vacuum-assisted venous drainage and gaseous microemboli in cardiopulmonary bypass. J Extra Corpor Technol. 2008;40:249–56. 123. Carrier M, Cyr A, Voisine P, et al. Vacuum-assisted venous drainage does not increase the neurological risk. Heart Surg Forum. 2002;5:285–8. 124. Nifong LW, Chitwood WR. Challenges for the anesthesiologist: robotics? Anesth Analg. 2003;96:1–2. 125. Reichenspurner H, Detter C, Deuse T, et al. Video and roboticassisted minimally invasive mitral valve surgery: a comparison of the port-access and transthoracic clamp techniques. Ann Thorac Surg. 2005;79:485–90. 126. Mohr FW, Falk V, Diegeler A, et al. Minimally invasive portaccess mitral valve surgery. J Thorac Cardiovasc Surg. 1998;115: 567–76. 127. Gao C, Yang M, Xiao C, et al. Robotically assisted mitral valve replacement. J Thorac Cardiovasc Surg. 2012;143:S64–7. 128. Gao C, Yang M, Wang G, et al. Totally endoscopic robotic atrial septal defect repair on the beating heart. Heart Surg Forum. 2010;13:E155–8. 129. Reichenspurner H, Boehm DH, Gulbins H, et al. Threedimensional video and robot-assisted port-access mitral valve operation. Ann Thorac Surg. 2000;69:1176–81. 130. Wimmer-Greinecker G, Dzemali O, Aybek T, et al. Perfusion strategies for totally endoscopic cardiac surgery. Multimedia manual of cardiothoracic surgery 2006, October 9 (http://mmcts. ctsnetjournals.org/). 131. Goswami S, Nishanian E, Mets B. Anesthesia for robotic surgery. In: Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL, editors. Miller’s anesthesia. 7th ed. Philadelphia: Churchill Livingstone; 2009. p. 2389–403. 132. Jones B, Krueger S, Howell D, et al. Robotic mitral valve repair: a community hospital experience. Tex Heart Inst J. 2005;32:143–6. 133. Webb WR, Harrison Jr LH, Helmcke FR, et al. Carbon dioxide field flooding minimizes residual intracardiac air after open heart operations. Ann Thorac Surg. 1997;64:1489–91. 134. Woo YJ, Nacke EA. Robotic minimally invasive mitral reconstruction yields less blood product transfusion and shorter length of stay. Surgery. 2006;140:263–7. 135. Toomasian J, Peters W, Siegel L, et al. Extracorporeal circulation for port-access cardiac surgery. Perfusion. 1997;12:83–91. 136. Toomasian J, Williams D, Colvin S, et al. Perfusion during coronary and mitral valve surgery utilizing minimally invasive port-access technology. J Extra Corpor Technol. 1997;29: 67–72. 137. Reichenspurner H, Boehm DH, Welz A, et al. Minimally invasive coronary artery bypass grafting: port-access approach versus offpump techniques. Ann Thorac Surg. 1998;66:1036–40. 138. Kernstine KH, DeArmond DT, Shamoun DM, et al. The first series of completely robotic esophagectomies with three-field lymphadenectomy: initial experience. Surg Endosc. 2007;21: 2285–92. 3 Intraoperative Transesophageal Echocardiography in Robotic Cardiac Surgery Yao Wang and Changqing Gao Abstract Robotic cardiac surgery is a new surgical technique that uses small incisions. Previous studies have proved that intraoperative transesophageal echocardiography (TEE) plays an important role in conventional cardiac surgery with a median sternotomy incision. Intraoperative TEE is also useful in robotic cardiac surgery. Intraoperative TEE allows us: (1) to confirm the preoperative diagnosis before CPB; (2) to guide correct placement of the cannulae in the IVC, SVC, and AAO during establishment of peripheral CPB; (3) and to assess immediately the surgical results after weaning from CPB. Therefore, intraoperative TEE is a valuable adjunct in robotic cardiac surgery. 3.1 Introduction Conventional cardiac surgery operations have been performed through a median sternotomy, which provides extensive exposure of the operative field and allows ample access to all cardiac structures and proximal great vessels. During the early days of minimally invasive cardiac surgery, attempts to operate through small incisions were hindered by the absence of appropriate accessory technology, such as cardiopulmonary bypass, vascular cannulation, visualization systems, and instrumentation. Advances in closed-chest cardiopulmonary bypass, myocardial protection, improved intracardiac visualization, and robotic telemanipulation, have hastened the shift toward minimally invasive endoscopic cardiac surgery. Currently, complex mitral valve surgery, atrial septal defect repair, and atrial masses removal can be performed through small incisions using robotic assistance. Previous reports have demonstrated the importance of intraoperative transesophageal echocardiography (TEE) for conventional cardiac Y. Wang, MD • C. Gao, MD (*) Department of Cardiovascular Surgery, PLA General Hospital, No. 28 Fuxing Road, Beijing 100853, People’s Republic of China e-mail: gaochq301@yahoo.com surgery operations [1–5]. Intraoperative TEE has also gained wide acceptance for the management of patients undergoing robotic cardiac surgery [6–9]. This chapter will document the role of intraoperative TEE in robotic MV surgery, atrial septal defect repair, and atrial mass removal. 3.2 Intraoperative Transesophageal Echocardiography in Robotic Mitral Valve Surgery Mitral valve (MV) surgery has advanced dramatically over the past decades [10–13]. Conventional MV surgery has been performed through a median sternotomy, which provides extensive exposure of the operative field. Minimally invasive MV surgery has been used with technical advances in cardiopulmonary perfusion, valve exposure, myocardial preservation, instrumentation, and robotic telemanipulation [10–12, 14–17]. Currently, complex MV repair or replacement can be performed through port incisions with the use of robotic assistance [18, 19]. Previous reports have demonstrated the importance of intraoperative TEE for conventional MV surgery [20, 21], and recent data are available on the value of intraoperative TEE in robotic MV surgery [6, 7]. Intraoperative TEE is a valuable adjunct in robotic MV surgery. C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_3, © Springer Science+Business Media Dordrecht 2014 33 34 Y. Wang and C. Gao a b Fig. 3.1 TEE differentiation of degenerative MV disease: (a) Barlow’s disease with posterior leaflet prolapse (arrow): both leaflets are thick, bulky, and billowing (arrow); (b) Fibroelastic deficiency with P2 pro- 3.2.1 TEE Examination Before CPB Establishment After induction of anesthesia, a left-sided double-lumen endotracheal intubation and cannulation of the right internal jugular vein, the TEE probe is inserted into the mid esophagus. Before CPB, a systematic TEE examination is performed: (1) to analyze MV anatomy according to Carpentier’s pathophysiologic triad, which consists of valve etiology (i.e., the cause of the disease), valve lesions resulting from the disease, and valve dysfunction resulting from the lesions [22]; (2) to identify the precise localization of the leaflet dysfunction according to segmental valve analysis [23]; and (3) to evaluate the severity of the hemodynamic consequences according to published guideline [24, 25]. 3.2.1.1 Analysis of the MV Pathology Etiology The determination of the etiology of MV disease is important because it helps to predict the proper surgical intervention (valve repair or replacement) and expect complexity of the operation [26]. MV can be affected by numerous diseases and is the primary target in degenerative valve disease, rheumatic valve disease, and other uncommon diseases [26]. TEE is the gold standard for diagnosis and differentiation of degenerative MV disease [27]. Two main forms of degenerative MV disease (Barlow’s disease and fibroelastic deficiency) have unique differentiating characteristics on echocardiography [28]. Barlow’s disease is characterized by (1) excess leaflet tissue with large billowing and thickened leaflets; (2) prolapse of multiple leaflet segments that are usually involved; (3) chordae tendinae that tends to be thickened; (4) chordae elongation which is the most common lapse (arrow): both leaflets are thin and do not have billowing. A ruptured chord (arrow) is visible. AO aorta, LA left atrium, LV left ventricle, RA right atrium, RV right ventricle cause of prolapse; and (5) large annular size. In contrast, fibroelastic deficiency is characterized by (1) thin valve leaflets that do not show redundancy or billowing; (2) a single prolapsing segment; (3) occasional visible ruptured chordae; and (4) annular dilation that is less pronounced than that in Barlow’s disease [28] (Fig. 3.1). TEE can provide anatomic information on patients with rheumatic valve disease [26]. Mitral stenosis (MS) is the most frequent complication of rheumatic valve disease [26]. Commissural fusion is an important feature to distinguish rheumatic from degenerative MS [25]. Commissural fusion can be assessed from the short-axis view of MV. Commissures are better visualized using real-time or live 3D TEE [29] (Fig. 3.2). Valvular Lesions The valve lesions are critical data that a surgeon needs in order to define the best therapeutic strategy. In addition, the valve lesions may have great effect on the potential benefits of surgical intervention [27]. Any of the diseases previously mentioned can cause one or several lesions, which may affect one or several components of MV apparatus: the annulus, the leaflet, the chordae, the papillary muscles, and the ventricular wall. TEE can accurately assess MV lesions in patients with degenerative MV disease [30]. The following definitions are used: leaflet prolapse is defined as “any portion of the MV that moved above the mitral annulus during systole” [30]; leaflet billowing as “excess leaflet tissue protrudes into the atrium during systole with the free edge of the leaflets remaining in apposition below the plane of the MV annulus” [31]; chordae elongation as “the free edge of the leaflet is above the annular plane” [32]; chordae rupture as “the presence of free and highly mobile, linear echoes is associated with flail mitral leaflet” [33] (Fig. 3.3); annular dilatation as “the ratio of 3 Intraoperative Transesophageal Echocardiography in Robotic Cardiac Surgery a 35 b Fig. 3.2 Live 3D TEE shows commissures of the MV: (a) Commissures viewed from the left atrium; (b) Commissures viewed from the left ventricle. AO aorta, LAA left atrial appendage, MV mitral valve a b c d Fig. 3.3 TEE assessment of MV lesions: (a) leaflet prolapse; (b) leaflet billowing; (c) chordae elongation; (d) chordae rupture. AO aorta, LAA left atrial appendage, LA left atrium, LV left ventricle, RA right atrium, RV right ventricle 36 Fig. 3.4 Live 3D TEE shows the typical rheumatic MS: a “fish mouth” configuration annulus to anterior leaflet is greater than 1.3 or when the diameter of the annulus is greater than 35 mm” [34]. TEE can also accurately assess the valve and subvalvular apparatus in patients with MS due to rheumatic valve disease [26]. The pathological process of rheumatic MS causes commissural fusion, leaflet thickening and calcification, chordal fusion, or a combination of these processes [25]. Commissural fusion can be assessed from the short axis view of the MV; leaflet thickening from the mid esophageal long axis view; chordal fusion from the mid esophageal long-axis and fourchamber views. The typical rheumatic MS has a funnel shape and a small central orifice with a “fish mouth” configuration, which could be best visualized with live 3D TEE (Fig. 3.4). The Type of Dysfunction Assessing the type of dysfunction in MV disease is important for the surgeon to identify the lesions causing the dysfunction [31]. In normal motion of the leaflet, MV regurgitation is due to either leaflet perforation or abnormal leaflet coaptation. MV prolapse may be due to either chordae rupture or elongation. Restricted leaflet motion is seen in rheumatic MV disease or ischemic cardiomopathy. TEE is the principal diagnostic tool for the accurate evaluation of the dysfunction of the MV [23]. The “functional approach” of valvular disease is based on analysis of the motion of the leaflets by TEE and visual inspection during the operation [23]. Three functional types are described depending upon whether the motion of the leaflets is normal (type I), increased (typed II), or restricted (type III) (Fig. 3.5). Restricted leaflet motion may occur mainly during the opening of the valve (type IIIa) or during valve closure (type IIIb) [31]. Types I and II valve dysfunctions result in valve regurgitation whereas type III may result in valve regurgitation, stenosis, or both (Fig. 3.5). Y. Wang and C. Gao 3.2.1.2 Identification of the Precise Localization of Leaflet Dysfunction The functional classification of MV disease is refined by the addition of the “Segmental Analysis” which allows precise localization of the leaflet dysfunction [23]. In segmental valve analysis, the valvular apparatus is separated into eight segments. The three scallops of the posterior leaflet are identified as P1 (anterior scallop), P2 (middle scallop), and P3 (posterior scallop). The three corresponding segments of the anterior leaflet are termed as: A1 (anterior part), A2 (middle part), and A3 (posterior part). The remaining two segments are the anterior commissure and the posterior commissure [23]. MV is examined with TEE by using four mid-esophageal views (the mid-esophageal four-chamber view, the commissural view, the two-chamber view, and the long-axis view) [35] and the transgastric basal short-axis view [36] (Fig. 3.6). The transgastric basal short-axis view is obtained at a multiplane angle of 0°–20° by anteflexing and withdrawing the probe at the level of the base of LV. The view provides the MV short axis view, with P3 being the closest to the apex of the sector [36]. The recent development of a fully sampled matrix-array TEE transducer (Philips Medical Systems, Andover, MA) allows excellent real-time imaging of MV in three dimensions [37] (Fig. 3.7). 3.2.1.3 Evaluation of the Severity of the Hemodynamic Consequences Assessing the severity of hemodynamic consequences is an important complement to functional valve analysis, and it is essential for clinical decision-making [24, 25]. The severity of MS is assessed according to published guidelines [25]. Routine evaluation of MS severity should combine measurements of mean gradient and MV area using planimetry and the T1/2 method. In case of discrepancy, the result of planimetry is the reference measurement, except with poor acoustic windows. MV stenosis is graded as being mild, moderate, and severe. The severity of MV regurgitation is assessed according to published guidelines [24]. A comprehensive approach to the evaluation of the severity of MV regurgitation is required which integrates multiple parameters. Specific signs related to MV anatomy (regurgitant jet area, vena contracta width, flow convergence, pulmonary vein flow) along with supportive signs (pulmonary vein flow, peak mitral E velocity, and regurgitation jet profile) constitute the basic features of an integrated assessment. These specific signs include color flow jet area, mitral inflow, jet density, jet contour, pulmonary vein flow, and quantitative parameters regarding regurgitant volume, regurgitant fraction and effective regurgitant orifice area [24]. MV regurgitation is graded as being mild, moderate, and severe [24]. 3 Intraoperative Transesophageal Echocardiography in Robotic Cardiac Surgery 37 a b c Fig. 3.5 TEE evaluation of the dysfunction of the MV (left) and hemodynamics (right): (a) type I; (b) type II; (c) type IIIa; AAO ascending aorta, LA left atrium, LV left ventricle, RA right atrium, RV right ventricle 3.2.2 TEE-Guided Cannulation of Peripheral CPB Conventional cardiac surgery has been performed via median sternotomy, which provides optimal access to all cardiac structures and the great vessels and allows central cannulation for CPB under direct vision. To perform robotic cardiac procedures through small port sites, peripheral vessel cannulation for CPB has been used. [6]. TEE may provide direct visualization of the target vessels, guidewire and cannulae [38]. TEE may be useful in guiding successful placement of the cannulae in the inferior vena cava (IVC), superior vena cava (SVC), and ascending aorta (AAO) in the establishment of peripheral CPB during robotic cardiac surgery [8]. 38 Y. Wang and C. Gao a b c d Fig. 3.6 The mid-esophageal mitral valve views: (a) the mid-esophageal four-chamber view; (b) the commissural view; (c) the two-chamber view; (d) the long-axis view. AO aorta, LAA left atrial appendage, LA left atrium, LV left ventricle, RA right atrium, RV right ventricle a b Fig. 3.7 Live 3D imaging of the en face view of the mitral valve from the left atrial perspective (a) and left ventricle perspective (b) at enddiastole. AO aorta 3 Intraoperative Transesophageal Echocardiography in Robotic Cardiac Surgery a b c d 39 Fig. 3.8 TEE-Guided Cannulation of the Inferior Vena Cava: (a) the intrahepatic IVC view; (b) TEE shows the guidewire in the IVC; (c) TEE shows the guidewire in the RA; (d) TEE shows the cannula in the IVC. HV hepatic vein, IVC inferior vena cava, LA left atrium, LV left ventricle, RA right atrium 3.2.2.1 TEE-Guided Cannulation of the Inferior Vena Cava (IVC) The intrahepatic IVC view (70°–90°) and the mid-esophageal bicaval view (80°–110°) [36] are obtained in turn. A guidewire is inserted through a cutdown into the right femoral vein. Under TEE guidance, the guidewire is advanced into the IVC and then into the right atrium (RA) sequentially, and a femoral venous cannula (Medtronic, Inc, Minneapolis, MN, USA) is inserted over the guidewire with the distal end of the cannula parallel to the IVC wall and its distal tip positioned at or above the IVC/RA junction (Fig. 3.8). The guidewire is then removed. the cannula is removed, and an arterial cannula (Medtronic, Inc, Minneapolis, MN, USA) is inserted over the guidewire with the distal end of the cannula parallel to the SVC wall and its distal tip positioned at or above the SVC/RA junction (Fig. 3.9). The guidewire is then removed. 3.2.2.2 TEE-Guided Annulation of the Superior Vena Cava (SVC) The mid esophageal bicaval view (80°–110°) is obtained [36]. Under TEE guidance, the guidewire is advanced into RA via the cannula in the right internal jugular vein and then 3.2.2.3 TEE-Guided Cannulation of the Ascending Aorta (AAO) The mid-esophageal aortic valve long-axis view (120°–160°) is obtained [36]. After cross clamping of the AAO, an angiocath (a cannula adapted for antegrade administration of cardioplegic solution) (Becton Dickinson Infusion Therapy Systems Inc., Sandy Utah) is inserted into the AAO via the fourth intercostal space, with its distal tip located in the aortic root under TEE guidance. Color flow imaging is used to indicate whether the angiocath is following the appropriate course (Fig. 3.10), and rapid flush of the cardioplegic solution is used to identify the tip of the angiocath (Fig. 3.10). 40 a Y. Wang and C. Gao b Fig. 3.9 TEE-guided cannulation of the superior vena cava: (a) TEE shows the guidewire in the SVC; (b) TEE shows the cannula in the SVC. LA left atrium, LV left ventricle, RA right atrium, SVC superior vena cava a b c d Fig. 3.10 TEE-guided cannulation of the ascending aorta: (a) TEE shows an angiocath inserted into the AAO; (b) Rapid flush of the cardioplegic solution identifies the tip of the angiocath; (c) Color flow imaging indicates the course of the angiocath; (d) Surgical view shows the angiocath inserted into the AAO. AAO ascending aorta, LA left atrium, LV left ventricle, AV aortic valve 3 Intraoperative Transesophageal Echocardiography in Robotic Cardiac Surgery 3.2.3 TEE Examination After Pump-Off 41 a 3.2.3.1 Assessment of the Mitral Valve After Repair Immediately after weaning from CPB, TEE is performed to assess the results of MV repair, and to assess for residual MV regurgitation, restriction of MV opening with stenosis, and systolic anterior motion of the leaflets of the MV. Residual MV Regurgitation Confirming the absence of significant residual MV regurgitation is the most critical aspect of postoperative valve analysis by TEE [35]. Immediate repair results by TEE are essential in determining whether reintervention is warranted. Residual MV regurgitation evaluated by TEE should be attempted as much as possible to create representative loading conditions with volume or vasopressors to fully assess the adequacy of the MV repair immediately after the patient is weaned from CPB, because insufficient preload and low ventricular pressure will result in underestimation of residual MV regurgitation [39, 40]. Appropriate volume loading, and hemodynamic manipulations are necessary to adequately evaluate the repaired MV. The depth of coaptation should be documented and be at least 5 mm in a two-dimensional long-axis view to ensure adequacy of coaptation [39]. Mitral Stenosis (MS) Acute MS following MV repair is a rare but severe complication, and it is more likely to be seen with the Alfieri edge-toedge repair, commissuroplasty, and small annuloplasty ring [41, 42]. Intraoperative TEE can be utilized to diagnose iatrogenic MS immediately after MV repair. Continuous-wave Doppler gradients displaying a mean gradient greater than 7 mmHg or peak gradient greater than 17 mmHg is suggestive of clinically relevant MS after MV repair [41]. Systolic Anterior Motion (SAM) SAM of MV leaflets causes obstruction of dynamic left ventricular outflow tract (LVOT) which is a known complication of MV repair that may necessitate immediate additional surgical intervention [43–45]. TEE may demonstrate a characteristic systolic anterior motion of the MV into the LVOT. Doppler echocardiography is used to determine the peak gradient. Peak gradient across the LVOT is increased from baseline as a result of dynamic LVOT obstruction. When SAM occurs after MV repair, hemodynamic maneuvers must be attempted before the results are declared inadequate. SAM can be resolved with volume loading, increased afterload, and withdrawal of inotropic agents [45]. Aortic Valve Leaflet Injury The leaflets of the aortic valve may be inadvertently injured during percutaneous cannulation of the angiocath in the ascending aorta in the establishment of peripheral CPB. TEE b c Fig. 3.11 TEE shows perforated aortic valve with regurgitation: (a) discontinuity is noted in the RCC (arrow); (b) an accentric jet of AR through this region on color flow imaging; (c) after repair of the RCC, there is no residual AR can provide high-resolution images of the aortic valve and is helpful in determining the mechanism and cause of the injury immediately after CPB. Discontinuity in the leaflet of the aortic valve with an accentric jet of aortic regurgitation noted by TEE alerts the surgeon to perforated aortic valve (Fig. 3.11). 42 Y. Wang and C. Gao a b c d Fig. 3.12 Bileaflet mechanical valve (upper) and bioprosthetic valve (lower) in mitral position. TEE shows the opening (left) and closure (right) of the leaflets of the prosthetic valve (arrows). AO aorta, LA left atrium, LV left ventricle, RV right ventricle 3.2.3.2 Assessment of the Mitral Valve After Replacement Immediately after MV replacement, TEE is performed to verify normal leaflet or motion of occluders and to detect technical problems such as paravalvular regurgitation and left ventricular outflow tract obstruction. Confirmation of the Leaflet Motion The opening and closure of the leaflets of the prosthetic valve in the MV position can be confirmed by TEE. Leaflet motion is best visualized using the 2D TEE mid-esophageal long-axis views and live 3D-TEE en face view of the MV. In 2D-TEE mid-esophageal long-axis views, the two mechanical leaflets are open, producing two parallel linear shadows within a circular annulus, and close symmetrically to a tilt angle of 85°–90° (Fig. 3.12). In the live-3D TEE en face view of MV, the leaflets motion of mechanical and bioprosthetic valves are better visualized (Fig. 3.13). Confirmation of the Absence of Paravalvular Regurgitation TEE demonstrates small characteristic regurgitant jets during leaflet closure. Closure backflow is the reversal of flow required for closure of the valve. In contrast, leakage backflow occurs after closure of mechanical valves and originates from the hinges and the regions of coaptation between the occluders and the valve ring. Physiologic regurgitation jets are small and short in duration. Mild transvalvular or paravalvular regurgitation can often be detected by TEE immediately after implantation. Small, insignificant transvalvular or paravalvular leaks are commonly observed immediately after CPB (Fig. 3.14), and should not be a cause for concern [46]. Pathologic paravalvular regurgitation is caused by incomplete fixation of the prosthetic sewing ring to the native annulus or dehiscence of the sewing ring. Paravalvular regurgitant jets detected by TEE originate from the outside of the 3 Intraoperative Transesophageal Echocardiography in Robotic Cardiac Surgery a b c d 43 Fig. 3.13 Bileaflet mechanical valve (upper) and bioprosthetic valve (lower) in mitral position. Live-3D TEE en face view of the MV from the left atrial perspective (upper) and from the left ventricle perspective (lower) shows the opening (left) and closing (right) of the leaflets of the prosthetic valve (arrows). AO aorta sewing ring, and characteristically produce eccentric jets that track along the walls of the left atrium [47]. Intraoperative TEE is useful for detecting pathologic paravalvular regurgitation. Precise characterization of the location and severity of paravalvular regurgitation jets detected by TEE immediately after MV replacement may be useful for guiding decisions for surgical intervention [47]. LVOT image after MV replacement and to estimate the LVOT pressure gradient [50]. Dynamic Left Ventricular Outflow Tract (LVOT) Obstruction Dynamic LVOT obstruction is an uncommon, but is a recognized complication of MV replacement. [48] The valve sparing or chordal sparing technique used in MV replacement, may cause residual MV leaflet or chordal apparatus remaining in the LVOT, and result in LVOT obstruction [48, 49]. In addition, LVOT obstruction may also resulted from a porcine bioprosthesis in the mitral position with a strut impinging LVOT [50]. TEE can provide a means for Atrial septal defect (ASD) is one of the most common adult congenital heart defects. ASD types include: secundum ASD, primum ASD, superior sinus venosus defect, inferior sinus venosus defect, and unroofed coronary sinus [51]. Currently, ASD repair can be performed through port incisions with robotic assistance [52]. Previous studies have shown that intraoperative TEE was valuable in the perioperative care of patients with congenital heart defects [4]. Intraoperative TEE is also a valuable adjunct in robotic ASD repair. 3.3 Intraoperative Transesophageal Echocardiography in Robotic Atrial Septal Defect Repair 44 Y. Wang and C. Gao 3.3.1.1 Confirmation of the Preoperative Diagnosis TEE is the primary diagnostic imaging modality for ASD [53] (Fig. 3.15). TEE may be necessary to adequately visualize the atrial septum, because it provides exact localization and sizing of the ASD [54, 55]. The septum is thin and may not be visualized if the septum is parallel to the echocardiographic beam. To ensure proper visualization of the septum, the echocardiographic beam should be perpendicular to the septum. The shunt of blood that occurs with ASD can be evaluated with color-flow Doppler imaging [56] (Fig. 3.16). a 3.3.1.2 Ruling Out the Presence of Associated Lesions ASD can be associated with additional malformations, including anomalous pulmonary venous connection, persistent left SVC, pulmonary valve stenosis, and mitral valve prolapse [51]. TEE may be necessary to identify the lesions. b 3.3.2 During the Establishment of CPB Follow the same steps as previously discussed in Sect. 3.2.2. c 3.3.3 TEE Examination After Weaning from CPB Immediately following CPB, a thorough intraoperative TEE exam must also be performed (1) to assess the adequacy of the surgical repair; and (2) to rule out the complications of the surgical repair. Fig. 3.14 Mild transvalvular (upper) and paravalvular regurgitantion (middle) of mechanical and mild paravalvular regurgitation of bioprosthetic (lower) valve in the MV position, detected by TEE immediately after CPB. AO aorta, LA left atrium, LV left ventricle 3.3.1 TEE Examination Before CPB Prebypass TEE examination is performed: (1) to confirm the preoperative diagnosis; (2) to rule out the presence of associated lesions that may have a direct impact on surgical procedure. 3.3.3.1 Assessment of the Adequacy of the Surgical Repair The contributions of post-CPB TEE include assessment of the adequacy of the surgical repair (Fig. 3.16), evaluation of postrepair atrioventricular valve competence, and evaluation of ventricular function [57]. TEE may also reliably provide for immediate detection of suboptimal surgical repairs and significant postoperative residue [57], potentially improving the efficacy of the surgical repair. 3.3.3.2 Ruling Out Complications of Surgical Repair Post-CPB TEE examination may also be particularly important since repair of these defects, using a patch may involve the pulmonary veins, obstruct the IVC, or may not completely close the defect. In each of these instances, diagnosis should immediately be made by intraoperative TEE. 3 Intraoperative Transesophageal Echocardiography in Robotic Cardiac Surgery a 45 b Fig. 3.15 TEE in the mid-esophageal bicaval view demonstrating ASD: (a) secundum ASD; (b) superior sinus venosus defect. ASD atrial septal defect, LA left atrium, RA right atrium, SVC superior vena cava a b Fig. 3.16 Pre- and post-bypass TEE in patients with ASD: (a) colorflow Doppler imaging shows the shunt of blood that occurs with ASD; (b) there is no residual shunt at atrial level post ASD repair. ASD atrial septal defect, IAS interatrial septum, LA left atrium, RA right atrium, SVC superior vena cava 3.4 examination is important for the planning of incision and excision techniques. Intraoperative Transesophageal Echocardiography in Robotic Atrial Masses Removal Surgical removal of an intracardiac mass is the treatment of choice in many instances [58]. Currently, atrial mass removal can be performed through port incisions with robotic assistance [59]. Previous studies have shown that intraoperative TEE was useful toward a successful outcome during surgical removal of intracardiac masses [60]. Intraoperative TEE is a valuable adjunct in robotic atrial mass removal. 3.4.1 3.4.1.1 Confirmation of the Preoperative Diagnosis TEE gives a clear image and anatomical definition of the atrial mass [60]. TEE can characterize the location, size, shape, and mobility of the tumor [61]. Typical TEE displays characteristics of myxoma as having a rounded shape, smooth margins, and lack of laminated appearance (Fig. 3.17). Caution should be applied to appropriate patient selection because malignant tumors are unlikely to be removed with minimally invasive approaches [62]. TEE Examination Before CPB Prebypass TEE examination is performed to confirm the preoperative diagnosis, and to provide information about the attachment site of atrial masses. The pre-CPB TEE 3.4.1.2 Providing Information About the Attachment Site of Atrial Masses TEE may provide a definitive site of attachment (stalk) of the atrial masses, which is most frequently from the fossa ovalis 46 Y. Wang and C. Gao a b c d Fig. 3.17 Pre- and post-bypass TEE in patients with LA myxoma: (left) pre-bypass TEE demonstrating the myxoma attached to the interatrial septum (upper) and the root of the anterior leaflet of the of the interatrial septum [61]. The tumor’s site of attachment may have important implications for involvement of adjacent, and indirectly involved structures including the valve. In addition, identifying the location and extent of right atrial myxomas may be important for guiding the appropriate percutaneous cannulation of the IVC and SVC. 3.4.2 TEE Examination During CPB Establishment Follow the same steps as previously discussed in Sect. 3.2.2. 3.4.3 TEE Examination After Weaning from CPB Following resection of the mass, post-CPB TEE is necessary to evaluate the completeness of surgical removal and to assure that the interatrial septum is intact (Fig. 3.16). mitral valve (lower) via a narrow stalk (arrows); (right) post-bypass TEE confirming complete resection of the myxoma. AO aorta, IAS interatrial septum, LA left atrium, LV left ventricle, RA right atrium Conclusion Intraoperative TEE is especially useful in robotic cardiac surgery. Intraoperative TEE allows surgeons: (1) to confirm the preoperative diagnosis before CPB; (2) to guide correct placement of the cannulae in the IVC, SVC, and AAO during establishment of peripheral CPB; (3) and to assess immediately the surgical results after weaning from CPB. Therefore, intraoperative TEE is a valuable adjunct in robotic cardiac surgery. References 1. Omran AS, Woo A, David TE, Feindel CM, Rakowski H, Siu SC. Intraoperative transesophageal echocardiography accurately predicts mitral valve anatomy and suitability for repair. J Am Soc Echocardiogr. 2002;15(9):950–7. 2. Orihashi K, Matsuura Y, Ishihara H, Hamanaka Y, Kawaue Y, Sueda T, Kanehiro K, Nomimura T. Some advantages of transesophageal echocardiography during mitral valve replacement. Hiroshima J Med Sci. 1988;37(3):127–31. 3 Intraoperative Transesophageal Echocardiography in Robotic Cardiac Surgery 3. Milano A, Dan M, Bortolotti U. Left atrial myxoma: excision guided by transesophageal cross-sectional echocardiography. Int J Cardiol. 1990;27(1):125–7. 4. Tempe DK, Sharma S, Banerjee A, Sharma V, Ramamurthy P, Datt V. The utility of transesophageal echocardiography for detecting residual shunt in a patient undergoing atrial septal defect repair. Anesth Analg. 2007;104(4):777–8. 5. Yang SG, Novello R, Nicolson S, Steven J, Gaynor JW, Spray TL, Rychik J. Evaluation of ventricular septal defect repair using intraoperative transesophageal echocardiography: frequency and significance of residual defects in infants and children. Echocardiography. 2000;17(7):681–4. 6. Wang Y, Gao CQ, Wang JL, Yang M. The role of intraoperative transesophageal echocardiography in robotic mitral valve repair. Echocardiography. 2011;28(1):85–91. 7. Wang Y, Gao CQ, Xiao C, Yang M, Wang G, Wang J, Shen Y. Intraoperative transesophageal echocardiography in patients undergoing robotic mitral valve replacement. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2012;37(12):1264–9. Chinese. 8. Wang Y, Gao CQ, Wang G, Wang JL. Transesophageal echocardiography guided cannulation for peripheral cardiopulmonary bypass during robotic cardiac surgery. Chin Med J (Engl). 2012; 125(18):3236–9. 9. Sorrell VL, Rajeev AG, Nifong LW, Chu FV, Chitwood Jr WR. Intraoperative transesophageal echocardiography with a special focus on a patient undergoing advanced robotic-assisted procedures. Echocardiography. 2002;19(7 Pt 1):583–8. 10. Navia JL, Cosgrove DM. Minimally invasive mitral valve operations. Ann Thorac Surg. 1996;62(5):1542–4. 11. Kaneko Y, Kohno T, Ohtsuka T, Ohbuchi T, Furuse A, Konishi T. Video-assisted observation in mitral valve surgery. J Thorac Cardiovasc Surg. 1996;111(1):279–80. 12. Mohr FW, Falk V, Diegeler A, Walther T, van Son JAM, Autschbach R. Minimally invasive port-access mitral valve surgery. J Thorac Cardiovasc Surg. 1998;115(3):567–74. 13. Chitwood WR, Nifong LW, Elbeery JE, Chapman WH, Albrecht R, Kim V, Young JA. Robotic mitral valve repair: trapezoidal resection and prosthetic annuloplasty with the da Vinci surgical system. J Thorac Cardiovasc Surg. 2000;120(6):1171–2. 14. Chitwood WR, Wixon CL, Elbeery JR, Moran JF, Chapman WHH, Lust RM. Video-assisted minimally invasive mitral valve surgery. J Thorac Cardiovasc Surg. 1997;114(5):773–80. 15. Falk V, Walther T, Autschbach R, Diegeler A, Battellini R, Mohr FW. Robot-assisted minimally invasive solo mitral valve operation. J Thorac Cardiovasc Surg. 1998;115(2):470–1. 16. Felger JE, Chitwood R, Nifong LW, Holbert D. Evolution of mitral valve surgery: toward a totally endoscopic approach. Ann Thorac Surg. 2001;72(4):1203–8. 17. Mohr FW, Falk V, Diegeler A, Walther T, Gummert JF, Bucerius J, Jacobs S, Autschbach R. Computer-enhanced “robotic” cardiac surgery: experience in 148 patients. J Thorac Cardiovasc Surg. 2001;121(5):842–53. 18. Mehmanesh H, Henze R, Lange R. Totally endoscopic mitral valve repair. J Thorac Cardiovasc Surg. 2002;123(1):96–7. 19. Gao CQ, Yang M, Xiao C, Wang G, Wu Y, Wang J, Li J. Robotically assisted mitral valve replacement. J Thorac Cardiovasc Surg. 2012;143(4):S64–7. 20. Freeman WK, Schaff HV, Khandheria BK, Oh JK, Orszulak TA, Abel MD, Seward JB, Tajik AJ. Intraoperative evaluation of mitral valve regurgitation and repair by transesophageal echocardiography: incidence and significance of systolic anterior motion. J Am Coll Cardiol. 1992;20(3):599–609. 21. Reichert SL, Visser CA, Moulijn AC, Suttorp MJ, vd Brink RB, Koolen JJ, Jaarsma W, Vermeulen F, Dunning AJ. Intraoperative transesophageal color-coded Doppler echocardiography for 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 47 evaluation of residual regurgitation after mitral valve repair. J Thorac Cardiovasc Surg. 1990;100(5):756–61. Carpentier A, Chauvaud S, Fabiani JN, Deloche A, Relland J, Lessana A, D’Allaines C, Blondeau P, Piwnica A, Dubost C. Reconstructive surgery of mitral valve incompetence: ten-year appraisal. J Thorac Cardiovasc Surg. 1980;79(3):338–48. Carpentier AF, Lessana A, Relland JYM, Belli E, Mihaileanu S, Berrebi AJ, Palsky E, Loulmet DF. The physio-ring- an advanced concept in mitral-valve annuloplasty. Ann Thorac Surg. 1995;60(5):1177–85. Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16(7):777–802. Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, Iung B, Otto CM, Pellikka PA, Quinones M. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009;22(1):1–23. Bonow RO, Carabello BA, Chatterjee K, de Leon Jr AC, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O’Gara PT, O’Rourke RA, Otto CM, Shah PM, Shanewise JS, Smith Jr SC, Jacobs AK, Adams CD, Anderson JL, Antman EM, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B, American College of Cardiology/American Heart Association Task Force on Practice Guidelines. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease. Circulation. 2006;114(5):e84–231. Enriquez-Sarano R, Freeman WK, Tribouilloy CM, Orszulak TA, Khandheria BK, Seward JB, Bailey KR, Tajik AJ. Functional anatomy of mitral regurgitation – accuracy and outcome implications of transesophageal echocardiography. J Am Coll Cardiol. 1999;34(4):1129–36. Anyanwu AC, Adams DH. Etiologic classification of degenerative mitral valve disease: Barlow’s disease and fibroelastic deficiency. Semin Thorac Cardiovasc Surg. 2007;19(2):90–6. Schlosshan D, Aggarwal G, Mathur G, Allan R, Cranney G. Real-time 3D transesophageal echocardiography for the evaluation of rheumatic mitral stenosis. JACC Cardiovasc Imaging. 2011;4(6):508–88. Agricola E, Oppizzi M, De Bonis M, Maisano F, Toracca L, Bove T, Alfieri O. Multiplane transesophageal echocardiography performed according to the guidelines of the American Society of Echocardiography in patients with mitral valve prolapse, flail, and endocarditis: diagnostic accuracy in the identification of mitral regurgitant defects by correlation with surgical findings. J Am Soc Echocardiogr. 2003;16(1):61–6. Carpentier A. Cardiac valve surgery – the “French correction”. J Thorac Cardiovasc Surg. 1983;86(3):323–37. Duran CG. Surgical management of elongated chordae of the mitral valve. J Card Surg. 1989;4(3):253–9. Mintz GS, Kotler MN, Segal BL, Parry WR. Two-dimensional echocardiographic recognition of ruptured chordae tendineae. Circulation. 1978;57(2):244–50. Caldarera I, Vanherwerden LA, Taams MA, Bos E, Roelandt J. Multiplane transesophageal echocardiography and morphology of regurgitant mitral-valves in surgical repair. Eur Heart J. 1995;16(7): 999–1006. Troianos CA, Konstadt S. Evaluation of mitral regurgitation. Semin Cardiothorac Vasc Anesth. 2006;10(1):73–7. Shanewise JS, Cheung AT, Aronson S, Stewart WJ, Weiss RL, Mark JB, Savage RM, Sears-Rogan P, Mathew JP, Quinones MA, Cahalan MK, Savino JS. ASE/SCA guidelines for performing a comprehensive intraoperative multiplane transesophageal echocardiography examination: recommendations of the American Society of Echocardiography Council for Intraoperative Echocardiography 48 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. Y. Wang and C. Gao and the Society of Cardiovascular Anesthesiologists Task Force for Certification in Perioperative Transesophageal Echocardiography. Anesth Analg. 1999;89(4):870–84. Lang RM, Badano LP, Tsang W, Adams DH, Agricola E, Buck T, Faletra FF, Franke A, Hung J, Perez de Isla L, Kamp O, Kasprzak JD, Lancellotti P, Marwick TH, McCulloch ML, Monaghan MJ, Nihoyannopoulos P, Pandian NG, Pellikka PA, Pepi M, Roberson DA, Shernan SK, Shirali GS, Sugeng L, TenCate FJ, Vannan MA, Ten Cate FJ, Vannan MA, Luis Zamorano J, Zoghbi WA. EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography. J Am Soc Echocardiogr. 2012;25(1):3–46. Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996;24(12):2053–8. Adams DH, Anyanwu AC, Sugeng L, Lang RM. Degenerative mitral valve regurgitation: surgical echocardiography. Curr Cardiol Rep. 2008;10(3):226–32. Grewal KS, Malkowski MJ, Piracha AR, Astbury JC, Kramer CM, Dianzumba S, Reichek N. Effect of general anesthesia on the severity of mitral regurgitation by transesophageal echocardiography. Am J Cardiol. 2000;85(2):199–203. Riegel AK, Busch R, Segal S, Fox JA, Eltzschig HK, Shernan SK. Evaluation of transmitral pressure gradients in the intraoperative echocardiographic diagnosis of mitral stenosis after mitral valve repair. PLoS One. 2011;6(11):e26559. Perier P, Hagen T, Stumpf J. Septal myectomy for left ventricular outflow tract obstruction after mitral valve repair. Ann Thorac Surg. 1994;57(5):1328–30. Lopez JA, Schnee M, Gaos CM, Wilansky S. Left ventricular outflow tract obstruction and hemolytic anemia after mitral valve repair with a Duran ring. Ann Thorac Surg. 1994;58(3): 876–7. Mascagni R, Al Attar N, Lamarra M, Calvi S, Tripodi A, Mebazaa A, Lessana A. Edge-to-edge technique to treat post-mitral valve repair systolic anterior motion and left ventricular outflow tract obstruction. Ann Thorac Surg. 2005;79(2):471–3. Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, Nishimura RA, Ommen SR, Rakowski H, Seidman CE, Towbin JA, Udelson JE, Yancy CW. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011;58(25):e212–60. Meloni L, Aru G, Abbruzzese PA, Cardu G, Ricchi A, Cattolica FS, Martelli V, Cherchi A. Regurgitant flow of mitral valve prostheses: an intraoperative transesophageal echocardiographic study. J Am Soc Echocardiogr. 1994;7(1):36–46. Karthik S, Sundar S, Lerner A, Panzica P, Subramaniam B, Mahmood F. Intraoperative assessment of perivalvular mitral regurgitation: utility of three-dimensional-echocardiography. J Cardiothorac Vasc Anesth. 2008;22(3):431–4. De Canniere D, Jansens JL, Unger P, Le Clerc JL. Left ventricular outflow tract obstruction after mitral valve replacement. Ann Thorac Surg. 1997;64(6):1805–6. 49. Come PC, Riley MF, Weintraub RM, Wei JY, Markis JE, Lorell BH, Grossman W. Dynamic left ventricular outflow tract obstruction when the anterior leaflet is retained at prosthetic mitral valve replacement. Ann Thorac Surg. 1987;43(5):561–3. 50. Guler N, Ozkara C, Akyol A. Left ventricular outflow tract obstruction after bioprosthetic mitral valve replacement with posterior mitral leaflet preservation. Tex Heart Inst J. 2006;33(3):399–401. 51. Baumgartner H, Bonhoeffer P, De Groot NMS, de Haan F, Deanfield JE, Galie N, Gatzoulis MA, Gohlke-Baerwolf C, Kaemmerer H, Kilner P, Meijboom F, Mulder BJM, Oechslin E, Oliver JM, Serraf A, Szatmari A, Thaulow E, Vouhe PR, Walma E, Esc. ESC guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J. 2010;31(23):2915–57. 52. Gao CQ, Yang M, Wang G, Wang J, Xiao C, Wu Y, Li J. Totally endoscopic robotic atrial septal defect repair on the beating heart. Heart Surg Forum. 2010;13(3):E155–8. 53. Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, del Nido P, Fasules JW, Graham Jr TP, Hijazi ZM, Hunt SA, King ME, Landzberg MJ, Miner PD, Radford MJ, Walsh EP, Webb GD, Writing Comm M. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease. J Am Coll Cardiol. 2008;52(23):e143–263. 54. Franke A, Kuhl HP, Rulands D, Jansen C, Erena C, Grabitz RG, Dabritz S, Messmer BJ, Flachskampf FA, Hanrath P. Quantitative analysis of the morphology of secundum-type atrial septal defects and their dynamic change using transesophageal three-dimensional echocardiography. Circulation. 1997;96(9):II-323–7. 55. Kronzon I, Tunick PA, Freedberg RS, Trehan N, Rosenzweig BP, Schwinger ME. Transesophageal echocardiography is superior to transthoracic echocardiography in the diagnosis of sinus venosus atrial septal defect. J Am Coll Cardiol. 1991;17(2):537–42. 56. Hausmann D, Daniel WG, Mugge A, Ziemer G, Pearlman AS. Value of transesophageal color Doppler echocardiography for detection of different types of atrial septal defect in adults. J Am Soc Echocardiogr. 1992;5(5):481–8. 57. Unver S, Karadeniz U, Yamak B, Catav Z, Erdemli O. Utility of intraoperative transesophageal echocardiography in an atrial septal defect operation. J Cardiothorac Vasc Anesth. 2006;20(1):90–3. 58. Dein JR, Frist WH, Stinson EB, Miller DC, Baldwin JC, Oyer PE, Jamieson S, Mitchell RS, Shumway NE. Primary cardiac neoplasms. Early and late results of surgical treatment in 42 patients. J Thorac Cardiovasc Surg. 1987;93(4):502–11. 59. Gao C, Yang M, Wang G, Wang J, Xiao C, Wu Y, Li J. Excision of atrial myxoma using robotic technology. J Thorac Cardiovasc Surg. 2010;139(5):1282–5. 60. Aru GM, Falchi S, Cardu G, Meloni L, Lixi G, Martelli V. The role of transesophageal echocardiography in the monitoring of cardiac mass removal: a review of 17 cases. J Card Surg. 1993;8(5):554–7. 61. Dujardin KS, Click RL, Oh JK. The role of intraoperative transesophageal echocardiography in patients undergoing cardiac mass removal. J Am Soc Echocardiogr. 2000;13(12):1080–3. 62. Pineda AM, Santana O, Zamora C, Benjo AM, Lamas GA, Lamelas J. Outcomes of a minimally invasive approach compared with median sternotomy for the excision of benign cardiac masses. Ann Thorac Surg. 2011;91(5):1440–4. 4 Peripheral Cardiopulmonary Bypass Establishment for Robotic Cardiac Surgery Cangsong Xiao and Changqing Gao Abstract Conventional cardiac surgery is performed via median sternotomy and central cardiopulmonary bypass (CPB) is performed through cannulation on ascending aorta and superior vena cava and inferior vena cava. Robotic surgical technology has provided port-access which has made peripheral CPB endoaortic balloon occluders possible. Establishment of peripheral CPB has been an important step for robotic cardiac surgery. The standard procedures of peripheral CPB establishment include right internal jugular cannulation and femoral artery and vein cannulation. This chapter describes the peripheral CPB technique which has been used routinely for totally robotic cardiac surgery using da Vinci Surgical System at the Chinese PLA General Hospital. Conventional cardiac surgery is performed via median sternotomy and central cardiopulmonary bypass (CPB) is performed through cannulation on ascending aorta and superior vena cava (IVC) and inferior vena cava (SVC). With the evolution of minimally invasive cardiac surgery, especially totally robotic cardiac surgery [1–3], very limited skin incisions make central CPB extremely difficult or even impossible and peripheral CPB becomes mandatory. Port-access technology for peripheral CPB with endoaortic balloon occluders was reported applicable and strongly advocated for minimally invasive and robotic mitral surgery by some authors [4–7]. However, this technique has such disadvantage as migration of the occluding balloon resulting in inadvertently occlusion of cephalic artery and subsequently compromising of cerebral blood flow. Therefore, peripheral CPB establishment through internal jugular vein and femoral artery and vein and direct aortic cross clamping via intercostal space by Chitwood clamp is more reasonable to avoid this disadvantage. Moreover, C. Xiao, MD • C. Gao, MD (*) Department of Cardiovascular Surgery, PLA General Hospital, No. 28 Fuxing Road, Beijing 100853, People’s Republic of China e-mail: gaochq301@yahoo.com Reichenspurner and colleagues demonstrated increased morbidity, cost, and operative/cross-clamp times when the endoballoon technique was used for mitral valve surgery [8]. The standard procedures of peripheral CPB establishment include right internal jugular cannulation and femoral artery and vein cannulation. Aorta is cross-clamped with Chitwood clamp through 4th intercostal space. Myocardial preservation is achieved by antegrade delivery of cardioplegia via angio-catheter inserted into ascending aorta, mostly through 2nd intercostal space. 4.1 Pre-operative Preparation for Establishment of Peripheral CPB Preoperative evaluations of candidates for robotic cardiac surgery include heart lesions suitable for robotic correction, general conditions of patients as well as peripheral arteries and veins. Regarding the peripheral CPB setup, much attention is paid to ECHO examination of right internal jugular vein and bilateral femoral arteries and veins. For young patients, ECHO is of adequacy for thorough investigation of peripheral vessels. For patients older than 60 years, 3-D CTA is necessary for further evaluation of iliac-femoral artery and abdominal aorta to exclude the patient with significant atherosclerotic stenosis or tortuosity of the arteries (Fig. 4.1). For patients C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_4, © Springer Science+Business Media Dordrecht 2014 49 50 C. Xiao and C. Gao Fig. 4.1 3-D CTA of iliac-femoral artery and abdominal aorta older than 50 years, coronary angiogram is routinely conducted. For patients younger than 50 years with risk factors of atherosclerosis, CTA is used to evaluate coronary artery (Fig. 4.2). The right femoral artery and vein are preferred for cannulation, therefore, right femoral artery is not used for angiography to avoid local hematoma which may complicate the cannulation. For cases of previous history of abdominal surgery, such as kidney surgery, magnetic resonance imaging (MRI) is probably necessary for watching out if IVC stenosis was created. 4.2 Preparation of Conduits of Peripheral CPB The CPB conduits are specially designed for the peripheral CPB establishment at the PLA General Hospital. Venous conduit has two bifurcations, one is much shorter than the other so that these two conduits can be comfortably placed on the table after cannulation (Fig. 4.3). Proper size of cannula for femoral artery and vein cannulation is selected according to the weight and height of the patient. The surgeon’s experience is also of much importance for cannula selection. So far, 15 F cannula is routinely used for internal jugular cannulation at the PLA General Hospital, and Fig. 4.2 3-D CTA of coronary artery Connected to IVC Connected to SVC Fig. 4.3 Venous conduits placed on table the outflow is sufficient. For femoral vein cannulation, 23 F cannula is most frequently used. 21 F cannula is adequate for arterial inflow for patients with weight of about 80 kg. The lightest weight of the patient receiving robotic heart surgery performed at the PLA General Hospital was 29 kg, and the arterial cannula size was 17 F. 4 Peripheral Cardiopulmonary Bypass Establishment for Robotic Cardiac Surgery a 51 b Fig. 4.4 Internal jugular cannula with guidance of ECHO. (a) To puncture the internal jugular vein under guidance of ECHO; (b) The EECHO view a b 15G Fig. 4.5 A 15G angio-catheter is pre-positioned 10 mm above clavicle (a) and heparin is infused (b) 4.3 Techniques for Peripheral CPB Establishment Intraoperative transesophageal echocardiography (TEE) plays a very important role in venous cannulation for peripheral CPB set up. The precise positioning of the internal jugular vein cannula and femoral vein cannula, which are both advanced into right atrium, must be guided by TEE. After general anesthesia and double-lumen endotracheal intubation, a 15 gauge angio-catheter is inserted and secured in advance by anesthesiologist with the guidance of ECHO (Fig. 4.4) and heparin is infused inside the catheter (Fig. 4.5). The puncture site of skin for angio-catheter is just 10 mm above the clavicle. The puncture site of internal jugular vein should be guided by ECHO and be just at the anterior middle portion of the vein, which is important for subsequent smooth advancement of a 15 F cannula. Another 7 F double lumen catheter is also introduced more cephalically (Fig. 4.6). 4.4 Exposure of Femoral Artery and Vein The patient is positioned as described above, and followed by sterilization and draping. A 2-cm transverse right groin incision just above the crease is made to expose the femoral artery and vein. The two vessels are dissected just below, rather than above, the femoral canal. This maneuver can avoid injury of structures within femoral canal, and may not decrease the strength of the abdominal wall because the plane of dissection is just at the inferior edge, instead of within, the femoral canal (Fig. 4.7). A purse string with 5/0 52 C. Xiao and C. Gao a b Fig. 4.6 Another 7 F double lumen catheter is inserted cephalically a b c Femoral V Femoral A Fig. 4.7 Exposure of femoral artery and vein. (a) The skin mark of incision; (b) The dissection plane at the inferior edge of abdominal wall; (c) The dissected right femoral artery and vein 4 Peripheral Cardiopulmonary Bypass Establishment for Robotic Cardiac Surgery a 53 b c Fig. 4.8 (a) A purse string suture on the right femoral vein; (b and c) Two snares around right femoral artery and vein polypropylene suture is placed at the anterior wall of the femoral vein. Two snares are placed around the femoral artery and vein respectively (Fig. 4.8). 4.5 Femoral Artery Cannulation After systemic heparinization (300 IU/kg), the femoral arterial is clamped with two fine clamps, between which transverse arteriotomy was made and the arterial cannula is inserted using the Seldinger guidewire method. The guidewire, which has been inserted within the cannula in advance, is firstly introduced into femoral artery. The guidewire should be passed into the artery smoothly without any resistance. Arterial cannula insertion along the guidewire is followed. Assistant should hold the end of the cannula tightly to facilitate the insertion of the tip of the cannula. The surgeon holds the tape and the cannula is carefully advanced into the artery for at least 10 cm deep along the guidewire. Femoral artery is then snared and the guidewire is withdrawn and the cannula is clamped by the assistant. Blood is allowed to squirt for deairing and good blood flow is checked. Cannula is connected to the arterial conduit of CPB and secured with two sutures (Fig. 4.9). 4.6 Femoral Vein Cannulation into the Right Atrium Just after completion of arterial cannulation, TEE probe has already been standing by and focusing on the IVC to guide the venous cannula positioning. The two snares around 54 C. Xiao and C. Gao a b c d e f g h Fig. 4.9 (a–h) Femoral artery cannulation using Seldinger guidewire method. (a) The clamp for femoral artery occlusion; (b) The right femoral artery was occluded; (c) The end of femoral catheter; (d) The assistant hold the end of the cannula to facilitate the insertion of the tip of the cannula; (e) The cannula is advanced into the femoral artery; (f) Deairing and check the blood flow; (g) The cannula was connected to the arterial conduit of CPB; (h) The cannula was secured with two sutures 4 Peripheral Cardiopulmonary Bypass Establishment for Robotic Cardiac Surgery a b c d e f 55 Fig. 4.10 Femoral vein cannulation using Seldinger guidewire method. (a) A small incision was made on femoral vein; (b) The incision was dilated; (c) The guidewire was inserted into the femoral vein; (d) The cannula was inserted into femoral vein along the guidewire; (e) The cannula was connected to the vein conduit of CPB; (f) The tip of femoral vein cannula femoral vein are pulled slightly and a small incision is created within the purse string suture. The small incision is dilated by mosquito clamp to facilitate venous cannula entrance. Seldinger guidewire is then advanced into right atrium under the guidance of TEE followed by venous cannula insertion. The venous cannula tip is positioned at the middle portion of right atrium. Care must be taken to clearly visualize the cannula passing through the SVC and into right atrium. The cannula is clamped and subsequently connected to venous conduit of CPB. Before the clamp is released, the other end of bifurcated venous conduit of CPB must be clamped to prevent bleeding (Fig. 4.10). 4.7 Right Internal Jugular Cannulation into Right Atrium After femoral vein is cannulated, right internal jugular vein cannulation is followed. Seldinger guidewire is firstly advanced into right atrium through the pre-positioned angio-catheter. The 56 C. Xiao and C. Gao a b c d e f Fig. 4.11 (a–f) Right internal jugular vein cannulation into right atrium using Seldinger guidewire method. (a) The 15G angio-catheter was prepositioned; (b) The guidewire was inserted into the catheter; (c) The dilating sheaths with different diameter are respectively passed through the guidewire; (d) The cannula was inserted into jugular vein along the guidewire; (e) The cannula was secured; (f) The secured vein cannula angio-catheter is withdrawn and the guidewire is left in place. The assistant presses the jugular vein with left hand to prevent bleeding and hold the guidewire with thumb and pointing finger of left hand to prevent inadvertently pulling out the guidewire. The skin is incised with blade and dilated with tip of mosquito clamp. Two dilating sheaths with different diameter are respectively passed through the guidewire and into SVC to make a channel along the guidewire to facilitate the passage of a 15 F cannula. After the second dilating sheath is withdrawn and guidewire is still in place, the cannula was passed along the guidewire and into right atrium guided by TEE. The assistant should hold the end of the cannula to help the surgeon easily pass the tip of the cannula across the entering site of the vein and into right atrium. The cannula is connected to another venous conduit and secured (Fig. 4.11). At this moment, the peripheral CPB establishment for robotic cardiac surgery is completed. 4 Peripheral Cardiopulmonary Bypass Establishment for Robotic Cardiac Surgery a 57 b Fig. 4.12 (a) Chitwood clamp is introduced through the 4th intercostal space adjacent to the inferior edge of working port; (b) The inferior jaw of clamp must not bite the pulmonary trunk and right pulmonary artery 4.8 Techniques for Antegrade Cardioplegia Delivery a 12G Chitwood clamp is used through the 4th intercostal space adjacent to the inferior part of working port. The bed side surgeon must hold the shaft of Chitwood clamp tightly with both hands and slowly let the clamp go forward. After perfusion flow is decreased and blood pressure is lowed by perfusionist, jaws of Chitwood clamp is opened very carefully under guidance of console surgeon. The inferior jaw must not bite the pulmonary trunk and right pulmonary artery in case of injury (Fig. 4.12). 14G angio-catheter is routinely used for cardioplegia delivery at the PLA General Hospital. A side hole on the catheter, 4 mm away from the tip, is created by a scrubbing nurse (Fig. 4.13). The catheter is often obliquely advanced through the 2nd intercostal space, about 3 cm lateral to the stay suture catheter. Then cardioplegia is delivered to irrigate the catheter to flush away the residuals inside the needle to prevent embolism (Fig. 4.14). Console surgeon slightly hold the catheter and puncture the ascending aorta and the bedside surgeon must meticulously cooperate. After the tip of the catheter has crossed aortic wall for about 1 cm, the inside needle is withdrawn by the bedside surgeon. At the essential moment as the catheter proceeds the tip of catheter must by carefully visualized by TEE. Proper location of the tip is always near the posterior wall of aorta (Fig. 4.15). The catheter is fixed by sutures on the chest wall. Attention should be taken so as to avoid the risks of injuring the aortic wall or valve because the catheter tip is too close to the aortic wall. Inadvertent forward displacement of the catheter during surgery is also risky. Cross clamping of aorta should always be cautious like in open chest cardiac surgery. Prior to clamping, perfusing flow is decreased and the aorta is slowly clamped. Cardioplegia delivery is constantly monitored by TEE (Fig. 4.16). Again, the tip of catheter must be confirmed inside the aorta. 14G 15G b c Fig. 4.13 (a) 14G angio-catheter is used for cardioplegia delivery; (b) A side hole on the catheter; (c) 4 mm away from the tip, is showed 58 C. Xiao and C. Gao a b Fig. 4.14 (a) The catheter is advanced through the 2nd intercostal space, 3 cm lateral to the staying suture catheter; (b) Cardioplegia is delivered to irrigate the catheter to flush away the debris inside the needle a b Fig. 4.15 (a) Catheter goes through anterior wall of ascending aorta; (b) Proper location of its tip, always near the posterior wall of aorta, is monitored by TEE Sometimes aortic regurgitation may be detected by TEE and the depth of catheter should be adjusted and regurgitation can be corrected. After all the procedures are completed and heart incision is closed, clamp is slowly released and the heart beat resumed. The catheter delivering cardioplegia is used for deairing. Surgical outcome is checked by TEE. A purse string by a mattressed Gortex suture is placed around the aortic puncture site. At the same time of decreasing perfusing flow, the catheter is pulled out of aorta and the purse suture is tied (Fig. 4.17). Cardiopulmonary bypass is weaned off as usual. 4.9 De-cannulation After Conclusion of CPB After conclusion of CPB, surgical results are evaluated by TEE. Protamine is administered and the ACT is titrated to baseline value and de-cannulation is followed. Femoral venous cannula is always withdrawn firstly. The purse string suture is held slightly when the cannula is pulled out to prevent bleeding and then tied. Care must be taken in decannulation. The conduit connected to the right internal jugular vein cannula should be clamped in case of bleeding before withdrawing the femoral venous cannula. Femoral 4 Peripheral Cardiopulmonary Bypass Establishment for Robotic Cardiac Surgery a 59 b Fig. 4.16 (a) Aorta is cautiously clamped; (b) Cardioplegia delivery is constantly monitored by TEE and aortic valve competency is verified a b c Fig. 4.17 Before CPB is weaned off, catheter delivering cardioplegia is withdrawn and a mattressed Gortex suture is used for hemostasis. (a) The pure string suture is placed around the catheter; (b) The suture is tied using pusher by the assistant; (c) The tied kont 60 C. Xiao and C. Gao arterial cannula must be removed always with great caution. The distal snare is released and the artery is clamped with a fine clamp. The proximal snare is released but the snare tape is kept in place and another clamp is placed in advance. After these preparation, the proximal snare tape is held slightly and the cannula is slowly pulled out and the artery is immediately clamped. The proper site of the two clamps may be adjusted for more space to facilitate subsequent repair of the artery. The width of arterial wall of both side of arteriotomy should be adequate for suturing. The proximal edge of the arteriotomy is always much larger than the distal one because of cannulation and the posterior wall may be injured, which will make the approximation of both edge technically demanding. A 6/0 polypropylene running suture is placed evenly to approximate the two edges of arteriotomy. The suture should not be frapped too tight to avoid artery stenosis. Right internal jugular vein cannula is pulled out and puncture site of vein is compressed for at least ten minutes for hemostasis and skin incision is sutured. 4.10 Results So far, 640 cases of totally robotic has been successfully performed at the PLA General Hospital [9–11], which include 297 cases of peripheral cardiopulmonary bypass. Only one adult patient with Marfan syndrome was converted to sternotomy because of failure of venous cannulation due to lower part of IVC or bilateral common iliac vein stenosis. Postoperative thrombotic complication at the site of peripheral cannulation occurred in five patients at an earlier time after the operation. Three patients suffered from femoral vein thrombus formation which was resolved by warfarin. Two patients had femoral artery thrombus which was resolved by re-exploration for thrombus clearance. We think that the cause for thrombus was the compression of the cannulation site for prevention of bleeding in previous cases. We realized afterwards that this compression of cannulation site was unnecessary and abandoned such practice. With this learning curve, we started giving 100 mg aspirin routinely to patients for 3 months after the operation to prevent thrombotic complications. In all cases, antegrade delivery of cardioplegia via 14G agiocatheter provides optimal myocardial protection. With the aortic cross clamping technique well applied, no pulmonary artery may be injured. References 1. Modi P, Rodriguez E, Chitwood WR. Robot assisted cardiac surgery. Interact Cardiovasc Thorac Surg. 2009;9(3):500–5. 2. Kypson AP, Chitwood WR. The use of robotics in cardiovascular surgery. Future Cardiol. 2005;1(4):61–7. 3. Chitwood WR. Current status of endoscopic and robotic mitral valve surgery. Ann Thorac Surg. 2005;79:S2248–53. 4. Vanermen H, Farhat F, Wellens F, et al. Minimally invasive video assisted mitral valve surgery: from Port-Access towards a totally endoscopic procedure. J Card Surg. 2000;15:51. 5. Vanermen H, Wellens F, De Geest R, et al. Video-assisted PortAccess mitral valve surgery: from debut to routine surgery. Will Trocar-Port-Access cardiac surgery ultimately lead to robotic cardiac surgery? Semin Thorac Cardiovasc Surg. 1999;11:223. 6. Murphy D, Miller JS, Langford DA, Snyder AB. Endoscopic robotic mitral valve surgery. J Thorac Cardiovasc Surg. 2006;132: 776. 7. Colvin SB, Galloway AC, Ribakove G, et al. Port-Access mitral valve surgery: summary of results. J Card Surg. 1998;13:286. 8. Reichenspurner H, Detter C, Deuse T, et al. Video and roboticassisted minimally invasive mitral valve surgery: a comparison of the Port-Access and transthoracic clamp techniques. Ann Thorac Surg. 2005;79:485; discussion 490. 9. Gao C, Yang M, Wang G, et al. Totally robotic resection of myxoma and atrial septal defect repair. Interact Cardiovasc Thorac Surg. 2008;7(6):947–50. 10. Gao C, Yang M, Wang G, Wang J, Xiao C, Wu Y, Li J. Totally endoscopic robotic atrial septal defect repair on the beating heart. Heart Surg Forum. 2010;13(3):E155–8. 11. Gao C, Yang M, Wang G, et al. Totally endoscopic robotic ventricular septal defect repair. Innovations (Phila). 2010;5(4):278–80. 5 Robotic Surgery in Congenital Heart Diseases Changqing Gao and Ming Yang Abstract Surgical techniques to reduce postoperative recovery time and improve the cosmetic results have been achieved through limited incisions. In the late 1990s, as a result of technical innovation in peripheral cardiopulmonary bypass (CPB) technology combined with the possibility of endoaortic clamping, remote cardiac arrest became feasible and thus enabled small access and thoracoscopic surgery. Conventional thoracoscopic instruments have limited degrees of freedom, which hampers performance of complex maneuvers that involve tissue reconstruction, such as suturing and tying knots, particularly under tension. Robotic surgical instruments have the dexterity required for these complex maneuvers and, therefore, hold the promise of facilitating truly thoracoscopic repair of cardiac defects even in children. Application of robotic approaches for open heart procedures now still is confined to operations where much of the intracardiac repair is performed through the right atrium, such as closure of atrial or ventricular septal defects, atrioventricular canal defects, atrioventricular valve repair/replacement. This chapter describes the robotic surgical system employed in the congenital heart disease in adult. 5.1 Robotic Atrial Septal Defects Repair in Adults For atrial septal defect (ASD) in adults, surgical repair has been performed for more than 50 years. Lewis and Taufic performed the first successful ASD closure in 1953 [1]. Since then standard surgical closure of an ASD via sternotomy or thoracotomy has been a safe and effective procedure with low morbidity and mortality [2, 3]. Currently, there is a growing interest in minimally invasive approaches in all fields of cardiac surgery. The ASD closure traditionally conducted via median sternotomy has been recently forwarded by progressively advanced minimally invasive technology. In parallel, closure of small ostium secundum and patent foramen ovale types of ASD by different percutaneous catheter techniques have been developed by interventional C. Gao, MD (*) • M. Yang, MD Department of Cardiovascular Surgery, PLA General Hospital, No. 28 Fuxing Road, Beijing 100853, People’s Republic of China e-mail: gaochq301@yahoo.com cardiologists [4, 5]. The catheter procedure avoids operative trauma and reduces hospital stay, although it is associated with occasional major complications [6]. The success rate in the transcatheter approach depends on the size and shape of the defect. Therefore, surgery will undoubtedly continue to be an option for the treatment. With the development of portaccess technology for peripheral cardiopulmonary bypass (CPB) induction and the use of a transthoracic clamp, skin incision could be further reduced [7–9]. The recent clinical introduction of robotically assisted surgery finally enables totally endoscopic procedures through ports. Robotic systems comprised of miniaturized surgical instruments with multiple degrees of motion, coupled with a dual camera endoscope providing true three-dimensional high-magnification visualization that had greatly propelled this field. With the assistant of robotic surgical system, the surgeon can perform complex intracardiac procedures such as ASD closure, coronary artery bypass and mitral valve repair or replacement through smaller incisions. Since Torracca and colleagues [10] reported a small series of patients undergoing robotic ASD repair in 2001, other C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_5, © Springer Science+Business Media Dordrecht 2014 61 62 C. Gao and M. Yang Fig. 5.2 Intraoperative TEE check Fig. 5.1 Checking the intubation depth using bronchofiberscope authors [11–13] subsequently report their experiences. The first case of ASD repair in China was performed robotically on January 15, 2007 at the PLA General Hospital [14]. The group of robotic ASD repairs enrolled the most cases that supplement this experience at beginning. 5.1.1 Anesthesia, Patient Position and CPB Establishment Anesthesia is induced using a standard technique with a leftsided double-lumen endotracheal intubation for single-lung ventilation. And the flexible bronchofiberscope is used to identify the proper intubation depth (Fig. 5.1). The transesophageal echocardiography (TEE) probe is inserted (Fig. 5.2) to evaluate the position of the venous cannulas. Both a central venous catheter and a 15-F or 17-F venous drainage cannula are placed percutaneously into the right internal jugular vein (Figs. 5.3 and 5.4). External defibrillator patches are placed to subtend the maximum cardiac mass. Each patient is positioned with the right side of the chest elevated approximately 30° and with the right arm tucked at the side (Fig. 5.5). After systemic heparinization (300 IU/ kg), the femoral arterial (18–20 F) and venous cannulations (21–23 F) are performed through a 2-cm transverse right groin incision (Fig. 5.6) by using the Seldinger guide wire Fig. 5.3 Puncture the internal jugular vein under TEE guidance Fig. 5.4 Central venous catheter and internal venous drainage cannula 5 Robotic Surgery in Congenital Heart Diseases 63 Fig. 5.5 The patient position Fig. 5.7 Right internal jugular vein cannulation Fig. 5.6 Femoral arterial and venous cannulations method and TEE guidance. Bicaval venous drainage is instituted through the jugular and femoral/inferior vena cava cannulas (Fig. 5.7) [14]. 5.1.2 Surgical Technique on Arrested Heart [14] 5.1.2.1 Robotic ASD Closure on Arrested Heart After exclusion of the right lung, a 12-mm endoscopic trocar is placed into the right thoracic cavity through the fourth intercostal space (ICS), lateral to the nipple. The pleural space is insufflated with carbon dioxide at a maximum pressure of 8–10 mmHg, usually 6 mmHg, and the 30° endoscopic camera is inserted. A 1.5–2.0 cm incision is used as a working port in the same ICS for the patient-side surgeon. Additionally two 8-mm port incisions are made in the second and sixth ICS to allow insertion of the left and right instrument arms. The right instrument arm generally is positioned 4–6 cm lateral to the working port in the sixth ICS. The left instrument arm is positioned medial and cephalad to the right arm in the second or third ICS. The fourth arm trocar is placed in the midclavicular line in the 4th or 5th ICS [14], dependent on the patient’s rib direction and ICS. Two 16 F Angiocatheters are inserted in the 6th and 4th ICS laterally respectively for the placement of pericardial stay sutures (Figs. 5.8 and 5.9). CPB is initiated with kinetically assisted bicaval venous. The intrathoracic part of the operation began robotically with pericardiotomy and placement of pericardial stay sutures. The pericardium is opened longitudinally 1.5 cm anteriorly to the phrenic nerve (Fig. 5.10). The incision is extended superiorly to expose the superior vena cava and then extended inferiorly to the diaphragm to visualize the inferior vena cava. The pericardium stay sutures are placed 64 C. Gao and M. Yang Fig. 5.8 Ports position Fig. 5.11 The pericardium stay suture Fig. 5.9 Setup of the da Vinci Surgical System Fig. 5.12 The stay suture on the left superior side of pericardium to expose the aorta Fig. 5.10 The pericardium was opened anteriorly to the phrenic nerve on the right side of pericardium to rotate the heart for optimal exposure of the atrium (Fig. 5.11). And the 3rd pericardium stay suture is placed on the left superior side of pericardium through anterior chest (16 Ga Angio) to expose the aorta (Fig. 5.12). The space between the vena cavae and the pulmonary veins are dissected clear (Figs. 5.13 and 5.14). And the linear tapes are placed around the inferior and superior vena cavae (Figs. 5.15 and 5.16). The aortic occlusion is performed with a Chitwood cross-clamp via the midaxillary line in the fourth ICS (Figs. 5.17 and 5.18). Antegrade cold blood cardioplegic solution is administered directly through the anterior chest (the second ICS) with a 14 Ga Angiocatheter (Figs. 5.19 and 5.20). 5 Robotic Surgery in Congenital Heart Diseases 65 Fig. 5.16 The tape around the superior vena cavae Fig. 5.13 Dissected the space between superior vena cava and right superior pulmonary vein Fig. 5.14 Dissected the space between inferior vena cava and right inferior pulmonary vein Fig. 5.17 The extracorporeal position of Chitwood clamp Fig. 5.18 The Chitwood cross-clamp Fig. 5.15 The tape around the inferior vena cavae 66 Fig. 5.19 14 Ga angiocatheter is inserted into the aorta C. Gao and M. Yang Fig. 5.21 The right atrium is opened Fig. 5.22 The atrial retractor is introduced into right atrium Fig. 5.20 Administration cold blood cardioplegic solution through the angiocatheter After snaring of the superior and inferior vena cavae, the right atrium is opened (Fig. 5.21). The atrial retractor is introduced into the right atrium through the fourth robotic arm to expose the atrial septal defect (Fig. 5.22). Cardiotomy suction is passed through the working port by the patientside surgeon. After thorough exploration, ASD is closed directly using 4-0 Gore-Tex running suture or autologous pericardial patching, depending on the size and location of ASD (Figs. 5.23 and 5.24). The knot tying is performed extracorporeally by patient-side surgeon using a knot pusher. And the atrial leakage is identified before closing right atrium. If the moderate to severe tricuspid valve regurgitation is diagnosed, the retractor is removed to expose the tricuspid valve and ring. The tricuspid valve plasty is performed using De Vaga technique. The result of tricuspid valve plasty Fig. 5.23 Closing the ASD using running suture 5 Robotic Surgery in Congenital Heart Diseases 67 Fig. 5.24 Closing the ASD using autologous pericardial patch Fig. 5.26 Evaluating the plasty result Fig. 5.25 Tricuspid valve plasty using De Vaga technique is evaluated (Figs. 5.25 and 5.26). The right atrium is closed with double-layer 4-0 Gore-Tex running suture (Fig. 5.27). The deairing is done through the cardioplegia Angiocatheter. Then the aortic puncture site is closed using 4-0 Gore-Tex (Fig. 5.28). After adequate hemostasis achieved, the robotic arms are removed and a chest tube is inserted through right arm porthole. The right femoral artery is reconstructed after removing of the cannulas. 5.1.2.2 Robotic ASD Repair on Beating Heart For ASD closure on beating heart, the aortic occlusion and cardioplegic solution administration can be avoided [15]. Under mild hypothermic conditions (rectal temperature, 34–35 °C), CPB full flow is maintained with mean systemic pressure more than 60 mmHg. To avoid air embolism, carbon dioxide with 6–8 mmHg is insufflated continuously into the chest for air displacement. On beating heart, a right atriotomy is performed under SVC and IVC snared with same techniques mentioned above, and ASD is exposed with atrial retractor by the 4th arm. A small suction catheter is placed in the right atrium, not in the left atrium through the Fig. 5.27 The right atrium is closed with double-layer running suture Fig. 5.28 Aortic puncture site is closed 68 Fig. 5.29 The right atrium is opened on beating heart under SVC and IVC snared Fig. 5.30 The atrial retractor is introduced into the right atrium Fig. 5.31 ASD is exposed with the aid of atrial retractor working port. The direct closure with running suture or autologous pericardium patching can be used (Figs. 5.29, 5.30, 5.31, 5.32, and 5.33). As the inter-atrial septum is closed, the lung is briefly inflated, and the inter-atrial suture line is secured when there is no evidence of retained air in the left atrium. C. Gao and M. Yang Fig. 5.32 The autologous pericardium patch is used for ASD closure Fig. 5.33 Secured suture line when there is no evidence of retained air in the left atrium Advantages of this method include avoidance of ischemiareperfusion injury, performance of surgery in a more physiological state of the heart, decreased use of inotropic medications, and shorter hospital stay [16]. In addition, proximal aortic arteriosclerosis is the source of macro- and microemboli at the time of placement and release of the aortic cross-clamp. Potential concerns related to this technique may include performance of surgery in a relatively bloodfilled field, limited surgical precision due to difficult exposure, risk of air embolization, and limited ability to perform very large ASD closure procedure on beating heart [16]. In fact, the operations can be performed without difficulty because the atrial retractor through 4th arm and small suction catheter from the working port could provide adequate visualization of the operative field. In addition, the concomitant surgery of tricuspid valve repair is easily performed. In our study, the complications related to beating heart ASD repair are not observed, such as, strokes or residual atrial septal defect due to dehiscence of the atrial suture line. For the prevention of air embolism, each patient is positioned with the right chest elevated approximately 30°. Furthermore, the left atrium is kept full without suction in it 5 69 Robotic Surgery in Congenital Heart Diseases during operation, and throughout the procedure carbon dioxide with 6–8 mmHg is insufflated continuously into the chest for air displacement. De-airing of left atrium at the end of the procedure is easily done. Based on this knowledge, it seems reasonable to perform robotic beating-heart ASD closure surgery with on-pump beating heart conditions. This technique is simple and it shortens the duration of CPB and total operation. Besides, this technique does not increase the risk of central nervous system (CNS) injury. It is not possible to determine with certainty whether minor neuron-cognitive disorders due to microembolization occur. The neurocognitive evaluation is an important aspect that needs to be further investigated. Possible contraindications to robotic beating-heart ASD repair may include the presence of mobile vegetations in patients with infective endocaditis or large left atrial thrombi, due to the risk of embolization. Inadequate experience of console surgeon certainly is contraindication to beating heart surgery. 5.1.3 Postoperative Management Postoperation patients are monitored at the intensive care unit (ICU) and discharged to an intermediate care unit as soon as hemodynamics and spontaneous respiration has become adequately stabilized. Chest drains are removed when drainage reaches less than 50 ml/12 h. All patients undergo transthoracic echocardiography immediately before discharge from hospital and at 3 months after the procedure. 5.1.4 Surgical Results and Learning Curves Totally endoscopic ASD closure remains a highly complex procedure, the performance of which requires experience with several non-routine operative steps, such as remote access perfusion and robotic cardiac surgery [17]. Moreover anesthesia management of those patients has additional non-routine steps as prerequisites, such as single-lung ventilation and advanced TEE for patient monitoring during remote access cardiopulmonary bypass (CPB) [13]. According to the previous literatures published, the robotic ASD closure is a more time-consuming operation compared with procedures in sternotomy, which requires long CPB and aortic occlusion time [10–13]. However, from our experience, we feel that robotic surgery is not time-consuming operation after overcoming the learning curve. The learning curves and operation times play a major role for the acceptance of such a program [13]. Between January 2007 and January 2013, 147 consecutive patients (99 female and 48 male) underwent ASD closure with da Vinci S or Si Surgical System at the PLA General Hospital. The mean age of the patients was 35.8 Table 5.1 The baseline characteristics of robotic ASD closure at the PLA General Hospital (01/2007 –01/2013) Variables Total number of patients Gender Male (%) Female (%) Age (year) Weight (kg) Height (cm) Pathology Atrial septal defect II, n (%) Patent foramen ovale, n (%) Median to sever tricuspid valve regurgitation, n (%) Median to sever pulmonary hypertension, n (%) Atrial septal aneurysm, n (%) Diameter of defect (cm) Left ventricular ejection fraction (%) Arrest Beating Both heart group heart group groups 54 93 147 16(29.6) 38(70.3) 35.2 ± 13.1 58.3 ± 10.0 162.6 ± 8.0 32(34.4) 61(65.6) 36.4 ± 13.3 61.7 ± 12.1 163.0 ± 8.2 48(32.7) 99(67.3) 35.8 ± 12.3 59.2 ± 13.6 162.7 ± 9.2 52(96.3) 2(3.7) 4(7.4) 91(97.8) 2(2.2) 8(8.6) 143(97.3) 4(2.7) 12(8.1) 6(11.1) 9(9.7) 15(10.2) 4(7.4) 2.8 ± 1.6 64.3 ± 7.1 2(2.2) 2.7 ± 1.8 65.8 ± 8.4 6(4.1) 2.7 ± 2.0 65.3 ± 6.4 Table 5.2 Results of robotic ASD closure at the PLA General Hospital (01/2007–01/2013) Variables Procedure, n Direct closure, n (%) Patch closure, n (%) Combined with tricuspid valve plasty, n (%) Operation time (min) Cardiopulmonary bypass time (min) Cross clamp time (min) Mechanical ventilation time (h) ICU duration (h) Drainage volume (ml) Length of stay (d) Arrest heart group 54 38(70.4) 16(29.6) 4(7.4) Beating heart group 93 34(36.6) 59(63.4) 8(8.6) 287.4 ± 58.7 103.5 ± 27.5 43.0 ± 10.2 4.9 ± 2.4 29.4 ± 7.8 107.8 ± 32.4 12.1 ± 4.5 207.9 ± 62.3* 61.9 ± 17.0* 0 4.7 ± 1.5 27.9 ± 3.8 92.4 ± 36.7 11.2 ± 3.2 *p < 0.05 years old (12–65 years), and ostium secundum ASD was confirmed echocardiographically on all patients. Patients were excluded if they could not tolerate single-lung ventilation or peripheral CPB, or otherwise were considered poor candidates for a thoracoscopic approach. Fifty-four cases were completed on arrest heart (arrest heart group) from January 2007 to December 2008, and 93 cases on beating heart (beating heart group) from December 2008 to January 2013 (Table.5.1). Anesthesia and surgical techniques were described above. The direct closure of ASD was performed in 72 cases, and autologous pericardial patching in 75 cases, and 8 patients accepted ASD repair combined with tricuspid valve repair (Table 5.2). TEE confirmed complete closure and tricuspid C. Gao and M. Yang 70 500.0 125.0 400.0 CPB time (min) Operation time (min) 150.0 300.0 100.0 75.0 50.0 200.0 0.0 10.0 20.0 30.0 40.0 50.0 0.0 60.0 10.0 20.0 Case number valve plasty in all cases. Reoperations and intraoperative conversions to alternate procedures were not needed. Mortality and serious complications were not encountered. In the arrest heart group, the median operating room time was 301.6 min (260–390 min), the median CPB time was 99.2 min (62–154 min), and the median cross-clamp time was 43.0 min (21–62 min). Every five patients were a group, then the mean operating room time, CPB time and crossclamp time were calculated and the coefficient of variation of each group was estimated. The operation, CPB and crossclamp time were stable if the two consecutive groups’ differences of coefficient of variation were smaller than 0.05. Learning curves were assessed by means of regression analysis with logarithmic curve fit. The operation time was stable after 30 cases and decreased with the increase of the case number (Fig. 5.34). The tendency of CPB time had the same pattern as the operating room time (Fig. 5.35). Significant learning curves were noted for cross-clamp time of arrest heart group: y(min) = 69.63 − 8.70 ln(x) ⟮r2 = 0.525; P < 0.01) (Fig. 5.36). In beating heart group, the median operating room time was 254.7 min (range, 120–330 min), and the median CPB time was 61.9 min (range, 40–94 min). The operating room time of beating heart group was stable after five cases, and the significant learning curve was noted: y (min) = 355.51 − 56.29 ln(x) ⟮r2 = 0.581; P < 0.01) (Fig. 5.37). The CPB time decreased as case number increased (Fig. 5.38). No statistic differences in median ventilation time, ICU stay, drainage volume, and length hospital of stay were shown between two groups. No perioperative neurologic event was recorded and no residual ASD was detected on intraoperative TEE and on postoperative TEE performed before discharge. All the patients were discharged, and 40.0 50.0 60.0 Fig. 5.35 The linear correlations of CPB time with case number (r2 = 0.349, p = 0.000) 70.0 60.0 Cross–clamp time (min) Fig. 5.34 The linear correlations of operation time with case number (r2 = 0.104, p = 0.017) 30.0 Case number 50.0 40.0 30.0 20.0 0.0 10.0 20.0 30.0 40.0 50.0 60.0 Case number Fig. 5.36 The learning curve of cross-clamp time in arrest heart group (y(min) = 69.63 − 8.70 ln(x); r2 = 0.525, p = 0.000) cosmetic results are excellent (Figs. 5.39, 5.40, 5.41, 5.42, 5.43, and 5.44). In our study, there were no incision conversions either to a thoracotomy or to a median sternotomy. These patients benefit from minimal musculoskeletal trauma, zero transfusion, and early discharge. We believe that ASD closure using da Vinci Surgical System, is feasible, safe and simple with excellent surgical results either on arrest heart or beating heart. 5.1.5 Summary During the past decade, improvements in instruments, endoscopes, as well as patients demand have resulted in a 5 71 Robotic Surgery in Congenital Heart Diseases Operation time (min) 400.0 300.0 200.0 100.0 0 20 40 60 Case number 80 100 Fig. 5.37 The learning curve of operating room time in beating heart group (y (min) = 355.51 − 56.29 ln(x); r2 = 0.581, p = 0.000) Fig. 5.39 Postoperative view of conventional sternotomy 100.0 90.0 CPB time (min) 80.0 70.0 60.0 50.0 40.0 30.0 0 20 40 60 Case number 80 100 Fig. 5.38 The linear correlations of CPB time with case number (r2 = 0.246, p = 0.000) substantial increase in minimally invasive cardiac surgical procedures being performed [17]. Endoscopic instrumentation, with only four degrees of freedom, significantly reduces the dexterity needed for delicate cardiac surgical procedures, and the loss of depth perception by using two-dimensional video monitor further increases operative difficulty [17]. With the advances in closed-chest cardiopulmonary bypass, micro instruments and computer telemanipulation, the robotic surgical system have been developed to facilitate the surgeons’ hand motion in limited closed chest operating spaces [18]. Computerized surgical robotic systems have been developed very rapidly in the past few years. The most common robotic applications in cardiac surgery are for mitral valve repair and endoscopic coronary artery bypass Fig. 5.40 One week after robotic ASD closure grafting. Argenziano et al. demonstrated that ASD in adults could be closed safely and effectively using totally endoscopic robotic approaches with a median cross-clamp time of 32 min [12]. Gao et al. reported first ASD repair surgery using da Vinci S Surgical System for in China in January, 2007, and subsequently, 54 ASD cases were completed on arrested heart. Since 2008, Gao and his team developed the techniques of beating-heart ASD repair without crossclamping the aorta and had excellent results [15]. Although transcatheter closure of ASD using an occluder has recently been presented as an alternative, it is considered difficult in practice for implantation for defects greater than 72 C. Gao and M. Yang Fig. 5.41 One month after robotic ASD closure in a female patient Fig. 5.43 Three months after robotic ASD closure Fig. 5.42 One month after robotic ASD closure in a male patient 30-mm in diameter or defects without sufficient amount of septal tissue. In addition, the long-term outcomes of occluder implantation remain to be clarified [19, 20]. Unlike transcatheter treatment, robotic surgery allows for closure of ASD of all types, including primum type or sinus venous defects, Fig. 5.44 Six months after robotic ASD closure 5 Robotic Surgery in Congenital Heart Diseases 73 as well as closure of multiple defects. Some ASD cases may be complicated by tricuspid regurgitation, however, robotic surgery provides a solution to these problems. Few reports have so far investigated the feasibility of robotic surgery for treating pediatric ASD, particularly in infants [21] because the femoral cannulation is the big issue. In conclusion, the robotic ASD closure can be safely implemented on arrest or beating heart, and is especially suitable for patients whose defects are greater than 30-mm in diameter, defects without sufficient amount of septal tissue for occluder implantation, or defects complicated by tricuspid regurgitation. 5.2 Ventricular Septal Defect Repair Fig. 5.45 The exposed VSD Recent advances in robotic instrumentation have facilitated totally endoscopic intracardiac procedures. However, due to relative complexity of ventricular septal defect (VSD) anatomy, totally endoscopic robotic VSD repair has not been reported in the literatures except those reported by our institution. 5.2.1 Indications of VSD for Surgery Adults with small restrictive VSDs who are asymptomatic often require no surgical intervention and should receive endocarditis prophylaxis as necessary. In general, if Op:Os ratio is >1.5:1 and the calculated pulmonary vascular resistance is under 6 U/m2, surgical closure of a VSD can be performed safely and is recommended. The development of a double-chambered right ventricle with outflow obstruction is also an indication for surgical intervention. The occurrence of infective endocarditis in an adult with a restrictive VSD is rare but compelling indication for repair of the defect [22]. 5.2.2 Anesthesia, Patient Position and CPB Establishment The anesthesia, position of patient and CPB establishment are the same as those previously described for atrial septal defect repair in Sect. 5.1. 5.2.3 Surgical Technique [23] The CPB is initiated with kinetically assisted bicaval venous. The intrathoracic part of the operation began robotically with pericardiotomy and placement of pericardial stay sutures. The pericardium is opened longitudinally 1.5 cm anteriorly to the phrenic nerve (Fig. 5.10). The incision is extended superiorly to expose the superior vena cava and then extended inferiorly to the diaphragm to visualize the inferior vena cava. The pericardium stay sutures are placed on the right side of pericardium to rotate the heart for optimal exposure of the atrium (Fig. 5.11). And the 3rd pericardium stay suture is placed on the left superior side of pericardium through anterior chest (16 Ga Angio) to expose the aorta (Fig. 5.12). The space between the vena cavae and the pulmonary veins are dissected clear (Figs. 5.13 and 5.14). And the linear tapes are placed around the inferior and superior vena cavae (Figs. 5.15 and 5.16). The aortic occlusion is performed with a Chitwood cross-clamp via the midaxillary line in the fourth ICS (Figs. 5.17 and 5.18). Antegrade cold blood cardioplegic solution is administered directly through the anterior chest (the 2nd ICS) with a 14 Ga Angiocatheter (Fig. 5.19). After snaring of the superior and inferior vena cavae, the right atrium is opened. The atrial retractor is applied through the fourth robotic arm. VSD is exposed through the tricuspid valve annulus (Fig. 5.45). Visualization of the perimembranous VSD edges is excellent with the assistance of valve hook. The membranous aneurysm is opened and the basal part of ventricular septal defect is exposed (Figs. 5.46 and 5.47). The defect is closed with interrupted sutures (Fig. 5.48) or Dacron patch (Fig. 5.49). The knot tying is performed extracorporeally by patient-side surgeon using a shafted knot pusher. The aortic clamp is released when the patient is rewarming. The tricuspid valve is repaired (Fig. 5.50) when no leakage and atrioventricular block are identified. The right atriotomy is closed using double-layer continuous 4-0 polytetrafluoroethylene running sutures. Then the patient is weaned from cardiopulmonary bypass. 74 Fig. 5.46 The membranous aneurysm is opened C. Gao and M. Yang Fig. 5.49 VSD closure with Dacron patch Fig. 5.50 The tricuspid valve is repaired Fig. 5.47 The basal part of VSD is exposed 5.2.4 Fig. 5.48 VSD closure with interrupted sutures Surgical Results and Learning Curves From 2009 to 2012, 20 patients with VSD, 11 female and 9 male, were operated on with “da Vinci S” or “da Vinci Si” Surgical System. Ages ranged from 16 to 45 years with an average of 29.0 ± 9.5 years. The echocardiography demonstrates the average diameter of perimembranous ventricular septal defect was (6.1 ± 2.8) mm, and a patent foramen ovale was found in one patient (Table 5.3). The VSD closure was secured with interrupted mattress sutures in 17 patients and patch closure in 3 patients (Table 5.4.). All cases were accomplished successfully without complications. The mean operation time was 225.0 ± 34.8 (180–300) min. And the mean CPB time was 94.3 ± 26.3 (70– 140) min; the mean cross-clamp time was 39.1 ± 12.9 (22 to 75) min. The postoperative TEE demonstrated intact ventricular septum. The mean hospital stay was 5 days. No residuary shunt was detected in an average of 14 months follow-up. 5 Robotic Surgery in Congenital Heart Diseases 75 Table 5.3 The baseline characteristics of robotic VSD closure at the PLA General Hospital (01/2009–01/2013) 20 120.00 CPB time (min) Variables Total number of patients Gender Male (%) Female (%) Age (year) Weight (kg) Height (cm) Diameter of defect (mm) Left ventricular ejection fraction (%) 140.00 9(45 %) 11(55 %) 29.0 ± 9.5 56.3 ± 8.2 160.7 ± 7.3 6.1 ± 2.8 66.9 ± 8.3 80.00 60.00 0.00 Table 5.4 Results of robotic perimembranous VSD repair 20 17(85 %) 3(15 %) 225.0 ± 34.8 94.3 ± 26.3 39.1 ± 12.9 4.6 ± 3.3 91.8 ± 60.8 5.0 ± 2.1 Operation time (min) 20.00 70.00 280.00 260.00 60.00 50.00 40.00 30.00 20.00 0.00 240.00 5.00 10.00 15.00 Case number 20.00 Fig. 5.53 The linear correlations of cross-clamp time with case number (r2 = 0.19, p = 0.046) 220.00 5.00 10.00 15.00 Case number 20.00 Fig. 5.51 The learning curve of operating time of VSD closure (y(min) = 258.25 − 16.18 ln(x); r2 = 0.221, p = 0.037) Significant learning curve was noted for operation time: y (min) = 258.25−16.18 ln(x) ⟮r2 = 0.221; P<0.05) (Fig. 5.51). The CPB and cross-clamp time decreased as the case number increased (Figs. 5.51, 5.52, and 5.53). 5.2.5 10.00 15.00 Case number 80.00 300.00 200.00 0.00 5.00 Fig. 5.52 The linear correlations of CPB time with case number (r2 = 0.14, p = 0.039) Cross–clamp time (min) Variables Procedure, n Direct closure, n (%) Patch closure, n (%) Operation time (min) Cardiopulmonary bypass time (min) Cross clamp time (min) Mechanical ventilation time (h) Drainage volume (ml) Length of stay (d) 100.00 Summary VSD closure can be completed through a conventional median sternotomy with low morbidity, relatively low cost, and excellent long-term results. However, patients are reluctant to undergo an operation because of the long incision in the midline of the chest. The incision leaves an unsightly scar that may be a source of persistent psychological disturbances and permanent dissatisfaction. Although the transcatheter closure of VSD has been used in some centers, the success rate of the procedure is low, and recurrence of the intracardiac shunt and the occluder dislodgment have been reported frequently. With the advent of computer-assisted robotic surgery, another option is offered for VSD closure without opening the chest. After over 300 cases of robotic cardiac surgery at the PLA General Hospital, Prof. Changqing Gao completed the first case of totally endoscopic robotic VSD repair on an adult patient using da Vinci robot in the world on the 22nd October 2009 [23]. We believe that the 76 C. Gao and M. Yang Fig. 5.55 One month after robotic VSD closure 5.3 Fig. 5.54 One week after robotic VSD closure possibility of closing all type of VSD regardless of the size and location could be realistic. The excellent exposure of whole VSD edges in the surgical field is paramount for successful VSD repair. In this group, the excellent visualization for VSD repair is achieved through the tricuspid valve annulus using dynamic atrial retractor to elevate the anterior leaflet of the tricuspid valve. Although in one case, the edges of the defect are a little difficult to be visualized because of multiple attachments of the septal defect to the edges of the defect, the visualization is well acceptable for repairing under the assistance of valve hook. In addition, the defect is carefully examined to establish that all edges can be seen well, and reached before repair is started. Our experience shows that the closure of VSD can be completed with a patch for a large one or direct suture for a small one without difficulties after a learning curve. The lack of a thoracotomy or a sternotomy should allow for a faster recovery and should quicken the patient’s return to a normal life style with excellent cosmetic result (Figs. 5.54, 5.55, and 5.56). The results are encouraging, however, a large study would be needed to confirm this concept. Partial Atrioventricular Septal Defect Repair Atrioventricular septal defects encompass a spectrum of lesions that are caused by maldevelopment of the endocardial cushions. Abnormalities of atrioventricular valve form and function and interatrial and interventricular communications may results. 5.3.1 Ostium Primum Defect with a Cleft Mitral Valve A 33-year-old female patient was admitted due to heart murmurs for 6 years. An ostium primum defect (2.5 × 3.0 cm) with a cleft mitral valve was confirmed (Fig. 5.57a), and moderate mitral valve regurgitation was revealed echocardiographically (Fig. 5.57b). The right atrium of the patient was enlarged and cardiac function was in class II (NYHA). The systolic heart murmur in the apex could be auscultated in physical examination. Electrocardiography showed sinus rhythm and left anterior branch block. Routine chest radiography revealed normal cardiothoracic ratio with mildly exaggerated bronchovascular markings. After inducing of general anesthesia, the intubation for single-lung ventilation and TEE were administrated. The right side of the chest was slightly elevated at 30o. Femoral arterial (18 F) and venous cannulation (23 F) was performed through a 2 cm transverse right groin incision with Seldinger guidewire method. And the cannulation was 5 Robotic Surgery in Congenital Heart Diseases 77 Fig. 5.56 Three months after robotic VSD closure, the surgical incision viewed from the front and right side a b Fig. 5.57 Preoperative echocardiography showed ostium primum defect (a) and mitral valve regurgitation (b) performed in the right internal jugular venous (15 F) under TEE guidance. Cardiopulmonary bypass was initiated with kinetically assisted bicaval venous drainage. The da Vinci Si camera and instrument arms were inserted in the right chest. A 2.0-cm incision was used as the working port in the fourth intercostals space of right chest. The aortic occlusion was performed with a Chitwood crossclamp via the midaxillary line in the fourth ICS. Antegrade cold HTK solution was administered directly through the anterior chest (second ICS) with a 14Ga Angiocatheter. Carbon dioxide was insufflated continuously into the operative field for air replacement. After lung deflation, the pericardium was opened and stay sutures were placed on the right side of pericardium to rotate the heart for optimal exposure of the left atrium. A right atrium incision was made and the atrial retractor was applied. A partial atrioventricular septal defect with estimated dimensions of 2.5 × 3.0 cm was found (Fig. 5.58), and the mitral valve cleft with a normal mitral annulus was also found (Fig. 5.59a). Repair of the mitral valve cleft proceeded by precise placement of simple Gortex sutures in the cleft, beginning at its base and moving centrally until the first set of chordal attachment was approached (Fig. 5.59b). The valve was then tested again with saline solution. Absolutely 78 C. Gao and M. Yang Fig. 5.58 The 2.5 × 3.0-cm partial atrioventricular septal defect a b Fig. 5.59 The 0.2-cm cleft in A2 segment (a), and the cleft was repaired using interrupted suture (b) alignment of the cleft in all its dimensions was of critical importance. The interatrial communication was then closed with a patch. The patch was placed with interrupted suture technique, beginning at the base of the mitral cleft (Fig. 5.60a). The suture line continued to the surgeon’s right, where the critical area of the conduction system and the coronary sinus were located. The edge of the patch was sutured superficially to the mitral valve tissue that was adherent to the underlying ventricular septal crest. Suture depth was critical, as the proximal conduction bundles traveled along the underlying crest of the ventricular septum at this level. As the suture line approached the inferiormost extent of the ventricular septal crest, it should be directed well to the right ventricular side of the crest, using the available tissue from the right-side atrialventricular valve inferior leaflet. As the annulus was approached, the suture line undergoes transition from atrioventricular valve tissue to the atrial free wall. The patch repair allowed the coronary sinus to drain to the right atrium (Fig. 5.60b). The sinus rhythm was observed on the electrocardiogram monitor after release of the aortic cross-clamp. The right atriotomy was closed using double-layer continuous 4-0 Gortex running sutures. The bypass weaned from CPB after the patient was rewarmed. The ports were closed and the femoral vessels were decannulated. The total operative time was 320 min; total bypass time and ischemic time was 165 and 126 min respectively. The patient was ventilated for 6 h. The postoperative course was uneventful and the patient was discharged from the hospital on the eighth postoperative day with excellent results (Fig. 5.61a, b). And the ECG showed sinus rhythm, right bundle branch block and first-degree atrioventricular block. 5 Robotic Surgery in Congenital Heart Diseases 79 a b Fig. 5.60 The interrupted suture line was placed on the tricuspid valve side (a), and the continued line was placed inferiorly on the atrial wall, then under the lip of the coronary sinus and back to the edge of the ostium primum defect (b) a b Fig. 5.61 Postoperative echocardiography showed the patch closure of the defect (a) and good mitral valve function (b) 80 5.4 C. Gao and M. Yang Summary In the mid-1990s, cardiac surgeons recognized the significant advantages of minimizing surgical trauma by reducing incision size. A series of clinic reports demonstrate that robotic atrial septal defect repair is safe and has excellent results [10–15]. However, total robotic partial atrioventricular septal defect repair combined with mitral valve repair has not been reported in the literatures to our knowledge. After 500 cases of robotic cardiac surgery, including 120 cases of ASD and 20 cases of VSD repair surgery, we performed the totally robotic partial atrioventricular septal defect repair. In terms of ostium primum defect with a cleft mitral valve, author’s understanding is as follows: excellent exposure is the key to successful operation. The robotic surgical system provides us with a satisfying surgical field of right atrium, tricuspid and mitral valve. With the assistance of the dynamic atrial retractor by the fourth arm, ostium primum defect can be perfectly identified through the right atrium incision. Robotic surgical system enables surgeons to perform complex repairs using optimized, high-definition visualization and fine dexterity [24, 25]. When an ostium primum interatrial defect is present with a left mitral valve, the approach is exclusively through a right atrial incision. The mitral valve is addressed first, looking through the atrial defect. Repair of the mitral valve cleft proceeds by precise placement of simple Gortex sutures in the cleft, beginning at its base and moving centrally until the first set of chordal attachment are approached. The valve is then tested again with saline. If central coaptation is adequate, the repair is complete. Absolute alignment of the cleft in all its dimensions is of critical importance. The interatrial communication is then closed with a patch. The patch is placed with a running suture technique using Gortex suture, beginning at the base of the mitral cleft. The suture line continues to the surgeon’s right, where the critical area of the conduction system and the coronary sinus are located. The edge of the patch is sutured superficially to the mitral valve tissue that is adherent to the underlying ventricular septal crest. Suture depth is critical, as the proximal conduction bundles travel along the underlying crest of the ventricular septum at this level. As the suture line approaches the inferiormost extent of the ventricular septal crest, it should be directed well to right ventricular side of the crest, using the available tissue from the right-side atrialventricular valve inferior leaflet. As the annulus is approached, the suture line undergoes transition from atrioventricular valve tissue to the atrial free wall. The patch repair allows the coronary sinus to drain to the right atrium. We believe that robotic surgery for partial atrioventricular septal defect should be feasible and safe with good cosmetic outcomes for selected patients [26]. References 1. Lewis FJ, Taufic M. Closure of atrial septal defects with the aid of hypothermia: experimental accomplishments and the report of the one successful case. Surgery. 1953;33:52. 2. Murphy JG, Gersh BJ, McGoon MD, et al. Long-term outcomes after surgical repair of isolated atrial septal defect. Follow-up at 27 to 32 years. N Engl J Med. 1990;323:1645–50. 3. Minale C. Atrial septal defect closure through a thoracotomy. Ann Thorac Surg. 1997;63:913–4. 4. Rao PS, Sideris EB, Hausdorf G, et al. International experience with secundum atrial septal defect occlusion by the buttoned device. Am Heart J. 1994;128:1022–35. 5. Ewert P, Berger F, Daehnert I, et al. Transcatheter closure of atrial septal without fluoroscopy. Feasibility of new method. Circulation. 2000;101:847–9. 6. Webb G, Gatzoulis MA. Atrial septal defects in the adult: recent progress and overview. Circulation. 2006;114:1645–53. 7. Izzat MB, Yim AP, El-Zufari MH. Limited access atrial septal defect closure and the evolution of minimally invasive surgery. Ann Thorac Cardiovasc Surg. 1998;4:56–8. 8. Galloway AC, Shemin RJ, Glower DD, et al. First report of the port-access international registry. Ann Thorac Surg. 1999; 67:51–8. 9. Chitwood Jr WR, Elbeery JR, Moran JF. Minimally invasive mitral valve repair using transthoracic aortic occlusion. Ann Thorac Surg. 1997;63:1477–9. 10. Torracca L, Ismeno G, Alfieri O. Totally endoscopic computerenhanced atrial septal defect closure in six patients. Ann Thorac Surg. 2001;72(4):1354–7. 11. Wimmer-Greinecker G, Dogan S, Aybek T, et al. Totally endoscopic atrial septal repair in adults with computer-enhanced telemanipulation. J Thorac Cardiovasc Surg. 2003;126(2): 465–8. 12. Argenziano M, Oz MC, Kohmoto T, et al. Totally endoscopic atrial septal defect repair with robotic assistance. Circulation. 2003;108 Suppl 1:II191–4. 13. Bonaros N, Schachner T, Oehlinger A, et al. Robotically assisted totally endoscopic atrial septal defect repair: insights from operative times, learning curves, and clinical outcome. Ann Thorac Surg. 2006;82(2):687–93. 14. Gao C, Yang M, Wang G, et al. Totally robotic resection of myxoma and atrial septal defect repair. Interact Cardiovasc Thorac Surg. 2008;7(6):947–50. 15. Gao C, Yang M, Wang G, Wang J, Xiao C, Wu Y, Li J. Totally endoscopic robotic atrial septal defect repair on the beating heart. Heart Surg Forum. 2010;13(3):E155–8. 16. Salerno TA, Suarez M, Panos AL, Macedo FI, Alba J, Brown M, Ricci M. Results of beating heart mitral valve surgery via the transseptal approach. Rev Bras Cir Cardiovasc. 2009;24(1):4–10. 17. Modi P, Rodriguez E, Chitwood WR. Robot assisted cardiac surgery. Interact Cardiovasc Thorac Surg. 2009;9(3):500–5. 18. Kypson AP, Chitwood WR. The use of robotics in cardiovascular surgery. Future Cardiol. 2005;1(4):61–7. 19. Rosas M, Zabal C, Garcia-Montes J, et al. Transcatheter versus surgical closure of secundum atrial septal defect in adults: impact of age at intervention: a concurrent matched comparative study. Congenit Heart Dis. 2007;2(3):148–55. 20. Bijulal S, Sivasankaran S, Ajitkumar VK. An unusual thrombotic complication during percutaneous closure of atrial septal defect. J Invasive Cardiol. 2009;21(2):83–5. 21. Baird CW, Stamou SC, Skipper E, et al. Total endoscopic repair of a pediatric atrial septal defect using the da Vinci robot and hypothermic fibrillation. Interact Cardiovasc Thorac Surg. 2007;6(6): 828–9. 5 Robotic Surgery in Congenital Heart Diseases 22. Cohn L. Cardiac surgery in the adult. 4th ed. New York: McGrawHill Professional; 2011. 23. Gao C, Yang M, Wang G, et al. Totally endoscopic robotic ventricular septal defect repair. Innovations (Phila). 2010;5(4):278–80. 24. Chitwood WR. Current status of endoscopic and robotic mitral valve surgery. Ann Thorac Surg. 2005;79:S2248–53. 81 25. Yang M, Gao C, Wang G, et al. Robotic-assisted endoscopic atrial septal defect closure: analysis of 115 cases in a single center. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2012;32(7):915–8. 26. Gao C, Yang M, Wang G, et al. Totally endoscopic robotic ventricular septal defect repair in the adult. J Thorac Cardiovasc Surg. 2012;144:1404–7. 6 Totally Robotic Myxoma Excision Changqing Gao and Ming Yang Abstract A median sternotomy approach with ascending aortic and bicaval cannulation is usually employed. In recent years, minimally invasive approaches are being applied with increasing frequency in all areas of cardiac surgery, and also in surgery for cardiac tumors. Over the past few years, computerized surgical robotic systems have been developed very rapidly. The da Vinci surgical robot has assisted the surgeon’s work using telemanipulation through a master-controller activation principle with a 3-D intracardiac camera. In 2005, Murphy and associates reported the initial successful experience with left atrial myxoma excision with the da Vinci Surgical System. Subsequently, the largest series of robotic resection of atrial myxomas with no operative deaths or strokes was reported by Gao et al. at the PLA General Hospital in Beijing, China in 2010. In this chapter, robotic resection of atrial myxoma will be discussed. Traditionally, left atrial myxomas have been resected by median sternotomy with cardiopulmonary bypass. Recent advances in robotic instrumentation have facilitated endoscopic intracardiac procedure. The initial successful robotic resection of left atrial myxoma was reported in 2005, and the largest case series was reported by Dr. Changqing Gao (Gao C) at the PLA General Hospital, Beijing, China in 2011. The experience of robotic myxoma resection is still limited. This chapter is to discuss a surgical approach for ideal and safe resection of atrial myxoma using the da Vinci Surgical System. The robotic myxoma resection is technically feasible in all stable and selective patients without the fear of inadequate intraoperative exposure. Results in this limited number of selected patients are satisfactory, but more experience and longer follow-up are still needed before this can be recommended as a standard approach. Neoplasms of the heart can be divided into primary cardiac tumors arising in the heart and secondary cardiac tumors that have metastasized to the heart. Primary cardiac tumors are uncommon and represent only 5–10 % of all neoplasms of the heart and pericardium. Primary cardiac tumors can be further stratified into benign and malignant tumors. Approximately 80 % of primary cardiac tumors are benign. Approximately 50 % of the benign tumors are myxomas C. Gao, MD (*) • M. Yang, MD Department of Cardiovascular Surgery, PLA General Hospital, No. 28 Fuxing Road, Beijing 100853, People’s Republic of China e-mail: gaochq301@yahoo.com [1–4]. Myxomas occur in any chamber of the heart but have a special predilection for the left atrium, in which approximately 75 % originate. The next most frequent site is the right atrium, where 10–20 % are found. Surgical resection is the only effective therapeutic option for patients with cardiac myxoma and should not be delayed because death from obstruction to flow within the heart or embolization may occur in as many as 8 % of patients awaiting operation [5, 6]. A median sternotomy approach with ascending aortic and bicaval cannulation is usually employed. In recent years, the minimally invasive approaches are being applied with increasing frequency in all areas of cardiac surgery, which include cardiac tumors. But minimally invasive surgical C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_6, © Springer Science+Business Media Dordrecht 2014 83 84 C. Gao and M. Yang Fig. 6.1 The pericardium is opened longitudinally anteriorly to the phrenic nerve experience in treatment of cardiac tumors is quite limited. Approaches include right parasternal or partial sternotomy exposure with standard cardioplegic techniques [7], right submammary incision with femoral-femoral bypass and nonclamped ventricular fibrillation [8], and the right submammary port access method with antegrade cardioplegia and ascending aortic balloon occlusion [9, 10]. Over the past few years, computerized surgical robotic systems have been developed very rapidly. The da Vinci surgical robot has assisted the surgeon’s work using telemanipulation through a master-controller activation principle with a 3-D intracardiac camera. In 2005, Murphy and associates [11] reported the initial successful experience with left atrial myxoma excision with the da Vinci Surgical System. Subsequently, the largest series of robotic resection of atrial myxomas with no operative deaths or strokes was reported by Dr. Changqing Gao et al. at the PLA General Hospital in Beijing, China in 2010 [10]. In this chapter, the largest series of robotic resection of atrial myxoma will be discussed. 6.1 Fig. 6.2 Vertical stay sutures placed on the right side of pericardium Fig. 6.3 Stay suture on the left superior side of pericardium to expose the ascending aorta Anesthesia, Patient Position and CPB Establishment The anesthesia, da Vinci Surgical System setup and CPB establishment are as previously described for atrial septal defect repair in Chap. 5. Fig. 6.4 The Chitwood cross-clamp is put in the ascending aorta 6.2 Surgical Technique The initial preparation is the same as ASD repair, and after the da Vinci Surgical System is docked, the operation starts. The pericardium is opened longitudinally anteriorly to the phrenic nerve (Fig. 6.1). The incision is extended superiorly to expose the aorta. Then the vertical stay sutures are placed low on the pericardium on the right side (Fig. 6.2) and the left superior side (Fig. 6.3) to rotate the heart for optimal exposure of the atrium and aorta. The aortic is occluded with a Chitwood cross-clamp in the fourth ICS via the midaxillary line (Fig. 6.4). Antegrade cold blood cardioplegic solution is administered directly through the anterior chest (the 2nd ICS) with a 14-F angiocatheter (Figs. 6.5 and 6.6). 6 Totally Robotic Myxoma Excision Fig. 6.5 The 14-F angiocatheter is punctured into the thoracic cavity on the second ICS in the anterior chest 85 Fig. 6.8 Exposing the left atrial myxoma with atrial retractor Fig. 6.6 The 14-F angiocatheter is punctured into the aorta for cardioplegic solution administration Fig. 6.9 The papillar myxoma in the left atrium Fig. 6.7 The left atriotomy anterior to the pulmonary veins for the left atrial myxoma A left atriotomy anterior to the pulmonary veins is performed (Fig. 6.7) and exposure of left atrial myxomas is maximized with the atrial retractor (Figs. 6.8, 6.9, and 6.10). For left atrial tumors, the vena cavae are not taped, allowing an increased mobility and exposing the left atrial cavity. Fig. 6.10 The villous myxoma in the left atrium 86 C. Gao and M. Yang Fig. 6.11 Total excision by dissecting a plane through the atrial muscle at the point of attachment Fig. 6.13 The attachment of myxoma after total excision Fig. 6.12 Total excision of left myxoma The left atriotomy can be extended behind both cavae for greater exposure. Total excision is achieved by dissecting a plane through the atrial muscle at the point of attachment (Figs. 6.11 and 6.12). The subendocardial defects are also directly closed with 4-0 polytetrafluoroethylene running suture without pericardial patches (Figs. 6.13 and 6.14). The atrial septal defects originated from the resection can be repaired with autologous pericardial patches with 4-0 polytetrafluoroethylene running suture. Four right atrial myxomas are completely resected from the beating heart with the superior and inferior venae cavae snared avoiding the aorta clamp and cardioplegia administration (Figs. 6.15 and 6.16). Right atrial myxomas pose special venous cannulation problems. Intraoperative echocardiography may be of benefit in allowing safe cannulation. Robotic surgery is constantly safer for right atrial myxomas than sternotomy because of cannulation of the jugular or femoral vein. The tricuspid valve and the right atrium should be inspected carefully in patients with right atrial myxoma, with or without familial myxoma. Regardless of the Fig. 6.14 Suturing the subendocardial defects Fig. 6.15 The right atrial myxoma is resected on the beating heart surgical approach, the ideal resection compasses the tumor and a portion of the cardiac wall or interatrial septum to which it is attached. It is controversial whether 6 Totally Robotic Myxoma Excision Fig. 6.16 The right atrial myxoma is exposed with the aid of atrial retractor 87 Fig. 6.18 The closed cardioplegia site Fig. 6.19 The pre-operative TEE shows the left atrial myxoma Fig. 6.17 The cardioplegia site is closed with extracorporeal knot tying excision of full-thickness wall is necessary or excision of only an endocardial attachment is sufficient to prevent recurrence. Our policy is to resect full thickness whenever possible. However, only partial-thickness resection of the area of tumor attachment has been performed when anatomically necessary without a noted increase in recurrence rate [12]. Every care should be taken to remove the tumor without fragmentation. When the tumor is removed from the field, the area should be liberally irrigated, suctioned, and inspected. The atrial is closed with running sutures after total resection. For excision in arrested heart, after crossclamp release and meticulous intracardiac deairing by angiocatheter of antegrade cold blood cardioplegic solution, the patient is weaned from CPB. After removal of the cardioplegia angiocatheter, the cardioplegia site is closed with extracorporeal knot tying through the working port (Figs. 6.17 and 6.18), and then chest tubes are inserted. The surgical result and integrity of the septal closure are confirmed by TEE (Figs. 6.19 and 6.20). Fig. 6.20 The surgical resection and integrity of the septal closure are confirmed by TEE 6.3 Postoperative Management After the operation, patients are monitored at the ICU and discharged to an intermediate care unit as soon as hemodynamics and spontaneous respiration have been adequately 88 C. Gao and M. Yang Table 6.1 The clinical data of robotic atrial myxoma resection Table 6.2 The results of robotic atrial myxoma resection Variables Total number of patients Gender Male (%) Female (%) Age (year) Weight (kg) Height (cm) Attachment sites Interatrial septum, n (%) Posterocaudal wall, n (%) Root of the anterior leaflet of mitral valve, n (%) Left atrial roof, n (%) Right atrium, n (%) Shape Spherical/encapsulated, n (%) Villous, n (%) Diameter of myxoma (mm) Left ventricular ejection fraction (%) Combined intracardiac diseases Sever mitral valve regurgitation Patent foramen ovale Variables Procedure, n Through a left atriotomy, n (%) Through an oblique right atriotomy, n (%) On beating heart, n (%) Combined with mitral valve repair, n (%) Combined with mitral patent foramen ovale closure, n (%) Operation time (min) Cardiopulmonary bypass time (min) Cross clamp time (min) Mechanical ventilation time (h) Drainage volume (mL) Length of stay (days) 45 12 (32.5 %) 33 (67.5 %) 47.0 ± 14.1 62.3 ± 11.8 162.0 ± 6.8 31 (77.5 %) 2 (5 %) 2 (5 %) 1 (2.5 %) 4 (10 %) 22 (55 %) 18 (45 %) 43 × 52 68.9 ± 8.1 2 1 1 stabilized. Chest drains are removed when drainage reaches less than 50 mL/12 h. All patients undergo transthoracic echocardiography immediately before discharge from hospital and at 3 months after the procedure. 6.4 Surgical Experience and Learning Curves Between July 2007 and May 2013, robotic myxoma resection with da Vinci S or Si Surgical System was performed on 45 consecutive patients at the authors’ hospital. Twelve patients were male and 33 female. The mean age was 47.0 ± 14.1 years old (ranging from 13 to 66). Two patients had preoperative cerebral infarction. The mean tumor size was 43 × 52 mm (14 × 19–44 × 74 mm). Four tumors were found in the right atrium and 36 tumors were found in the left atrium, of which 31 tumors arose from the interatrial septum, 2 from the posterocaudal wall, 2 from the root of the anterior leaflet of the mitral valve, and 1 from the left atrial roof. One left atrial myxoma was combined with severe mitral valve regurgitation. One patient was diagnosed with left atrial myxoma and patent foramen ovale (Table 6.1). In 34 patients, the tumors were explored through a left atriotomy anterior to the pulmonary veins and were exercised by dissecting a plane through the atrial muscle at the point of attachment. In the first two patients, the tumors were explored and exercised through an oblique right atriotomy. 45 34 (85 %) 2 (5 %) 4 (10 %) 1 (2.5 %) 1 (2.5 %) 288.1 ± 41.4 90.9 ± 29.1 46.4 ± 16.3 4.7 ± 3.2 101.8 ± 58.8 4.6 ± 2.1 Four right atrial myxomas were resected on the beating heart (Table 6.2). The da Vinci instrument arms were inserted through three 0.8 cm trocar incisions at the right side of the chest. Via four port incisions and a 1.5–2 cm working port, all the procedures were completed with da Vinci S or da Vinci Si robot. The mean operation time, cardiopulmonary bypass (CBP) time and cross clamp time were calculated. And the learning curves were assessed by means of regression analysis with logarithmic curve fit. Follow-up was conducted with echocardiography which was used as the diagnostic tool. All cases turned out to be successful. One formal artery arterial embolism was observed on the 5th postoperative day and was cured through embolectomy. Two patients required combined cardiac surgery: one mitral valve repair, and one patent foramen ovale closure. The mean operation time was 288.1 ± 41.4 (180–390) min, and the mean CPB time was 90.9 ± 29.1 (62–156) min, the mean cross-clamp time was 46.4 ± 16.3 (24–97) min. Significant learning curves were noted for operating time, CPB time and cross-clamp time (Figs. 6.21, 6.22 and 6.23). And the operating time was stable after 20 cases. All the patients were discharged with excellent cosmetic results (Figs. 6.24 and 6.25). No patients were lost to follow-up, and the mean follow-up was 24 ± 14 months. There were no deaths during hospitalization or at follow-up. No patient required reoperation for recurrence postoperatively. 6.5 Summary Cardiac myxoma is a benign gelatinous growth composed of primitive connective tissue cells and stroma resembling mesenchyme, which is usually pedunculated and arises from the interatrial septum, near the fossa ovalis [13]. Grossly, about 6 Totally Robotic Myxoma Excision 89 100.00 Cross−clamp time (min) Operation time (min) 400.00 300.00 200.00 100.00 0.00 80.00 60.00 40.00 10.00 20.00 Case number 30.00 40.00 Fig. 6.21 The learning curve of operation time (y(min) = 366.6 − 37.9 ln(x); r2 = 0.346, p = 0.000) 20.00 0.00 10.00 20.00 Case number 30.00 40.00 Fig. 6.23 The learning curve of cross-clamp time (y(min) = 70.5 − 11.2 ln(x); r2 = 0.64, p = 0.00 0) CPB time (min) 150.00 125.00 100.00 75.00 50.00 0.00 10.00 30.00 20.00 Case number 40.00 Fig. 6.22 The learning curve of CPB time (y(min) = 136.2 − 20.1 ln(x); r2 = 0.53, p = 0.000) two-thirds of myxomas are round or oval tumors with a smooth or slightly lobulated surface (Figs. 6.26 and 6.27). Most are polypoid, relatively compact, pedunculated and mobile. Embolism is a major feature of cardiac myxomas, with systemic embolism occurring in 30–45 % of patients with a left atrial tumor. In 2005, Murphy and associates [11] reported the initial successful experience with left atrial myxoma excision with the da Vinci Surgical System. To date, other approaches for better exposure and ideal resection of left or right atrial myxomas with the da Vinci S Surgical System have not been reported. The surgical principles of myxoma excision include exposure of the attachment point of the tumor which allows excision of adequate tissue margins, removal of the Fig. 6.24 The port incision view after robotic myxoma resection for 1 week tumor without fragmentation, reconstruction of atrial wall defects, and the ability to inspect the cardiac chambers for other tumors [13]. Exposure of left atrial myxomas is maximized by principles from mitral valve repair surgery with atrial retractors when the right side of the heart to rotate up and the left side of the heart to rotate down. Therefore, stay sutures are placed low on the pericardium on the right side. This rotates the heart for optimal exposure of the left atrium. For left atrial tumors, the superior vena cava is extensively mobilized as is the inferior vena cava–right atrial junction, allowing an increased mobility and exposure of the left 90 C. Gao and M. Yang Fig. 6.27 The oval myxoma with a smooth or slightly lobulated surface Fig. 6.25 The excellent cosmetic results after robotic myxoma resection for 1 month Fig. 6.26 The lathy myxoma atrial cavity. Left atrial myxomas could be approached by an incision through the anterior wall of the left atrium anterior to the right pulmonary veins. This incision could be extended behind both cavae for greater exposure [12]. Right atrial myxomas could be resected directly through the right atrial incision from the beating heart without an aortic cross clamp [10]. The atrial retractor is an excellent device for atrial exposure through the fourth arm. This device offers superior identification of the tumor attachment points to those that have been achieved in patients in whom the surgical approach has been via median sternotomy [10]. Furthermore, left atrial myxomas can be approached more easily by the left atrial approach than the right; thus the stalk can be easily found and total excision can be achieved by dissecting a plane through the atrial muscle at the point of attachment with magnification [10]. Left atrial myxomas were resected in 34 of our 40 patients through left atrial approach. Regardless of the surgical approach, the ideal resection encompasses the tumor and a portion of the cardiac wall or interatrial septum to which it is attached [12]. It has been controversial whether excision of full-thickness wall or only the endocardial attachment is sufficient to prevent recurrence. Our policy is to resect full thickness whenever possible. When the stalk of myxoma originates in the septum, we try to resect the stalk together with full septum, and the septum is then repaired. Actis Dato [14], McCarthy and their associates [15] reported that only partial thickness resection of the area of tumor attachment was performed when anatomically necessary without a noted increase in recurrence rate [12]. In our study, we found that some stalks of myxoma were loosely attached to the endocardium, which could be easily resected robotically because of the 10× magnification. When the stalk of myxoma was not completely resected, we cauterized the stalk of the myxoma to prevent recurrence [10]. Chitwood’s aortic clamp technique [16] is safe, simple, and economical compared with the remote access perfusion 6 Totally Robotic Myxoma Excision cannula with endoaortic balloon. In our series, aortic occlusion is completed with the Chitwood crossclamp via the fourth ICS in the midaxillary line. Cardioplegic solution administered antegradely directly through the anterior chest wall is feasible and safe [17]. Therefore, the working port could become smaller. In our series, the robotic system could be operated safely and efficiently, causing no operative deaths or conversions resulting from a system malfunction. Only two patients had temporary atrial fibrillation. Mean length of hospital stay was shorter than that with conventional surgical repair. These patients benefited from minimal trauma, early discharge, and excellent cosmesis [10]. We conclude that robotic myxoma resection is technically feasible and could be applied as a routine access in all stable and selective patients without the fear of inadequate intraoperative exposure. Surgical results are excellent. It is important to remember that the use of a minimally invasive technique must not compromise complete surgical excision. Results in this limited number of selected patients are satisfactory, but more experience and longer follow-up are still needed before this can be recommended as a standard approach. 6.6 Case Report 6.6.1 Totally Robotic Left Atrial Myxoma Excision Associated Mitral Valve Plasty An 18-year-old female patient was admitted because of progressive post-exercise despnea in the previous 5 months. On echocardiographic examination, a mass measuring 6.4 × 3.8 cm was discovered attached to the middle part of interatrial septum (Fig. 6.28a). The mass showed no signs of calcification or breakdown. Simultaneously, echo revealed a 0.2 cm cleft between A2 and A3 segment and the dilated mitral annulus, which led to severe mitral valve regurgitation (Fig. 6.28b). The patient had a NYHA III heart function and enlarged left atrium. The systolic heart murmur in the apex could be auscultated in clinical examination. Electrocardiography showed sinus tachycardia. Routine chest radiography revealed normal cardiothoracic ratio with mildly exaggerated bronchovascular markings. All laboratory tests were in normal ranges. After general anesthesia, the intubation for single-lung ventilation and transesophageal echocardiography (TEE) were established. The right side of the chest was slightly elevated at 30°. Femoral arterial (17 F) and venous cannulation (21 F) were performed through a 2-cm transverse right groin incision cutdown with Seldinger guidewire method and TEE guidance. Cardiopulmonary bypass (CPB) was initiated with kinetically assisted bicaval venous drainage. The da Vinci S camera and instrument arms were inserted through 91 a b Fig. 6.28 Preoperative echocardiography shows left atrial myxoma (a) and mitral valve regurgitation (b) 1-cm ports in the right chest. 3 cm below the camera port, a 2.5-cm incision was used as the working port in the fourth intercostals space (ICS) of right chest. The aortic occlusion was performed with a Chitwood cross clamp via the midaxillary line in the fourth ICS. Antegrade cold blood cardioplegic solution was administered directly through the anterior chest (second ICS) with a 14 F angiocatheter. Carbon dioxide was insufflated continuously into the operative field for air replacement. After lung deflation, the pericardium was opened and the stay sutures were placed on the right side of pericardium to rotate the heart for optimal exposure of the left atrium. A longitudinal incision, posterior to Waterstone’s groove was made and the atrial retractor was applied. Exposure revealed a mass soft, gelatinous, reddish brown, oval in shape, smooth surface with estimated dimensions of 6.4 × 3.8 cm, attached to the interatrial septum (Fig. 6.29a). The mass had neither calcified deposits nor areas of hemorrhage or necrosis. A meticulous dissection was made to ensure complete resection without any residues. The tumor was deposited into an Endopouch Retriever and extracted via the working port. 92 a C. Gao and M. Yang provided. The postoperative course was uneventful and the patient was discharged from the hospital on the eighth postoperative day without any complications. References b Fig. 6.29 Resection of myxoma at the point of attachment (a) and the good result of mitral valve repair (b) The mitral valve was inspected and examined revealing a 0.5-cm cleft between A2 and A3 segment and an enlarged mitral annulus. The two leaflets were reapproximated using interrupted suture (Fig. 6.29b), and a Cosgrove-Edwards annuloplasty band was implanted. And the left atriotomy was closed using double-layer continuous 4-0 polytetrafluoroethylene running sutures. Standard postoperative care was 1. Prichard RW. Tumors of the heart: review of the subject and report of one hundred and fifty cases. Arch Pathol. 1951;51:98–128. 2. Gerbode F, Keith WJ, Hill JD. Surgical management of tumors of the heart. Surgery. 1967;61:94–101. 3. McAllister HA, Fenoglio Jr JJ. Tumors of the cardiovascular system. In: Rubinstein L, editor. Atlas of tumor pathology, Series Ishington. Washington, DC: Armed Forces Institute of Pathology; 1978. 4. Silverman NA. Primary cardiac tumors. Ann Surg. 1980;91:127. 5. Sutton D, Al-Kutoubi MA, Lipkin DP. Left atrial myxoma diagnosed by computerized tomography. Br J Radiol. 1982;55:80. 6. Symbas PN, Hatcher Jr CR, Gravanis MB. Myxoma of the heart: clinical and experimental observations. Ann Surg. 1976;183:470. 7. Ravikumar E, Pawar N, Gnanamuthu R, et al. Minimal access approach for surgical management of cardiac tumors. Ann Thorac Surg. 2000;70:1077. 8. Ko PJ, Chang CH, Lin PJ, et al. Video-assisted minimal access in excision of left atrial myxoma. Ann Thorac Surg. 1998;66:1301. 9. Gulbins H, Reichenspurner H, Wintersperger BJ. Minimally invasive extirpation of a left-ventricular myxoma. Thorac Cardiovasc Surg. 1999;47:129. 10. Gao C, Yang M, Wang G, et al. Excision of atrial myxoma using robotic technology. J Thorac Cardiovasc Surg. 2010;139:1282–5. 11. Murphy DA, Miller JS, Langford DA, Snyder AB. Robot-assisted endoscopic excision of left atrial myxomas. J Thorac Cardiovasc Surg. 2005;130:596.597. 12. Cohn L. Cardiac surgery in the adult. 4th ed. New York: McGrawHill Professional; 2011. 13. Schroeyers P, Vermeulen Y, Wellens F, De Geest R, Degrieck I, Van Praet F, et al. Video-assisted port-access surgery for radical myxoma resection. Acta Chir Belg. 2002;102:131–3. 14. Actis Dato GM, de Benedictus M, Actis Dato Jr A, Ricci A, Sommarival L, De Paulis R. Long-term follow-up of cardiac myxoma (7–31 years). J Cardiovasc Surg (Torino). 1993;34:41–3. 15. McCarthy PM, Piehler JM, Schaff HV, Pluth JR, Orszulak TA, Vidaillet Jr HJ, et al. The significance of multiple, recurrent, and “complex” cardiac myxomas. J Thorac Cardiovasc Surg. 1986;91: 389–96. 16. Chitwood WR, Elbeery JR, Moran JM. Minimally invasive mitral valve repair: using a mini-thoracotomy and transthoracic aortic occlusion. Ann Thorac Surg. 1997;62:1477–9. 17. Gao C, Yang M, Wang G, Wang J. Totally robotic resection of myxoma and atrial septal defect repair. Interact Cardiovasc Thorac Surg. 2008;7:947–50. 7 Robotic Mitral Valve Surgery Changqing Gao and Ming Yang Abstract Mitral valve repair surgery has advanced markedly over the past 25 years with excellent long-term outcomes. And the significant advances in surgical optics, instrumentation, and perfusion technology have allowed surgeons to perform mitral valve surgery using progressively smaller incisions. Due to its excellent therapeutic results, minimally invasive mitral valve surgery has become a standard of care at quite some specialized centers worldwide. The da Vinci robotic surgical system, an embodiment of minimally invasive surgical tools, was introduced to mitral valve surgery in 1998. And Chitwood further refined the endoscopic approach, taking advantage of the da Vinci robotic surgical system and its advanced robotic technology to repair complex mitral valve pathology through port incisions using optimized, high-definition visualization and fine dexterity. The excellent clinical outcomes are built on the foundation of stepwise improvement in surgeon’s techniques with a gradual learning curve. This chapter covers robotic mitral valve repair and replacement. Mitral valve surgery has conventionally been performed through the median sternotomy with conventional cardiopulmonary bypass. Due to its more complex nature and requirement of cardiopulmonary, cardiac surgery lagged far behind other surgical fields in the development of minimal access methods until 1995. After closed-chest cardiopulmonary bypass and cardioplegic arrest were practiced, reduction of incision size became possible. The valve surgery through small incision has become a standard practice at many clinical centers. Loulmet and Carpentier [1] classified minimally invasive cardiac surgery into four levels: direct-vision approaches (Level I), video-assisted procedures (Level II and III), and the robotic valve operations (Level IV). C. Gao, MD (*) • M. Yang, MD Department of Cardiovascular Surgery, PLA General Hospital, No. 28 Fuxing Road, Beijing 100853, People’s Republic of China e-mail: gaochq301@yahoo.com 7.1 Level I: Direct-Vision and Mini-Incision Initially, minimally invasive cardiac valve surgery was based on modifications of previously used incisions and performed under direct vision. Alternative incisions to expose the mitral valve, including partial sternotomies, parasternal incisions and mini-thoracotomies, are the initial approaches to repair the mitral valve while optimizing cosmesis. Cosgrove, Cohn, Gundry and Arom [2–5] showed that mitral valve operations could be done with incisions other than a median sternotomy with low surgical mortality (1–3 %) and morbidity. In early 1996, the Stanford group [6, 7] performed the first mini-incision mitral valve surgery (MIMVS) using intra-aortic balloon occlusion (Port access) and cardioplegia. By December 1998, Cosgrove had done 250 minimally invasive mitral valve operations using either a ministernotomy or parasternal incision with no mortality [8]. In fact, the annulus of the mitral valve is nearly in the sagittal plane of the body, making a right mini-thoracotomy the optimal approach to the valve. This approach provides a direct enface view of the mitral valve, although the distance to the mitral valve is further. C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_7, © Springer Science+Business Media Dordrecht 2014 93 94 C. Gao and M. Yang These encouraging results confirmed the feasibility and safety of these techniques and further advanced the next level of “minimally invasiveness”. vision could transpose surgical manipulations from outside the chest wall to deep within cardiac chambers. 7.4 7.2 Level II: Video-Assisted and Microincisions The radical endoscopic surgical techniques initiated a wave of new surgical approaches in general, orthopedic, urologic, and gynecologic procedures and became routine operations in the 1990s. In contrast, fine vascular anastomotic and complex reparative procedures are the centerpieces of cardiac surgery. Because of the difficulty in acquiring the fine video-assisted dexterity needed for these operations, cardiac surgeons are reluctant to explore the benefits of operative video assistance. Microincisions are considered as 4–6 cm skin incisions, and video assistance indicates that 50–70 % of the operation is done while viewing the operative field from a monitor. Video assistance is used at first for closed-chest internal mammary artery harvests and congenital heart operations [9–11]. In early 1996, Carpentier performed the first video assisted mitral valve repair through a minithoracotomy using hypothermic ventricular fibrillation [12]. Shortly thereafter, Chitwood performed the first video-assisted mitral valve replacement through a minithoracotomy, using a percutaneous transthoracic aortic clamp and retrograde cardioplegia [13, 14]. Video technology is helpful for replacement and simple repair operations. However, complex reconstructions are still approached under direct vision [14]. 7.3 Level III: Video-Directed and Port Incisions In 1997, Mohr [15] used the AESOP 3000 (Computer Motion, Santa Barbara, CA) voice-activated camera robot in minimally invasive videoscopic mitral valve surgery for the first time. With this device, a voice-controlled robotic arm allows hands-free camera manipulation. Camera motion has been shown to be much smoother, more predictable, and requires less lens cleaning than during manual direction. Image stability during complex surgical maneuvers remains crucial. The addition of three-dimensional visualization, robotic camera control, and instrument tip articulation are the next essential steps toward a totally endoscopic mitral operation where wrist-like instruments and three-dimensional Level IV: Video-Directed and Robotic Instruments Innovations in computer-assisted robotic mitral surgery have rapidly taken place. In June 1998, Carpentier [16] did the first true robotic mitral valve operation using an early prototype of da Vinci Surgical System. The “micro-wrist” permits intra atrial instrument articulation with the seven degrees of freedom offered by the human wrist. The surgeon operates from a master console using three-dimensional vision to affect simultaneous, filtered, and scaled movements in a robotic slave that drives intracardiac articulated instruments. To date, Chitwood et al. [17] have rich experience with robotic mitral valve repairs, and have independently shown that da Vinci is very effective, even for performing complex bileaflet repairs. 7.5 Robotic Mitral Valve Repair Mitral valve repair is favored over replacement in most instances of mitral regurgitation owing to preserved left ventricular function and geometry, a decreased risk of thromboembolism and improved survival [18]. Although classically performed via median sternotomy, isolated mitral valve repair is now frequently performed via minimally invasive access, such as hemisternotomy or right thoracotomy often with videoscopic or robotic assistance [18]. With three-dimensional camera and its magnifying capability, robotic system can provide good exposure for mitral valve repair and replacement in a least invasive approach. Excellent view leads to easy and accurate assessment of valve pathology and a high rate of successful valve repairs or replacement. In 1998, Carpentier [16] performed the first complete robotic mitral valve repair using da Vinci Surgical System. In 2000, Chitwood performed the first complete da Vinci mitral valve repair in North America [19]. And the East Carolina University subsequently participated in the phase I and phase II [17] US Food and Drug Administration (FDA) trials. Now the experience of East Carolina University includes over 540 cases of patients from 2000 to 2010. Since 2007 at the PLA General Hospital in Beijing, Gao and his team have performed over 550 cases of robotic cardiac operations, which include 100 cases of mitral valve surgery using the da Vinci S or Si Surgical System. 7 Robotic Mitral Valve Surgery 95 Fig. 7.1 The patient position 7.5.1 Patient Selection Strict inclusion and exclusion criteria for patient selection should be followed in robotic mitral valve repair. In our experience, all patients had isolated mitral insufficiency or stenosis without other valvular disease or coronary artery disease requiring operative intervention. Patients with previous right thoracotomy were excluded. Patients with severely calcified mitral annulus were not candidates. Decalcification requires further instrument development as well as a reliable means to evacuate any calcium that may fall into the left ventricle. Patients with mitral valve stenosis treatable by commissurotomy would be suitable candidates for robotic repair. Improved visualization of the valve and subvalvular apparatus along with the tiny blade inserted into the robotic instrument would compliment comissurotomy. Patients with poor lung function shall undergo pulmonary testing to ascertain whether they could tolerate single-lung ventilation or not. And the cardiopulmonary bypass (CPB) will be instituted earlier for intrathoracic surgical preparation if the patient has a poor lung function. Fig. 7.2 The positions of ports cavity through the incision made at 2–3 cm lateral to the nipple in the fourth intercostal space (ICS). A 1.5 cm incision is used as a working port in the same ICS for the patient-side surgeon. Additionally two 8-mm port incisions are made in the second and sixth ICS to allow insertion of the right and left instrument arms. The right instrument arm generally is positioned 4–6 cm lateral to the working port in the sixth ICS. The left instrument arm is positioned medial and cephalad to the right arm in the second or third ICS. The fourth arm trocar is placed in the midclavicular line in the fifth ICS (Fig. 7.2). And the surgical system is set-up (Fig. 7.3). Cardiopulmonary bypass is established using femoral arterial inflow and kinetic venous drainage using the femoral vein (21–23 Fr cannula) and right internal jugular vein (15–17 Fr cannula) in each case. The cannulations in right femoral artery, vein (Fig. 7.4) and right internal jugular vein are completed under the guidance of TEE. 7.5.3 7.5.2 Anesthesia, Patient Position and CPB Establishment Patients are anesthetized and positioned, as described for robotic atrial septal defect repair in Chap. 5 with the right chest elevated to 30°–40°. The transesophageal echocardiography (TEE) probe is inserted to evaluate the position of the venous cannulas and surgical results. And the external defibrillator patches are placed to subtend the maximum cardiac mass (Fig. 7.1). After exclusion of the right lung, a 12-mm endoscopic trocar is placed into the right thoracic Surgical Technique The anterior pericardium is opened longitudinally to the phrenic nerve. The incision is extended superiorly to expose the aorta. The vertical pericardium staying sutures are placed on the right side and left superior side of pericardium for exposure, and two right side staying sutures should be as far as possible for nice exposure. The aorta is occluded with Chitwood cross-clamp via the fourth intercostal space in the midaxillary line. Care must be taken to avoid injury to the right pulmonary artery, the left atrial appendage, or the left main coronary artery. We have never used the endoballoon as an occluder since we started with robotic surgery. Antegrade 96 a C. Gao and M. Yang b Atrial retractor port Angiocatheter port Nipple Camera Left arm port Right arm port Chitwood damp Working port Fig. 7.3 The robotic mitral valve repair operative field. (a) System set-up; (b) Sketch map. From Siwek and Reynolds (21Reproduced with permission from Siwek and Reynolds [21) a c b Fig. 7.4 Cannulation of the femoral artery and vein. (a) Making a 2-cm incision in the right groin crease; (b) Exposure of the femoral artery and vein; (c) Placing purse string suture on the vein; (d) Circling the vessels; (e) Arterial cannulas inserted over a guidewire; (f) Vein cannulas inserted over a guidewire; (g) Cannulation completed 7 Robotic Mitral Valve Surgery 97 d e f g Fig. 7.4 (continued) Fig. 7.5 The Chitwood cross-clamp and antegrade cardioplegia administered Fig. 7.6 The small left atriotomy cold blood cardioplegia is administered directly through anterior chest on the second or third intercostal space with 14 F angiocatheter (Fig. 7.5). Carbon dioxide is insufflated continuously into the operative field for deairing. The interatrial groove is dissected. Then a small left atriotomy is performed medial to the right superior pulmonary vein with extension toward the SVC and inferiorly behind the IVC (Fig. 7.6). The atrial septum is retracted with left atrial endowrist retractor (Fig. 7.7) to visualize the mitral valve. The mitral valve and appurtenants are inspected using a 98 C. Gao and M. Yang Fig. 7.7 The left atrial retractor is used to expose the mitral valve Fig. 7.9 Resecting the prolapse P2 segment Fig. 7.8 The mitral valve and appurtenants are inspected using a valve hook Fig. 7.10 Residual leaflet edges are reapproximated valve hook (Fig. 7.8). A left inferior pulmonary vein sump scavenges residual left atrial blood. Valve function is tested by cold saline injections. The table surgeon exchanges the various microtipped instruments. Standard reconstructive methods have been used in all da Vinci mitral valve repairs. Posterior leaflet prolapse is treated by either quadrangular or trapezoidal resection of diseased chordal leaflet segment (Fig. 7.9). Residual leaflet edges are re-approximated with 4-0 GoreTex interrupted sutures or nitinol U-clips (Coalescent Inc., Sunnyvale, CA) (Fig. 7.10). Water injection test is performed again to identify that no mitral valve regurgitation occurs. Remodeling the annulus by ring annuloplasty after mitral valve repair is essential to a complete and long-lasting repair. The size of annulus is measured (Fig. 7.11). The flexible annuloplasty band (Cosgrove Edwards, Edwards Lifesciences, Irvine, CA) is secured between the fibrous trigones using running sutures or nitinol U-clips. Bites should be deep with the needle entering the annulus, then into the left ventricular cavity, and then coming out on the atrial side again. Fig. 7.11 Measuring the annulus For the running suture technique (Fig. 7.12), three 2-0 braided polyester sutures are used to secure the annuloplasty ring as follows [20]: After the ring is introduced into the left atrium, the first suture (16 cm in length) is passed through the ring, through the right trigone, and then back 7 Robotic Mitral Valve Surgery 99 a b c d Fig. 7.12 The running annuloplasty suture technique. (a) First suture is tied at the right trigone and run clockwise. (b) Second suture is tied at the mid-portion of the annulus and the tail is tied to the first suture. through the ring. The suture is then tied down and runs clockwise to the midportion of the ring (Fig. 7.12a). The second suture (14 cm in length) is then passed through the ring, through the midportion of the annulus, and then back through the ring. This second suture is tied down, and the tail is used to secure the first suture (Fig. 7.12b). The second suture then runs clockwise to the left trigone (Fig. 7.12c). The third suture (9 cm in length) is passed through the ring, through the left trigone, and then back through the ring. This third suture is tied down, and the tail is used to secure the second suture (Fig. 7.13d). Another technique is the 2-suture method that we have used. The technique is as follows: The first suture is used as described above. The second suture is passed through the ring, through the left trigone. The suture is then tied down and runs anticlockwise to the midportion of the ring. Then, the two sutures are tied together at the midpoint of the ring (Fig. 7.13). (c) Second suture runs clockwise. (d) Third suture is tied at the left trigone and the tail is tied to the second suture (Reproduced with permission from Tomislav et al. [20]) Fig. 7.13 The ring is secured using the running suture technique The flexible band can be secured using nitinol U-clips (Figs. 7.14 and 7.15). These clips are placed through the annulus like conventional sutures (Fig. 7.14a), with each arm then placed 100 a c C. Gao and M. Yang b d e Fig. 7.14 Annuloplasty band is secured with nitinol U-clips using the da Vinci system. (a) The clips are placed through the annula. (b) The clips are released using robotic needle holders. (c) The U-clip arm is laid over the band. (d) The secured clip against the tissues. (e) The annuloplasty band is secured using U-clip through the band. The locking mechanism, which deploys the clip, is released using robotic needle holders (Fig. 7.14b). Nitinol retains a preformed shape securing the annuloplasty band tightly against the tissues. The U-clip arms are carefully laid over the annuloplasty band to secure it firmly (Fig. 7.14c). The congenital clefts in anterior leaflet of the mitral valve can cause severe mitral valve insufficiency that requires surgical correction. The robotic repair can be easily used for isolated anterior cleft repair. After inspection of the intracardiac anatomy (Fig. 7.16), the cleft in the mitral valve is repaired using multiple interrupted 4-0 GoreTex suture (Fig. 7.17). The mitral valve function is tested by the cold saline injections (Fig. 7.18). In the presence of annular dilation, the repair is buttressed by an annuloplasty. The ring implanted can be completed using the method described above (Fig. 7.19). GoreTex neo-chordae placement is greatly facilitated by a robotic approach due to excellent exposure and 7 Robotic Mitral Valve Surgery 101 Fig. 7.15 Completed repair using nitinol U-clips to secure the annuloplasty band Fig. 7.18 The mitral valve function I is tested by the cold saline injections Fig. 7.16 The cleft is inspected Fig. 7.19 The ring is secured using running sutures Fig. 7.17 The cleft is repaired using multiple interrupted 4-0 GorTex suture magnified view of the subvalvular apparatus. The minimal distortion of the valve provided by the lateral approach enhances the ability to judge and adjust chordae length. Through inspection with mitral valve apparatus, the ruptured chordae is identified (Fig. 7.20). 4-0 GoreTex buttressed with two pledgets are placed through the head of the papillary muscle (Fig. 7.21). Both ends of the suture are then brought through the leading edge of the leaflet (Fig. 7.22). The suture length is then adjusted and the suture is held with a robotic instrument while the patient side surgeon assistant ties the suture (Fig. 7.23). The surgeon firmly holds the suture and let the assistant tie against the robotic instrument to prevent the knot from slipping and making the new chordae too short [21]. 102 C. Gao and M. Yang a b Fig. 7.20 The ruptured chordae of mitral valve. (a) Ruptured chordae in A3 area of anterior leaflet; (b) Ruptured chordae in A2 area of anterior leaflet Fig. 7.21 4-0 GoreTex buttressed with two pledgets are placed through the head of the papillary muscle. (a) Screenshot; (b) Sketch map a The left atriotomy is closed with running sutures after the satisfactory mitral valve plasty using water injection test. Before the crossclamp release, the left atrium is meticulously deaired with antegrade cold blood cardioplegic solution through the angiocatheter, and after removal of the cardioplegia angiocatheter, the cardioplegia site is closed with extracorporeal knot tying through the working port, and then patient is weaned from CPB. The surgical results are confirmed by TEE (Fig. 7.24). and then chest tubes are inserted, and da Vinci was undocked finally. 7.5.4 Postoperative Management Postoperatively patients are monitored as usual at the ICU, and discharged to an intermediate care unit as soon as their b hemodynamics and spontaneous respiration have been adequately stabilized. Chest drains are removed when drainage reaches less than 50 mL/12 h. All patients undergo transthoracic echocardiography immediately before discharge from hospital and at 3 months after the operation. 7.5.5 Surgical Experience and Learning Curves Between January 2007 and May 2013, 70 consecutive patients (49 male and 21 female) underwent mitral valve repair with da Vinci S or da Vinci Si Surgical System at PLA General Hospital. Mean age of the patients was 45.2 years (from 14 to 62 years). All the patients had isolated mitral 7 Robotic Mitral Valve Surgery a 103 b Fig. 7.22 The sutures are brought through the leading edge of the leaflet. (a) Screenshot; (b) Sketch map. From Siwek and Reynolds (Reproduced with permission from Siwek and Reynolds [21]) a b Fig. 7.23 (a) The suture firmly held is tied against the instrument to prevent the knot from slipping and making the new chordae too short. (b) Sketch map. From Siwek and Reynolds (Reproduced with permission from Siwek and Reynolds [21]) a b Fig. 7.24 TEE is used to evaluate the surgical result. (a) Pre-operation, severe mitral valve regurgitation; (b) Post-operative echo C. Gao and M. Yang 104 Table 7.1 Preoperative echocardiographic mitral valve characteristics (n = 90) n 71 37 8 2 14 1 2 2 1 3 14 4 3 2 3 2 Operation time (min) Variables Posterior leaflet P2 prolapse P2 prolapse with ruptured chordae tendineae P2 prolapse and P2 perforation P3 prolapse with ruptured chordae tendineae P3 prolapse and P3 perforation P1 prolapse with ruptured chordae tendineae P1 prolapse with P1 perforation P1 prolapse and P3 perforation P1 and P2 prolapse Anterior leaflet A3 prolapse with ruptured chordae tendineae A3 leaflet cleft A2 leaflet cleft Cleft between A2 and A3 leaflet Cleft between A1 and A2 leaflet 500.00 400.00 300.00 200.00 100.00 0.00 20.00 40.00 60.00 Case number 80.00 100.00 Fig. 7.25 The learning curve of operation time for robotic mitral valve plasty (y(min) = 392.5 − 25.1 ln(x); r2 = 0.167, p = 0.000) 300.00 Table 7.2 Type of mitral valve procedures (n = 90) n 67 3 2 6 4 8 250.00 CPB time (min) Procedures Posterior leaflet resection + annuloplasty ring Posterior leaflet resection Annuloplasty ring Artificial chordae + annuloplasty ring Anterior leaflet repair Anterior leaflet repair + annuloplasty ring 200.00 150.00 100.00 50.00 0.00 20.00 60.00 40.00 Case number 80.00 100.00 Fig. 7.26 The learning curve of CPB time for robotic mitral valve plasty (y(min) = 184.3 − 18.4 ln(x); r2 = 0.184, p = 0.000) 200.00 Aortic ocllusion time (min) valve regurgitation. Patients were excluded if they could not tolerate single-lung ventilation or peripheral CPB, or otherwise were considered as poor candidates for a thoracoscopic approach (Table 7.1). Repair techniques included quadrangular resections, sliding-plasties, neochord insertion, and annuloplasties. See Table 7.2 for the surgical procedures. There were no device-related and procedure-related complications. The median operation time was 296.2 min (ranging from 200 to 490 min), the median CPB time was 130 min (ranging from 70 to 152 min), and the median cross-clamp time was 87.9 min (ranging from 47 to 122 min). Every 5 patients were a group. Then mean operation time, CPB time and cross-clamp time were calculated, and the coefficient of variation of each group was estimated. The learning curves of operation, CPB and cross-clamp time were assessed by means of regression analysis with logarithmic curve fit. The operation time decreased as the case number increased (Figs. 7.25, 7.26, and 7.27). Postoperative echocardiograms showed that 88 patients (97.8 %) had no mitral regurgitation, only two patients (2.2 %) demonstrated trivial mitral regurgitation. The length of hospital stay for all patients was 5–8 days. All the patients were discharged, and the cosmetic results were excellent (Fig. 7.28). 150.00 100.00 50.00 0.00 20.00 60.00 40.00 Case number 80.00 100.00 Fig. 7.27 The linear correlations of cross-clamp time with case number (r2 = 0.064, p = 0.035) 7 Robotic Mitral Valve Surgery 105 b a Fig. 7.28 One year after robotic mitral valve repair, the surgical incision viewed from the front (a) and right side (b) 7.5.6 Summary Virtually any mitral valve pathologic problem can be addressed via an endoscopic robotic approach. The relative contraindications are previous right chest surgery, obesity, and severe mitral annular calcification [21]. Robotic instruments such as the left atrial retractor and simple mitral valve repair techniques including the running annuloplasty suture technique have greatly simplified robotic mitral repair and facilitated complex repairs while resulting in shorter operative time and maintaining excellent results. However, despite enthusiasm for robotic mitral valve plasty, caution cannot be overemphasized because that the final success still needs to be measured through comparison with conventional approach. Surgeons performing totally robotic mitral valve repair should be very experienced in the standard approach and diligent in evaluating the results to ensure the highest quality of valve surgery [22]. Fig. 7.29 The soft retractor in working port can provide more space for delivering the prosthetic valve 7.6.2 7.6 Robotic Mitral Valve Placement 7.6.1 Anesthesia, Patient Position and CPB Establishment The da Vinci Surgical System setup and CPB is established as previously described for robotic mitral valve repair in Chap. 4. The patient will require one-lung ventilation for a significant period of time, necessitating the use of doublelumen tube technique. The use of TEE is indicated for the position of femoral cannulation (Fig. 7.29). The working port incision for a 15-mm soft rubber port or tissue retractor is placed in the fourth ICS. Surgical Technique The camera cannula was placed in the right side, 2–3 cm lateral to the nipple in the fourth ICS. A 2.5- to 3.0-cm incision was used as a working port in the same ICS for the patientside surgeon. The soft tissue retractor was inserted into this port, and no other rib retractor was used (Fig. 7.29). The da Vinci instrument arms were inserted through three 8-mm trocar incisions in the right side of the chest. The right instrument arm was generally poisoned lateral to the working port in the sixth ICS. The left instrument arm was positioned medially and cephalad to the working port in the second ICS. The fourth trocar arm was placed in the midclavicular line in the fifth ICS. All resection and suturing of the mitral valve and atrial closure were completed with the da Vinci S robot. 106 Fig. 7.30 The Chitwood clamp is introduced to avoid injury to the right pulmonary artery, the left atrial appendage, or the left main coronary artery C. Gao and M. Yang Fig. 7.32 The short atriotomy is made with extension toward the SVC and inferiorly behind the IVC LA appendage Aortic valve AV node Circumflex artery Fig. 7.31 The interatrial groove is dissected Fig. 7.33 Inspection of the mitral valve structure with the aid of left atrial retractor Cardiopulmonary bypass was initiated with kinetically assisted bicaval venous drainage. The aorta was occluded with a Chitwood crossclamp (Scanlan International, Minneapolis, MN) using the midaxillary line in the fourth ICS (Fig. 7.30). Antegrade cold blood cardioplegic solution was administered directly through the anterior chest (the second ICS) with a 14 F angiocatheter, by which deairing was conducted, and repeat doses could be given when necessary. TEE was used routinely to monitor the position of the angiocatheter and assist with deairing. Carbon dioxide was insufflated continuously into the operative field for air displacement. The left atrium was then opened parallel to the interatrial septum (Figs. 7.31 and 7.32). All MVRs were performed using standard techniques. The diseased mitral valve was completely excised, and the posterior leaflets were preserved whenever possible (Figs. 7.33 and 7.35). Figure 7.34 shows the proximity of important cardiac structures. Appropriate sizing was performed, and everting, double-armed, mattress sutures with Teflon pledgets were placed counterclockwise from the 11-o’clock position. Every stitch was fixed sequentially outside with a small hemostat. Fig. 7.34 Location of important structures surrounding the mitral annulus (From Cohn [1]) Usually 10–12 sutures were needed (Figs. 7.36 and 7.37). Once the sutures were placed in the prosthesis sewing ring outside the chest, the prosthesis was lowered into the chest and 7 Robotic Mitral Valve Surgery Fig. 7.35 The anterior leaflet is removed with preserving partial posterior leaflet Fig. 7.36 Sutures are then placed anticlockwise from the 11 o’clock point Fig. 7.37 The interrupted sutures with pledget are well placed positioned, and the knots were tied using the knot pusher through the incision (Figs. 7.38, 7.39, 7.40, 7.41, 7.42, and 7.43). The atriotomy was closed with 4-0 polytetrafluoroethylene running suture (W. L. Gore & Associates, Flagstaff, AZ). Before the Chitwood crossclamp was released, meticulous intracardiac de-airing was conducted through the angiocatheter 107 Fig. 7.38 The interrupted sutures are extracorporeally placed in order Fig. 7.39 The patient-side surgeon places the sutures to the mechanical or tissue valve extracorporeally Fig. 7.40 The valve prosthesis is introduced into the left atrium through the working port of cardioplegia, and then the aorta was unclamped. The patient was weaned from cardiopulmonary bypass, and the cardioplegia site was closed with an extracorporeal knot tied through the working port, and chest tubes were inserted. The prosthesis function was confirmed by TEE [23]. 108 C. Gao and M. Yang Fig. 7.41 The patient-side surgeon ties the sutures using knot-pusher Fig. 7.42 The patient-side surgeon ties sutures using Cor-Knot (Lsisolution, Victory-mendon, New York, US) 7.6.3 Surgical Experience and Learning Curves The most common surgical approach to the mitral valve requires the surgeon to saw open the breastbone and spread the edges apart to gain direct access to the heart. Although this approach provides excellent access to the heart, the resulting wound requires several months to heal completely, which causes extended recovery period for patients and substantial activity restrictions, and patients can be subjected to serious complications such as infection, breakdown, and even death [23]. In contrast, robotic cardiac surgery can extend the ability of the surgeon toward new challenges, performing MVR using a 3-cm working port without rib resection and retraction, albeit with the potential danger of performing suboptimal surgery because of learning curves. After more than 500 cases of various types of robotic cardiac surgery, we believe that the da Vinci Surgical system can be considered the best surgical solution to the philosophic approach of minimally invasive cardiac surgery [23]. The 3-D digital vision system enables natural depth perception with high-power magnification [18]. A perfect view was obtained of all cardiac chambers, the mitral valve, and the subvalvular apparatus, especially in patients with a small left atrium. Although many reports have described the excellent results of robotically assisted mitral valve repair using the da Vinci Surgical system, few data are available on robotically assisted MVR. All our patients had satisfactory clinical outcomes, as demonstrated by the complete echocardiographic follow-up. No late thromboembolic complications or paravalvular leaks developed. Intraoperative contamination must be considered when performing extrathoracic knots and introducing the prosthetic ring through the narrow working port, although no cases of either native or prosthetic mitral valve endocarditis were identified during follow-up in our patients [23]. The suture techniques for robotic MVR are very different from those in the open technique. For all mechanical and bioprosthetic valves, we used everting, double-armed mattress sutures with Teflon pledgets counterclockwise from the 11-o’clock position to prevent any possibility of subannular obstruction of the valve leaflets by protruding tissue and to prevent one suture from crossing with another. Every stitch was fixed sequentially outside with a small hemostat (Figs. 7.37 and 7.38) [23]. Usually 10–12 sutures were needed (Fig. 7.43). Once the sutures were placed sequentially in the prosthesis sewing ring outside the chest, the prosthesis was lowered into the chest and positioned, and the knots were tied with the knot pusher through the incision. When the knots are tied with the knot pusher, the console surgeon must confirm the knot tightness one by one. And in the case of a knot not being tight, the knot tightness requires robotic assistance. Recently, we started using the Cor-Knot (LSI Solution, Victor, NY) to tie the knots during robotic MVR (Fig. 7.42). This has resulted in a shorter operative time, and the preliminary results have been satisfactory [23]. It is believed that any new surgical approach requires a learning curve, and robotic cardiac surgery is no exception. We believe that robotic cardiac surgery requires real teamwork and surgeons must overcome a substantial learning curve. Our learning curve is showed graphically in Figs. 7.44 and 7.45. The mean crossclamp time was significantly shortened with surgical experience as denoted by the number of operations. Our learning curve was truncated because the console surgeon simultaneously had performed a large volume of various types of other robotic cardiac surgeries with the same team over a relatively short period [23]. Furthermore, since we started our robotic surgical program, our robotic team members have remained the same. Our experience has demonstrated that with a well-trained 7 109 Robotic Mitral Valve Surgery a b Fig. 7.43 The mitral valve replacement is completed. (a) The mechanical valve; (b) The tissue valve 200.00 CPB time (min) 175.00 150.00 125.00 100.00 0.00 10.00 20.00 Case number 30.00 40.00 Fig. 7.44 The learning curve of CPB time for robotic mitral valve replacement (y(min) = 172.1 − 18.9 ln(x); r2 = 0.539, p = 0.000) 160.00 Aortic occlusion time (min) robotic team and after a substantial learning curve, optimal results can be achieved with robotic surgery [5–9, 23]. In conclusion, the present results suggest that robotically assisted MVR is safe for patients with isolated mitral valve stenosis. The 3-D digital vision system provides a perfect view of the mitral valve and the subvalvular apparatus in patients in whom limited exposure prohibits direct vision. This technique also provides the unique opportunity for junior surgeons to observe experienced surgeons at work, shorten their learning curve and avoid mistakes [23]. We conducted a retrospective review on 40 patients who underwent totally robotic mitral replacement with the da Vinci S or Si robotic system from November 2008 to May 2013. Mean age of the patients was 47 ± 10 years (from 32 to 66 years old). Eighteen patients were female and 22 were male. All patients had isolated mitral valve disease. Preoperative echo showed mitral stenosis combined with regurgitation in 11 patients and mitral stenosis in 29 patients. All patients had a preserved left ventricular ejection fraction. Moderate annular calcification alone did not preclude patients from undergoing a robotically approach. The mitral procedure was completed endoscopically in all the patients, including 30 mechanical prosthetic valves and ten tissue valve replacements. These procedures did not mandate intraoperative conversion to alternate techniques and caused no surgery-related hospital deaths. The median operation time was 320 min (from 140 to 405 min), the median CPB time was 127.5 min (from 89 to 198 min), and the median cross-clamp time was 87.9 min (from 47 to 151 min). The learning curves of operation, CPB and cross-clamp time were assessed by means of regression analysis with logarithmic curve fit. The CPB and cross-clamp time decreased as the case number increases (Figs. 7.44 and 7.45). 140.00 120.00 100.00 80.00 60.00 0.00 10.00 20.00 30.00 Case number 40.00 Fig. 7.45 The learning curve of cross-clamp time for robotic mitral valve replacement (y(min) = 132.2 − 17.4 ln(x); r2 = 0.717, p = 0.000) 110 7.6.4 C. Gao and M. Yang Summary Robotic technology can be used in mitral valve replacement safely and effectively. The robotic system allows excellent visualization of the valve and permits dexterity [23]. The placement of wrist-like articulations at the end of the instrument moves the pivoting action to the plane of mitral annulus. This improves dexterity in tight spaces and allows ambidextrous suture placement. From the learning curve, we can see that operation time decreases as case number increases. No doubt this change is related to improved setup and deployment times, team cooperation, and surgeon experience. This new science is a trek not a destination. In this era of outcomes-based medicines, surgical scientists must continue to evaluate robotics and all new technologies critically. Despite enthusiasm, caution can never be overemphasized. Surgeons must be careful because indices of operative safety, speed or recovery, level of discomfort, procedure cost, and long-term operative quality have yet to be defined. Conventional valve operations still enjoy long-term success with ever-decreasing morbidity and mortality, and remain the excellent control group for robotic mitral valve surgery. References 1. Cohn L. Cardiac surgery in the adult. 3rd ed. New York: McGrawHill Professional; 2008. 2. Gundry SR, Shattuck OH, Razzouk AJ, et al. Facile minimally invasive cardiac surgery via ministernotomy. Ann Thorac Surg. 1998;5:1100–4. 3. Grove DM, Sabik JF, Navia J. Minimally invasive valve surgery. Ann Thorac Surg. 1998;65:1535–8. 4. Arom KV, Emery RW. Minimally invasive mitral operations. Ann Thorac Surg. 1997;63:1219–20. 5. Navia JL, Cosgrove DM. Minimally invasive mitral valve operations. Ann Thorac Surg. 1996;62:1542–4. 6. Stevens JH, Burdon TA, Peters WS, et al. Port-access coronary artery bypass grafting: a proposed surgical method. J Thorac Cardiovasc Surg. 1996;111:567–73. 7. Pompili MF, Stevens JH, Burdon TA, et al. Port-access mitral valve replacement in dogs. J Thorac Cardiovasc Surg. 1996;112: 1268–74. 8. Cosgrove DM, Sabik JF, Navia J. Minimally invasive valve surgery. Ann Thorac Surg. 1998;65:1535–8. 9. Acuff TE, Landrenau RJ, Griffith BP, et al. Minimally invasive coronary artery bypass grafting. Ann Thorac Surg. 1996;61: 135–7. 10. Nataf P, Lima L, Regan M, et al. Minimally invasive coronary surgery with thoracoscopic internal mammary dissection: surgical technique. J Card Surg. 1996;11:288–92. 11. Burke RP, Wernovsky G, van der Velde M, et al. Videoassisted thoracoscopic surgery for congenital heart disease. J Thorac Cardiovasc Surg. 1995;109:499–507. 12. Carpentier A, Loulmet D, Carpentier A, et al. Open heart operation under videosurgery and minithoracotomy: first case (mitral valvuloplasty) operated with success. C R Acad Sci III. 1996;319:219. 13. Chitwood WR, Elbeery JR, Chapman WHH, et al. Videoassisted minimally invasive mitral valve surgery: the “micro-mitral” operation. J Thorac Cardiovasc Surg. 1997;113:413–4. 14. Chitwood WR, Elbeery JR, Moran JM. Minimally invasive mitral valve repair: using a mini-thoracotomy and transthoracic aortic occlusion. Ann Thorac Surg. 1997;63:1477–9. 15. Falk V, Walter T, Autschbach R, et al. Robot-assisted minimally invasive solo mitral valve operation. J Thorac Cardiovasc Surg. 1998;115:470–1. 16. Carpentier A, Loulmet D, Aupecle B, et al. Computer assisted open-heart surgery. First case operated on with success. C R Acad Sci III. 1998;321:437–42. 17. Nifong LW, Chitwood WR, Pappas PS, et al. Robotic mitral valve surgery: a United States multicenter trial. J Thorac Cardiovasc Surg. 2005;129:1395. 18. Anderson CA, Chitwood WR. Advances in mitral valve repair. Future Cardiol. 2009;5(5):511–6. 19. Chitwood WR, Nifong L, Elbeery JR, et al. Robotic mitral valve repair: trapezoidal resection and prosthetic annuloplasty with da Vinci surgical system. J Thorac Cardiovasc Surg. 2000;120: 1171–2. 20. Tomislav M, Craig MJ, Gillinov M, et al. A novel running annuloplasty suture technique for robotically assisted mitral valve repair. J Thorac Cardiovasc Surg. 2010;139:1343–4. 21. Siwek LG, Reynolds B. Totally robotic mitral valve repair. Oper Tech Thorac Cardiovasc Surg. 2007;12:235–49. 22. Jan DS, Suyong AM, Chon L. Minimally-invasive valve surgery. J Am Coll Cardiol. 2010;56(6):454–62. 23. Gao C, Yang M, Wang G, et al. Robotically assisted mitral valve replacement. J Thorac Cardiovasc Surg. 2012;143(4 Suppl):S64–7. 8 Robotic Coronary Bypass Graft on Beating Heart Changqing Gao and Ming Yang Abstract The ultimate goal of minimally invasive CABG is to perform the entire anastomosis in a closed chest, to avoid the deleterious effect of CPB and to minimize the incision and surgical trauma. We think that totally endoscopic coronary artery bypass (TECAB) on beating heart has brought minimally invasive CABG close to this goal. Since the first report of totally endoscopic CABG using da Vinci Surgical System (Intuitive Surgical, Sunnyvale, CA, USA) in 1999, the robotic technology has been applied to the closed-chest CABG on arrested or beating heart for more than 10 years. Despite this successful milestone, only a limited number of TECAB operations have been carried out worldwide. We started to perform the robotic CABG on beating heart using da Vinci Surgical System in 2008. In this chapter, we will describe in detail our experience in minimally invasive direct coronary artery bypass (MIDCAB) on beating heart through minithoracotomy, totally endoscopic coronary artery bypass (TECAB) on beating heart, and the hybrid revascularization. 8.1 Robotic Internal Thoracic Arteries Harvesting The ultimate goal of minimally invasive coronary artery bypass graft (CABG) is to perform the entire anastomosis in a closed chest, to avoid the deleterious effects of cardiopulmonary bypass (CPB) and to minimize the incision and surgical trauma. The superiority of left internal thoracic artery (LITA) as a conduit has been well established for long-term patency and event-free survival. Remarkable development has been made in the robotic surgical technology to reduce surgical trauma and to improve the postoperative course. Loulmet [1] reported the first totally robotic coronary artery bypass grafting on arrested heart in 1999. C. Gao, MD (*) • M. Yang, MD Department of Cardiovascular Surgery, PLA General Hospital, No. 28 Fuxing Road, Beijing 100853, People’s Republic of China e-mail: gaochq301@yahoo.com The initial clinical step for programs wishing to develop a robotic coronary surgery program is internal thoracic artery (ITA) takedown. Both pedicle and skeletonized harvesting techniques can be applied, with the latter offering better graft length and easier graft handling. The advantages of ITA skeletonization are reported to include early high blood flow, a longer conduit, and less bleeding than pedicle ITA grafts [2]. Longer conduits are needed for complete endoscopic arterial revascularization. The feasibility and safety of ITA skeletonizing using da Vinci robotic system have been reported [3, 4]. 8.1.1 Anesthesia and Patient Position The patient is positioned supine on the left edge of the operating room (Fig. 8.1). After routine induction of anesthesia, double-lumen intubation is carried out for single right lung ventilation. The placement of the double lumen endotracheal tube is aided by bronchoscopy. Single lung ventilation is an important step of operation for adequate visualization during the mobilization of ITAs. C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_8, © Springer Science+Business Media Dordrecht 2014 111 112 Fig. 8.1 Patient positioned on left edge of OR table C. Gao and M. Yang Fig. 8.3 Ports placement for LITA harvesting 8.1.2 Fig. 8.2 The external defibrillator pads on chest Standard hemodynamic monitoring is used with a radial arterial line for systemic blood pressure monitoring. A central venous line or a pulmonary artery catheter can be used for central access of the cardiac monitoring. CO2 insufflation at a pressure of 8–10 mmHg is used in the left pleural space to help with exposure. Special consideration has to be given to hemodynamic effects related to the insufflation as the increased pressure of CO2 may cause tamponade physiology and affect hemodynamics. Single lung ventilation can also cause hypoxemia and hypercarbia which hence may make the patient unstable. External defibrillator patches are placed on the chest (Fig. 8.2) and the patient is positioned supine with the left chest elevated to 30° with the aid of a small bolster under the left chest. The operative side arm with protective padding is hung loosely and supported by a sheet. In the female patient, the breast is positioned medially after sterile skin preparation, and is secured by an adhesive sheet during the draping. Surgical Technique The port sites are marked on the patients skin (Fig. 8.3) before the incision is made. The camera port mark is on a transverse line midway between the suprasternal notch and the xiphoid process. The elevation of the camera port is located about 3 cm lateral of the midclavicular line (MCL), any place from 4 to 6 cm medial of the anterior axillary line (AAL) depending on the body habitus. This location is typically at the 4th or 5th ICS but depends on the body habitus and the length of the sternum. The location of the left instrument port is about the breadth of four fingers from the camera mark at about the same elevation, and always in the seventh ICS. The right instrument port is about the breadth of four fingers from the camera port at about the same elevation, and always in the third ICS. The three ports are in the almost same line. However, our experience is that left port should be little lower in order to prevent collisions. After deflation of the left lung, a camera port is inserted through the middle incision and carbon dioxide insufflation is initialed and maintained at an average of 6–8 mmHg, which may be increased to 12 mmHg as long as patients are able to maintain satisfactory hemodynamic status. A 30 degree-angle upward camera is inserted, and the thoracic cavity, the location and course of the LITA are examined. The left and the right instrument ports are inserted (Fig. 8.4). The surgical cart with 4 arms is brought in and docked to the camera and the instrument arm ports (Fig. 8.5). After access to the left pleura space, a 30° upward endoscope is inserted to the camera port by the patient-side surgeon. The entire mediastinum is inspected. CO2 is insufflated for adequate visualization and working space for hemodynamic tolerance. The required dose of CO2 is nominally 8 mmHg (usually 8–10, 12–15 mmHg maximum for fatty 8 Robotic Coronary Bypass Graft on Beating Heart 113 Fig. 8.4 Ports placement for LITA harvesting Fig. 8.6 Dissecting the pleura parietalis, fascia and muscles covering the LITA Fig. 8.5 The da Vinci S Surgical System set up mediastinum). LITA location and adhesions are carefully examined before surgery. The LITA is identified and pulsation can be observed. Both pedicle and skeletonized harvesting techniques can be applied. The skeletonized harvesting technique is similar to that used in open surgery or endoscopy. First, the pleura parietalis, fascia and muscles covering the LITA are transected along the entire length (Fig. 8.6). This allows exposure of the vessel regardless of the amount of fat or muscle covering the mammary artery. The skeletonized LITA is dissected from the lateral edge medially using blunt dissection and short bursts of low power monopolar cautery to mobilize the anterior attachments (Fig. 8.7). Small intercostal branches are ligated with monopolar energy in a painting stroke then transected (Fig. 8.8). Large intercostal branches are clipped for hemostasis (Fig. 8.9). The entire length of LITA is dissected from the first intercostal branch to the diaphragm. Starting at about the 3rd ICS, short Fig. 8.7 The skeletonized LITA harvesting is performed using low power cautery segments of periarterial connective tissue are left attached to help stabilize the ITA when the surgeon prepares the end for anastomosis. The right ITA (RITA) can be harvested through the same approach for the LITA harvesting. After the instruments are inserted into the robotic ports, the anterior mediastinum is dissected and the instruments gain accesses to the right pleural space (Fig. 8.10). The RITA is identified. The pedicle or skeletonized harvesting technique is similar to that used in robotic LITA harvesting (Figs. 8.11, 8.12, 8.13, and 8.14). For RIMA to be the right coronary bypass graft, the RITA can also be robotically harvested using right chest approach, just the opposite to the left chest approach (Figs. 8.15 and 8.16). 114 C. Gao and M. Yang Fig. 8.8 The small branch is ligated with monopolar energy Fig. 8.11 Opening the right pleural cavity for exposing the RITA Fig. 8.9 Large intercostal branches are clipped for hemostasis Fig. 8.12 RITA is identified Fig. 8.10 The anterior mediastinum is dissected Fig. 8.13 RITA is harvested in skeletonized fashion 8 115 Robotic Coronary Bypass Graft on Beating Heart 70.00 Harvesting time (min) 60.00 50.00 40.00 30.00 20.00 10.00 0.00 50.00 100.00 150.00 200.00 Case number Fig. 8.14 The double ITAs are harvested Fig. 8.17 The learning curve of ITAs harvest (y(min) = 57.8 − 5.5 ln(x); r2 = 0.342, p = 0.000) 8.1.3 Fig. 8.15 The surgical system set-up of right approach for RITA harvesting Fig. 8.16 RITA is robotically harvested in a right approach The Surgical Experience and Learning Curves There is an initial learning curve with the technique of robotic-assisted endoscopic ITAs harvest. From April 2007 to May 2013, 220 patients accepted totally robotic coronary bypass on beating heart (BH-TECAB, 100 cases) or robotic minimally invasive coronary bypass on beating heart (MIDCAB, 120 cases). The mean age was 58.9 ± 10.1 (33–78) years. ITA was harvested robotically in all cases successfully without damage leading to abandon, including LITAs, RITAs and double-ITAs harvesting with da Vinci S or Si system. The mean harvesting time was 30.8 ± 8.7 (16–52) min. A significant learning curve (Fig. 8.17) for harvesting time was noted: y(min) = 57.8 − 5.5 ln(x); (r2 = 0.342; P < 0.01) The development of robotic surgical devices is a prerequisite for performing TECAB. However, TECAB is a highly complex procedure consisting of several but not routinely performed surgical steps, which requires a modular and step approach [5]. An important step of this procedure is the robotic ITA harvesting. For the patients undergoing robotic harvesting, the preoperative three-dimensional computer tomography images are needed to be taken to evaluate the quality of the target ITA. The robotic-enhanced IMA takedown is a prerequisite for TECAB or MIDCAB operations and can be safely implemented. With a noted learning curve, the surgeon will harvest the target ITA in an acceptably shorter time. In this study the harvesting time stayed stable after about 30 cases and decreased as case number increased. The harvesting time was reduced to an acceptable duration between 25 and 30 min. Long preparation time at the beginning may be explained by the complexity of this new system and the lack of clinical experience of the operation team [6]. 116 C. Gao and M. Yang Bolotin and associates [7] reported robotic LITA harvesting speed in a range of 39–48 min when using the dog model. Learning curves and long preparation time at the beginning of implementation had also been described by Falk and associates [8] and Reuthebuch and coworkers [9]. The Falk group presented a LITA takedown time of about 40 min after 50 cases. The Reuthebuch study noted that after the learning curve, a target LITA harvesting speed in the 35 min range could be achieved. In conclusion, robotic-enhanced IMA takedown can be safely implemented, and is prerequisite for TECAB operations. After overcoming learning curve, IMA takedown can be performed in an acceptable time. Demographics and chest size do not seem to influence ITA harvesting time. The rate of LITA injuries is comparable with the rate reported for conventional thoracoscopic harvesting [6]. 8.2 pericardium. The small left anterior thoracotomy incision (about 4 cm) may be made in the fourth or fifth intercostal space (Fig. 8.21). And the left pleural cavity is entered and a retractor is placed in the incision (Fig. 8.22). The distal end of the artery is then prepared for anastomosis. LAD is Minimally Invasive Direct Coronary Artery Bypass Grafting (MIDCAB) After LITA is completely mobilized, the pericardium is incised robotically, anterior to the left phrenic nerve and the small pericardial branches are carefully cauterized (Fig. 8.18). This helps in clearing the operative field and also proper placing of ITA. Then the left anterior descending artery (LAD) or the target vessels are identified (Fig. 8.19) and the corresponding anterior intercostal space is identified to confirm the proper placement of the small left anterior thoracotomy incision, usually 4 cm long in the 4th ICS. After systemic heparinization, with an activated clotting time (ACT) goal of 350 s, the LITA is dissected distally. The distal end of the artery is parked on the pericardium using a hemoclip (Fig. 8.20). If RITA is to be used for anastomosis, it is harvested prior to LITA harvest. RITA is harvested in its full length as a skeletonized conduit as described above in Fig. 8.16. If a free RITA is to be used for composite grafting, it is dissected at its origin, and the free RITA is parked on the Fig. 8.19 Identifying the target vessel Fig. 8.20 ITA is parked on the pericardium using a hemoclip Fig. 8.18 The pericardium is opened Fig. 8.21 A small left anterior thoracotomy incision may be made in the fourth or fifth intercostal space 8 Robotic Coronary Bypass Graft on Beating Heart 117 Fig. 8.22 The retractor and cardiac stabilizer are used to expose the target vessel Fig. 8.24 LITA is anastomosed to the LAD Fig. 8.23 LITA is anastomosed to the LAD in the end to side fashion, using a continuous 7-0 Prolene suture stabilized with a cardiac stabilizer and LITA is anastomosed to LAD manually in the end to side fashion, using a continuous 7-0 Prolene suture (Fig. 8.23). The in situ LITA is always used as grafting to the LAD (Fig. 8.24), or sequentially to diagonal branch (Fig. 8.25). The LAD along with composite RITA can be used to the lateral wall grafts. In some instances, in situ RITA can be anastomosed to the LAD, and in situ LITA to the lateral wall vessels. All composite grafts are anastomosed prior to the coronary grafting. 8.2.1 Surgical Experience and Learning Curves One hundred and twenty (86 male and 34 female) patients of the study group underwent MIDCAB. The mean age was 58.9 years (38–77 years), the mean weight was 70.6 kg Fig. 8.25 LITA is sequentially anastomosed to LAD and diagonal branch (44–100 kg). The mean height was 165.9 cm (153–178 cm). The mean left ventricular ejection fraction was 63.7 % (44–72 %) and the mean diameter of left ventricle was 44.8 mm (35–57 mm). The mean operating-room time was 240.8 min (180–300 min) and the mean operating time was 182.9 min (160–200 min). The mean ITA harvesting time was 33.4 min (16–45 min) (Fig. 8.26). Double ITA harvesting (for “Y” type or sequence graft) was performed in three patients (Fig. 8.27). Right ITA harvesting was performed on five patients (Poor LITA quality was found in one patient. RITA to right coronary graft was performed on two patients and RITA to LAD graft on two patients.). RITA to RCA graft was performed on two patients (Fig. 8.28), LITA to diagonal branch graft on two patients, (Fig. 8.29), RITA to LAD graft on one patient (Fig. 8.30), sequential graft on four patients (Fig. 8.31), RITA to LAD and 118 C. Gao and M. Yang Fig. 8.26 The MIDCAB incision after operation Fig. 8.28 RITA is anastomosed to the RCA Fig. 8.27 “Y” type graft for LAD and diagonal branch using composite graft Fig. 8.29 LITA to diagonal branch graft LITA to diagonal branch graft on two patients, (Fig. 8.32). LITA to LAD graft was performed on the rest of the patients (Fig. 8.33). The mean graft flow was 21.3 ± 12.6 (15–56) ml/min. The graft patency was followed up by 64-MSCTA, and the patency rate was 97.1 %. The mean follow-up time was 13.1 (1–70) months. All patients had excellent cosmetic results (Figs. 8.34 and 8.35). 8.3 Totally Endoscopic Coronary Artery Bypass Grafting (TECAB) Conventional coronary artery bypass grafting provides complete revascularization with excellent long-term results for various clear-cut indications with a major favorable impact on the patient outcome and recurrence of adverse cardiac events. The success of catheter-based techniques for treating 8 Robotic Coronary Bypass Graft on Beating Heart 119 Fig. 8.30 RITA is anastomosed to the LAD Fig. 8.32 LITA is anastomosed to diagonal branch and the RITA to LAD ischemic coronary syndromes, combined with the shift toward less invasive approaches, has renewed interest in minimally invasive approach. The current tendency is to perform operations through smaller and smaller incisions to reduce hospital stay and to hasten postoperative recovery. After the introduction of robotic telemanipulators, TECAB became feasible in the late 1990s. Didier Loulmet [1] performed the first TECAB procedure on arrested heart in 1999, and subsequently several investigators reported TECAB on beating heart [10, 11]. However, only a limited number of cases have been performed worldwide. 8.3.1 Fig. 8.31 LITA is used in sequential graft Surgical Technique TECAB surgery on beating heart begins with satisfactory single lung ventilation of the patient, and patient positioning 120 C. Gao and M. Yang Fig. 8.35 Three months after the surgery with well-healed incisions Fig. 8.33 LITA is anastomosed to LAD Fig. 8.36 The patient in a supine position with the left chest elevated 30° Fig. 8.34 A MIDCAB patient, 1 month after the surgery on the operating room table allows adequate access to the anatomy. After routine induction of anesthesia, doublelumen intubation is carried out for single right lung ventilation. External defibrillator patches are placed on the chest, and the patient is positioned supine with the left chest elevated 30° with the aid of a small bolster under the left chest (Fig. 8.36). The operative side arm with protective padding hung loosely is supported by a sheet. In female patients, the breast is positioned medially, and after sterile skin preparation, is secured by an adhesive sheet during the draping. Three 0.8–1.0-cm incisions are made in the 3rd, 5th, and 7th intercostal spaces (ICS) 2–3 cm medial to the anterior axillary line (Fig. 8.37). After deflation of the left lung, a camera port is inserted through the middle incision and Fig. 8.37 The ports placement for LITA harvesting before TEACB carbon dioxide insufflation is initiated and maintained at an average of 6–8 mmHg, which may increase to 12 mmHg as long as patients are able to maintain satisfactory hemodynamic status. A 30° angle upward camera is inserted, and the thoracic cavity and the location and course of the LITA are examined. The left and the right instrument ports are inserted. 8 Robotic Coronary Bypass Graft on Beating Heart 121 Fig. 8.38 The system set-up Fig. 8.40 LITA is fully harvested in a skeletonized fashion Fig. 8.39 The patient side cart center column is aligned with the patient’s neck Fig. 8.41 Large intercostal branches are clipped using hemoclip The surgical cart with 4 arms is brought in and docked to the camera and the instrument arm ports (Figs. 8.38 and 8.39). The robotic system is used to harvest the LITA completely from the subclavian vein to the LITA bifurcation in a totally skeletonized fashion (Fig. 8.40). Hemoclips are used for larger branches, while cautery is used to cauterize and transect the smaller branches. The 1st and 2nd intercostal arterial branches are usually larger, therefore, Hemoclips are used (Fig. 8.41). In a few cases, LITA is harvested with the accompanying veins in case of close proximity of arteries and veins. The LITA is left attached to the chest wall with the connecting areolar tissue to prevent it from hanging over the pericardium. The pericardial fat is removed (Fig. 8.42) and pericardiotomy is performed (Fig. 8.43). The pericardium over the apex of the left ventricle is left intact to prevent herniation of the heart, and the target vessel is identified using a 30 degree-angle-downward camera (Fig. 8.44). Fig. 8.42 The pericardial fat is removed 122 C. Gao and M. Yang Fig. 8.43 The pericardiotomy is performed Fig. 8.45 The 12 mm cannula is docked to the system Fig. 8.44 The target vessel is identified Fig. 8.46 Adjunctive mediastinotomy 12 mm cannula at the subcostal level The da Vinci S 12 mm cannula for endostabilizer is inserted into the thoracic cavity close to the left midclavicular line at the subcostal margin (Figs. 8.45 and 8.46). The skeletonized LITA is sprayed using papaverine solution with a 5 Fr feeding tube (Fig. 8.47). All the anastomosis supplies are passed into the chest through this port (Fig. 8.48). After systemic heparinization, the distal LITA is skeletonized completely and partially transected obliquely leaving a small toe section attached (Fig. 8.49). 5 S18-U-Clips are put outside-in in the far side of the partial transection of the LITA (Fig. 8.50). The LITA is fully transected and secured to the epicardial fat to maintain the LITA location and orientation. After the console surgeon takes active control to position the endostabilizer at the LAD to apply epicardial tension (Fig. 8.51), the LAD is dissected (Fig. 8.52) and occluded proximally and distally with SaddleLoops (Fig. 8.53 and 8.54). LAD arteriotomy is created (Fig. 8.55) and anastomosed to LITA using an interrupted parachuting technique (Fig. 8.56). First, the 5 Fig. 8.47 The skeletonized LITA is sprayed using papaverine solution with a 5Fr feeding tube 8 Robotic Coronary Bypass Graft on Beating Heart 123 Fig. 8.48 All the anastomosis supplies are passed into the chest through this port Fig. 8.50 Five S18-U-Clips are put outside-in in the far side of the partial transection of the LITA Fig. 8.49 After systemic heparinization, the distal LITA is partially transected obliquely leaving a small toe section attached Fig. 8.51 EndoWrist stabilizer and ClearField irrigator positioned onto target site U-clips are put inside-out in the far side of LAD (Fig. 8.57), and then three more U-clips are put in the near side (Fig. 8.58), and ITA is parachuted onto coronary artery. The SaddleLoop occluders are removed to check the anastomosis (Fig. 8.59). Lidocaine is infused intravenously during pericardiotomy and coronary anastomosis to minimize ventricular arrhythmia. After protamine is administered, the graft flow is measured by the Medistim transit time probe (Fig. 8.60). All the accessories are removed from the ports, a chest tube is placed, the robotic system is removed and all incisions are closed (Fig. 8.61). RITA can be anastomosed to the main stem of the right coronary artery using the same technique. RITA can also be robotically harvested using right chest approach, just the opposite of the left chest approach. And the anastomosis can be completed in the same fashion as that of LITA to LAD (Figs. 8.62, 8.63, and 8.64). Fig. 8.52 LAD is dissected 124 Fig. 8.53 The distally LAD is occluded with SaddleLoops Fig. 8.54 LAD is totally occluded proximally and distally with SaddleLoops C. Gao and M. Yang Fig. 8.56 LITA is anastomosed to LAD using an interrupted parachuting technique Fig. 8.57 5 U-clips are put inside-out in the far side of LAD Fig. 8.55 LAD arteriotomy is created Fig. 8.58 Three more U-clips are put in the near side of LAD 8 Robotic Coronary Bypass Graft on Beating Heart Fig. 8.59 SaddleLoop occluders are removed to check the anastomosis 125 Fig. 8.62 RITA is harvested in skeletonized and prepared for anastomosed to RCA Fig. 8.63 TECAB procedure of RITA to RCA Fig. 8.60 Graft flow is measured by the Medistim transit time probe Fig. 8.61 The operative incisions after TECAB Fig. 8.64 RITA is anastomosed to RCA C. Gao and M. Yang 60.00 25 50.00 20 Anastomosis time (min) ITA harvesting time (min) 126 40.00 30.00 20.00 10 5 10.00 0 0 20 40 60 Case number 80 100 0 20 40 60 80 100 Case number Fig. 8.65 The learning curve of ITA harvest in TECAB procedure (y(min) = 50.1 − 4.5 ln(x); r2 = 0.185, p = 0.000) Fig. 8.67 The learning curve of anastomosis time (y(min) = 18.3 − 2.5 ln(x); r2 = 0.285, p = 0.000) 50.00 150 40.00 400 Operation time (min) Occlusion time (min) 15 30.00 20.00 350 300 250 10.00 200 0.00 0 20 40 60 80 100 Case number Fig. 8.66 The learning curve of coronary (y(min) = 38.2 − 5.5 ln(x); r2 = 0.366, p = 0.000) 8.3.2 150 0 20 40 60 80 100 Case number occlusion time Surgical Experience and Learning Curves One hundred TECAB procedures on beating heart were successfully completed at the PLA General Hospital. Two patients were converted to minithoracotomy during the operation after the target vessels were identified to be not ideal for TECAB. The average LITA harvesting time, coronary occlusion time and anastomosis time were 34.9 ± 9.6 (18–55) min, 19.5 ± 8.4 (7–41) min and 10.0 ± 4.2 (5–21) min respectively. The mean operation time was 150.1 ± 55.9 (120–188) min. The learning curves Fig. 8.68 The learning curve of operation time (y(min) = 400.9 − 49.9 ln(x); r2 = 0.663, p = 0.000) were shown graphically in Figs. 8.65, 8.66, 8.67, and 8.68. The average graft flow was 35.8 ± 18.2 (10–103) ml/min. The average chest drainage was 164.9 ± 83.2 (70–450) ml. Troponin-T and creatine kinase/creatine kinase-myoglobin (CK/CK-MB) levels were within normal range. No patient had angina after surgery. TECAB on beating heart has become a feasible procedure for coronary revascularization at specialized centers. However, proper planning and patient selection are paramount for success. Grafting strategy should never be compromised to complete revascularization. This was the first robotic endoscopic cardiac procedure reported and remains 8 127 Robotic Coronary Bypass Graft on Beating Heart a b Fig. 8.69 Coronary angiography shows the sever stenosis in the proximal segment of LAD (a) and the LITA graft (b) among the most complex robotic surgical operations. TECAB has been criticized especially because of prolonged operative times compared with open procedures. We have to state that since the heart is not decompressed by using CPB, space in the thoracic cavity is limited, Therefore, CO2 pressure may be increased above the suggested value as long as the heart is filled sufficiently and contractility is not impaired; suturing of the anastomosis is the most demanding part of TECAB on beating heart, even the slightest movement of the target vessel impairs surgical manipulation due to the 10× magnification. TECAB on beating heart is a safe procedure in selected patients, and produces excellent early and midterm patency of anastomosis and surgical results. TECAB on beating heart should be conducted by surgeons with extensive surgical experience in open techniques, and requires a stable and well trained robotic team, and learning curves are substantial. Since da Vinci is a surgical tool, what kinds of surgical procedures surgeons can perform depend on surgeons’ own experience in the operating room, not on da Vinci! In our study, we experienced significant learning curves in terms of durations of operation, coronary occlusion, and anastomosis. It is clear that intraoperative surgical challenges prolong the operative time. It therefore seems to be very important for the surgical team to make all efforts to avoid any surgical problems and pay very meticulous attention to every detail. Before discharge, eight patients of the study group underwent CTA scan and the rest of the patients underwent coronary angiography. Both angiography and CTA scan showed 100 % graft patency (Figs. 8.69 and 8.70). Unexpectedly, the angiography showed that LITA graft in the middle segment developed a collateral branch in two patients (Fig. 8.71), however, they were asymptomatic. After discharge, all patients were followed up by CTA scan in 3, 6 and 12 months and the study showed 100 % graft patency. One patient had gastric bleeding 6 months after surgery. The average follow-up time was 18.39 ± 11.8 (1–62 months). ICU stay was 1.5 ± 0.9 (1–3) days. No other complications were found. And all the patients had cosmetic results (Fig. 8.72, 8.73, and 8.74). 8.4 Hybrid Coronary Revascularization Despite decades of intense scientific clinical research, controversy still exists regarding the most appropriate therapy for patients with multivessel coronary artery disease (CAD). Prospective randomized studies from each of the last 3 decades have documented the superior long-term symptom relief and survival benefit that coronary artery bypass grafting affords compared with both medical therapy and percutaneous coronary interventions (PCI) for multivessel CAD [12, 13]. However, PCI offers a lower level of invasiveness, a more rapid recovery, and less short-term complications than CABG in appropriately selected patients. It is widely accepted that the 128 C. Gao and M. Yang a b c d e f Fig. 8.70 CTA follow-up for TECAB. 3 months (a), 6 months (b), 1 year (c), 2 years (d), 3 years (e) and 5 years (f) after the surgery Fig. 8.71 Angiography shows that LITA graft develops a collateral branch survival advantage conferred by CABG is related to the presence of a patent left internal thoracic artery graft sewn to the left anterior descending artery [14]. Minimally invasive cardiac surgical techniques have been perfected to perform this isolated LITA-LAD revascularization [14]. Hybrid coronary artery revascularization is a combination of minimally invasive coronary artery surgery and catheter based coronary intervention. The ultimate goal of minimally invasive coronary artery bypass grafting is to perform the entire anastomosis in a closed chest. With the advent of robotically enhanced telemanipulation, the latest minimally invasive techniques are now available and thus enable true closed chest totally endoscopic procedures. The hybrid concept is gaining renewed interest because totally endoscopic LITA to LAD has become feasible and placement of drug-eluting stents in non-LAD targets may be competitive even for arterial bypass grafts. The concept of hybrid revascularization is first discussed and applied clinically when placement of the left internal mammary artery to the left anterior descending artery becomes feasible through mini-thoracotomies [15, 16]. 8 Robotic Coronary Bypass Graft on Beating Heart 129 Fig. 8.74 Six months after the surgery with well-healed incisions Fig. 8.72 A male patient, 1 month after TECAB Fig. 8.73 A female patient, 3 months after TECAB 8.4.1 Patient Selection Inclusion criteria for the hybrid procedure are patients with double-vessel or triple-vessel disease in whom LAD lesions are not suitable for PCI but suitable for surgical bypass and in whom non-LAD lesions are amenable to PCI. Selecting patients for hybrid coronary revascularization (HCR) involves close consultation between cardiac surgeon and interventional cardiologist. The surgeon and cardiologist must address specific concerns regarding the suitability of coronary anatomy as well as clinical characteristics as far as the specifics of minimally invasive LITA-LAD revascularization are concerned. Angiography should be carefully reviewed for the suitability of LAD for surgical grafting. A large distal LAD will provide the best incremental advantage to LITA-LAD revascularization compared with multivessel stenting. Very small LAD targets or obvious long intramyocardial LAD segments may pose significant technical challenges to the minimally invasive surgeon and should be approached carefully. Total chronic occlusions of LAD can be safely approached with minimally invasive LITA-LAD. The non-LAD targets should be reviewed in detail for PCI options. An estimation of both the technical considerations and the possible long-term success of PCI should be considered. Decisions regarding the possible aggressiveness of PCI should be based on HCR strategy, as the presence of a patent LITA-LAD graft may change the safety margin for the interventional cardiologist. In general, a suitable LAD with focal proximal lesions in the right coronary artery and/or circumflex distribution provides the best conditions for HCR [14]. The need for single-lung ventilation and chest cavity insufflation raises important considerations when selecting patients for robotic CABG. Absolute exclusion criteria for robotic CABG include patients with severe chronic obstructive pulmonary disease who cannot tolerate single-lung ventilation and patients who have had prior left chest surgery. Patients with severe pulmonary hypertension also provide a relative contraindication as rapid desaturation and hemodynamic change can compromise single-lung ventilation and thoracic cavity insufflation. Actively ischemic patients also 130 a C. Gao and M. Yang b Fig. 8.75 (a) Preoperative angiography of a patient for staged-hybrid revascularization demonstrating high-grade proximal LAD lesion. (b) Angiography on the fifth day after operation of patent LITA-LAD anastomosis at the time of staged-hybrid revascularization a b Fig. 8.76 Successful percutaneous coronary intervention of the right coronary artery. (a) pre-stent. (b) post-stent pose a challenge. Chest insufflation can exacerbate ischemia and result in malignant arrhythmias which can be challenging to handle [14]. From April 2007 to May 2013, 35 patients with right coronary artery or circumflex coronary stenosis received stent placement after robotic LITA to LAD surgery in staged session [17]. The average age of the patients was 62.3 ± 12.1 years old. Three patients were female and 32 were male. All patients underwent preoperative computed tomographic scan of the thorax and pulmonary function tests. Four to five days following the robotic LITA to LAD surgery, routine stent placement was performed on these patients in the catheter lab. At same time, angiographic confirmation of LITA-LAD graft patency was verified (Fig. 8.75a, b) and successful PCI of the right coronary and/or circumflex artery followed (Figs. 8.76a, b, and 8.77). No patient complained of complications. 8 Robotic Coronary Bypass Graft on Beating Heart Fig. 8.77 CTA follow-up for hybrid coronary revascularization 8.5 Summary Endoscopic operations have associated with nearly all surgical disciplines over the last two decades and have become the standard of care [18]. In cardiac surgery and specifically for coronary artery bypass grafting, the use of minimally invasive techniques has been a challenge for the following reasons: First, most procedures are already complex, and endoscopic approaches further increase the degree of complexity; second, the cardiac surgery community has no experience in endoscopic surgery until recently; and finally, early attempts to perform CABG with the use of conventional thoracoscopic instrumentation failed completely [18, 19]. Endoscopic instrumentation, with only four degrees of freedom, significantly reduces the dexterity needed for delicate cardiac surgical procedures, and the loss of depth perception by using two dimensional video monitors further increases the operative difficulty. Robotic surgery provides a solution to these problems and represents a paradigm shift in the delivery of healthcare for both the patient and the surgeon [20]. Mitral valve repair has been the most common application of robotic technology in cardiac surgery. On the basis of the success of robotic mitral surgery, surgical telemanipulation has expanded to other cardiac procedures such as coronary revascularization. Robotic coronary operations range from internal mammary artery harvest with a hand-sewn anastomosis, performed either on- or off-pump through a mini-thoracotomy or median sternotomy, to totally endoscopic coronary artery bypass grafting. The initial clinical expectation for robotic coronary surgery was ITA takedown and completion of CABG through sternotomy or minithoracotomy. Early reports demonstrated the feasibility and safety of harvesting 131 IMA with the da Vinci system with harvest time 30 min achievable once the learning curve had been negotiated [21]. In another study, by Duhaylongsod and coworkers [22], harvest time was 42–55 min. Our mean harvest time is 30.8 min, and the time decreases as case number increases. Our experience demonstrates that thoracoscopic LITA takedown using da Vinci telemanipulator is safe. ITA harvest can be completed as described above. Robotic endoscope is helpful in localizing the coronary target vessels, and also assists in identification of the correct intercostal space through which the target vessel is approached for anastomosis, though the minithoracotomy is most commonly performed in the fourth left intercostal space. Small thoracotomy retractors or less traumatic soft tissue retractors enhance the exposure of the target vessel and allow the use of standard surgical microinstrumentation for direct suturing by hand [18]. Although MIDCAB minimizes the morbidity of a full-sternotomy incision, concerns are about the quality of anastomosis of LITA to LAD, LITA graft patency rates, a steep learning curve for surgeons and the technical difficulties associated with the procedure. Now the outcomes published for robotically assisted MIDCAB show no perioperative mortality and low complication rates [23–28]. Often these incisions can be limited to 5–8 cm and yield excellent cosmetic results. In women, MIDCAB scars can be easily hidden in the inframammary crease. Patient satisfaction and rapid recovery following MIDCAB have been achieved. Preliminary studies suggested excellent long-term patency of grafts following MIDCAB. At our center, 120 patients underwent robotic MIDCAB on beating heart with excellent follow-up results. The study showed that the graft patency was 97.1 % in the period of 1–54 months. The ultimate goal of minimally invasive CABG is to perform the entire anastomosis in a closed chest, to avoid the deleterious effects of CPB and to minimize incisions and surgical trauma. TECAB on beating heart has brought minimally invasive CABG close to this goal. TECAB is technically demanding. Several critical issues have to be emphasized for successful surgery. Although TECAB is feasible and safe [17, 29, 30], proper planning and patient selection are critical for success, and grafting strategy should never be compromised to complete revascularization. Firstly, the patients’ comorbidities should be considered. All patients with pulmonary disease and/or poor ejection fraction should be excluded since poor hemodynamics or low cardiac output could develop during the procedure due to CO2 insufflation which decreases venous return. In addition, cardiac stabilization could further decrease cardiac output. Secondly, the location, quality, and trajectory of the target vessel should be considered. This is more important in TECAB than in open heart surgery because the artery sometimes can be quite difficult to be found if the vessel is located in the fat or intramyocardial vessel. In our group, one case was converted to MIDCAB due to intramyocardial LAD during operation. If the vessel is calcified, it could be more difficult to perform anastomosis robotically. Therefore, we 132 consider that diffuse calcified and intramyocardial vessels should be exclusion criteria for TECAB procedure. Thirdly, the diameter of the vessel is important. In OPCAB surgery, the bigger the vessel, the easier the anastomosis and the better the results. Totally occluded arteries are ideal target vessels since ischemia rarely happen during vessel occlusion and the time to perform the coronary anastomosis is not an issue [31]. However, using da Vinci Surgical System, we find that the diameter of the vessel is not a problem for anastomosis since a 3-D 10× magnified view and EndoWrist instruments allow for very precise placement of the U-Clips as long as the quality of the target vessel is good. We also find that the quality of totally occluded vessel is usually not as ideal as we expect. Therefore, we believe that the quality of the target vessel is of paramount importance. Suturing of the anastomosis is the most demanding part of TECAB on beating heart because under the 10× magnification even the slightest movement of the target vessel could compromise surgical manipulation, and due to lack of tactile feedback, sometimes it is difficult to assess the quality of the vessel wall. Therefore, it could be awkward to find the right position for placing a stitch. Interrupted anastomosis reduces the possibility of purse stringing of a continuous suture and helps to overcome the lack of tactile feedback inherent with the da Vinci Surgical System [30]. Moreover, intravascular ultrasonography has proven that interrupted anastomosis with surgical U-Clips is more compliant than anastomosis with running sutures [32]. We also find that big bite of U-Clips at the outside of the incision of target vessel is helpful for hemostasis. Since the heart is not decompressed by using CPB and the space in the thoracic cavity is limited, CO2 pressure may be increased above the suggested value up to 15 mmHg as long as the heart is filled sufficiently and contractility is not impaired. We must emphasize that the endostabilizer should not be compressed too much on the heart to avoid compromising contractility. A lighter touch rather than heavy compression can also minimize the bouncing effect of the beating heart. In addition, ischemic preconditioning may be useful for longer anastomotic time in instances of less than 80–90 % stenosis in a large proximal LAD. It is important to remember to rely on visual cues. Therefore, we believe that robotic cardiac surgery should be conducted by surgeons with extensive surgical experience in open techniques. Optimal anesthesia will minimize occurrence of ischemia in the target coronary arteries with significant stenosis. The crucial issue of anesthesia for the surgery is to deal with the hemodynamic compromise, hypoxia and hypercarbia associated with single-lung ventilation, and intrathoracic insufflation of CO2 with positive pressure [33]. The results of MIDCAB procedure with harvesting of the mammary vessel and coronary anastomosis through a minithoracotomy are established [34–36]. In our group, two cases were converted to MIDCAB during operation. One was due to intramyocardial LAD, in which we found intramyocardial LAD was difficult to be anastomosed to LIMA robotically. The other was due to diffuse calcified RCA. We anastomosed C. Gao and M. Yang the right IMA to the diffuse calcified RCA robotically, however, blood flow was not satisfactory. We therefore explored the anastomosis with an infraxyphoid incision. The intraoperative exclusion or conversion was not considered as failure of therapy as all these patients would have required an open approach. Therefore, when necessary, we recommend conversion to a MIDCAB procedure which allows excellent results with normal operating time. Robotic cardiac surgery requires real teamwork and the surgeons must overcome a substantial learning curve before they finally master TECAB. Median time for ITA harvesting and operation is significantly shortened with surgical experience in terms of number of operations, but IMA harvest time drops more rapidly than anastomosis time with experience. Our learning curve is truncated because the author, as the console surgeon, simultaneously has performed a large volume of various kinds of other robotic cardiac surgeries with the same team in a relatively short time [37–45], and has the experience of over 2,000 cases of OPCAB surgery [46, 47]. Since we started the robotic surgical program, our robotic team members have remained the same. Our experience shows that with well trained robotic team and after a substantial learning curve, we could achieve optimal results for TECAB on beating heart. In conclusion, TECAB is a safe procedure for coronary bypass grafting in selected patients, and produces excellent early and midterm patency of anastomosis and surgical results. Surgeons with extensive surgical experience in open techniques, a stable and well trained robotic team and substantial learning curves certainly ensure the perfection of TECAB procedure. References 1. Loulmet D, Carpentier A, d’Attellis N, et al. Endoscopic coronary artery bypass grafting with the aid of robotic assisted instruments. J Thorac Cardiovasc Surg. 1999;118:4–10. 2. Takami Y, Ina H. Effects of skeletonization on intraoperative flow and anastomosis diameter of internal thoracic arteries in coronary artery bypass grafting. Ann Thorac Surg. 2002;73:1441–5. 3. Tomita S, Watanabe G. Totally endoscopic internal artery harvesting. Innovations. 2006;1:243–6. 4. Gil B, Walter WS, Trevor CA, et al. Robotic skeletonizing of the internal thoracic artery: is it safe? Ann Thorac Surg. 2004;77:1262–5. 5. Bonatti J, Schahner T, Bonaros N, et al. Technical challenges in totally endoscopic robotic coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2006;131:146–53. 6. Armin O, Nikolaos B, Thomas S, et al. Robotic endoscopic left internal mammary artery harvesting: what have we learned after 100 cases? Ann Thorac Surg. 2007;83:1030–4. 7. Bolotin G, Scott W, Austin T, et al. Robotic skeletonizing of the internal thoracic artery: is it safe? Ann Thorac Surg. 2004;77: 1262–51265. 8. Falk V, Diegeler A, Walther T, et al. Total endoscopic computer enhanced coronary artery bypass grafting. Eur J Cardiothorac Surg. 2000;17:38–45. 9. Reuthebuch O, Comber M, Gruenenfelder J, Zund G, Turina M. Experiences in robotically enhanced IMA preparation as initial step towards totally endoscopic coronary artery bypass grafting. Cardiovasc Surg. 2003;11:483–7. 8 Robotic Coronary Bypass Graft on Beating Heart 10. Falk V, Diegeler A, Walther T, Jacobs S, Raumans J, Mohr FW. Total endoscopic off-pump coronary artery bypass grafting. Heart Surg Forum. 2000;3(1):29–31. 11. de Canniere D, Wimmer-Greinecker G, Cichon R, Gulielmos V, Van Praet F, Seshadri-Kreaden U, Falk V. Feasibility, safety, and efficacy of totally endoscopic coronary artery bypass grafting: multicenter European experience. J Thorac Cardiovasc Surg. 2007;134:710–6. 12. Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–72. 13. The Bypass Angioplasty Revascularization Investigation (BARI) Investigators. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med. 1996; 335:217–25. 14. Seshasayee N, Vankeepuram S, Joseph JD. Hybrid coronary revascularization. Cardiol Rev. 2011;19:101–7. 15. Angelini GD, Wilde P, Salerno TA, Bosco G, Calafiore AM. Integrated left small thoracotomy and angioplasty for multivessel coronary artery revascularization. Lancet. 1996;16:757–8. 16. de Cannière D, Jansens JL, Goldschmidt-Clermont P, Barvais L, Decroly P, Stoupel E. Combination of minimally invasive coronary bypass and percutaneous transluminal coronary angioplasty in the treatment of double-vessel coronary disease: two-year follow-up of a new hybrid procedure compared with “on-pump” double bypass grafting. Am Heart J. 2001;142:563–70. 17. Gao C, Yang M, Wang G, et al. Hybrid coronary revascularization by endoscopic robotic coronary artery bypass grafting on beating heart and stent placement. Ann Thorac Surg. 2009;87:737–41. 18. Bonatti J, Schahner T, Bonaros N, et al. Robotically assisted totally endoscopic coronary bypass surgery. Circulation. 2011;124: 236–44. 19. Stevens J, Burdon T, Siegel L, Peters W, Pompili M, St Goar F, Berry GJ, Ribakove GH, Vierra MA, Mitchell RS, Toomasian JM, Reitz BA. Port-access coronary artery bypass with cardioplegic arrest: acute and chronic canine studies. Ann Thorac Surg. 1996;62:435–40. 20. Modi P, Rodriguez E, Chitwood WR. Robot assisted cardiac surgery. Interact Cardiovasc Thorac Surg. 2009;9:500–5. 21. Vassiliades TA. Technical aids to performing thoracoscopic robotically assisted internal mammary artery harvesting. Heart Surg Forum. 2002;5:119–24. 22. Duhaylongsod F, Mayfield W, Wolf RK. Thoracoscopic harvest of the internal thoracic artery: a multicenter experience in 218 cases. Ann Thorac Surg. 1998;66:1012–7. 23. Derose JJ, Balaram SK, Ro C, Swistel DG, Singh V, Wilentz JR, Todd GJ, Ashton RC. Mid-term results and patient perceptions of robotically assisted coronary artery bypass grafting. Interact Cardiovasc Thorac Surg. 2005;4:406–11. 24. Subramanian V, Patel N, Patel N, Loulmet D. Robotic assisted multivessel minimally invasive direct coronary artery bypass with port-access stabilization and cardiac positioning: paving the way for outpatient coronary surgery? Ann Thorac Surg. 2005;79:1590–6. 25. Turner WF, Sloan JH. Robotic-assisted coronary artery bypass on a beating heart: initial experience and implications for the future. Ann Thorac Surg. 2006;82:790–4. 26. Srivastava S, Gadasalli S, Agusala M, Kolluru R, Naidu J, Shroff M, Barrera R, Quismundo S, Srivastava V. Use of bilateral internal thoracic arteries in CABG through lateral thoracotomy with robotic assistance in 150 patients. Ann Thorac Surg. 2006;81:800–6. 27. Kon ZN, Brown EN, Tran R, Joshi A, Reicher B, Grant MC, Kallam S, Burris N, Connerney I, Zimrin D, Poston RS. Simultaneous hybrid coronary revascularization reduces postoperative morbidity compared with results from conventional off-pump coronary artery bypass. J Thorac Cardiovasc Surg. 2008;135:367–75. 28. Poston RS, Tran R, Collins M, Reynolds M, Connerney I, Reicher B, Zimrin D, Griffith BP, Bartlett ST. Comparison of economic and 133 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. patient outcomes with minimally invasive versus traditional offpump coronary artery bypass grafting techniques. Ann Surg. 2008;48:638–48. Gao C, Yang M, Wu Y, Wang G, et al. Early and midterm results of totally endoscopic coronary artery bypass grafting on the beating heart. J Thorac Cardiovasc Surg. 2011;142(4):843–9. Srivastava S, Gadasalli S, Agusala M, Kolluru R, Barrera R, Quismundo S, Kreaden U, Jeevanandam V. Beating heart totally endoscopic coronary artery bypass. Ann Thorac Surg. 2010;89:1873–80. Folliguet T, Dibie A, Philippe F, Larrazet F, Slama M, Laborde F. Robotically-assisted coronary artery bypass grafting. Cardiol Res Pract 2010;Article ID 175450, 6 pages. doi:10.4061/2010/175450. Hamman B, White C. Interrupted distal anastomosis: the interrupted “porcupine” technique. Ann Thorac Surg. 2004;78:722–4. Wang G, Gao C, Zhou Q, Chen T. Anesthesia management for robotically assisted endoscopic coronary artery bypass grafting on beating heart. Innovations. 2010;5(4):291–4. Kappert U, Cichon R, Schneider J, Gulielmos V, Ahmadzade T, Nicolai J, Tugtekin SM, Schueler S. Technique of closed chest coronary artery surgery on the beating heart. Eur J Cardiothorac Surg. 2001;20(4):765–9. Bonatti J, Schachner T, Bonaros N, Jonetzko P, Ohlinger A, Ruetzler E, Kolbitsch C, Feuchtner G, Laufer G, Pachinger O, Friedrich G. Simultaneous hybrid coronary revascularization using totally endoscopic left internal mammary artery bypass grafting and placement of rapamycin eluting stents in the same interventional session: the combination pilot study. Cardiology. 2008;110(2):92–5. Kiaii B, McClure RS, Stewart P, et al. Simultaneous integrated coronary artery revascularization with long-term angiographic follow-up. J Thorac Cardiovasc Surg. 2008;136:702–8. Gao C. Development and current status of robotic cardiac surgery. Chin J Clin Thorac Cardiovasc Surg. 2011;27(7):385. Gao C, Yang M, Wang G, Xiao CS, Wang JL, Wu Y, Wang Y. Clinical analysis of robotic mitral valve replacement. Chin J Clin Thorac Cardiovasc Surg. 2011;27(7):390–2. Gao C, Yang M, Wang G, Wang JL, Xiao CS, Wu Y, Wang Y. The observation of 40 cases of totally myxoma resection. Chin J Clin Thorac Cardiovasc Surg. 2011;27(7):393–4. Gao C, Yang M, Wu Y, Wang G, Xiao CS, Wang JL, Li LX, Zhao Y, Zhou Q. Treatment of multiple vessel coronary artery disease by robotic bypass surgery on the beating heart and stent placement in distinct hybrid session. Chin J Clin Thorac Cardiovasc Surg. 2011;27(7):389–400. Gao C, Yang M, Wang G, Wang JL, Wu Y, Wang Y. Clinical analysis of robotic mitral valve repair. Zhonghua Wai Ke Za Zhi. 2011;49(7):641–4. Gao C, Yang M, Wang G. Totally endoscopic robotic ventricular septal defect repair. Innovations. 2010;5(4):278–80. Gao C, Yang M, Wang G, Xiao CS, Wu Y, Li JC. Excision of atrial myxoma using robotic technology. J Thorac Cardiovasc Surg. 2010;139(5):1282–5. Gao C, Yang M, Wang G, Wang JL. Totally robotic resection of myxoma and atrial septal defect repair. Interact Cardiovasc Thorac Surg. 2008;7(6):947–50. Gao C, Yang M, Wang G, Wu Y, Zhao Y, Li LX, Wang JL, Xiao CS, Zhou Q. Minimally invasive robotic coronary bypass on the beating heart using da Vinci S system. Zhonghua Wai Ke Za Zhi. 2008;47(8):570–3. Gao C, Li BJ, Xiao CS, Wang G, Jiang SL, Wu Y, Ma XH, Zhu LB, Liu GP, Sheng W. Clinical analysis of 1018 cases of coronary artery bypass grafting. Zhonghua Wai Ke Za Zhi. 2005;43(14):929–32. Gao C, Liu ZY, Li BJ, Xiao CS, Wu Y, Wang G, Yang L, Liu GP. Comparison of graft patency for off-pump and conventional coronary arterial bypass grafting using 64-slice multidetector spiral computed tomography angiography. Interact Cardiovasc Thorac Surg. 2009;8:325–9. 9 Hybrid Coronary Revascularization Mukta C. Srivastava, Bradley Taylor, David Zimrin, and Mark R. Vesely Abstract Hybrid coronary revascularization (HCR) is a treatment strategy for revascularization of multi-vessel coronary artery disease that utilizes minimally invasive coronary artery bypass grafting (CABG) techniques in conjunction with percutaneous coronary intervention (PCI), integrating the advantages of both. The long-term symptom relief and survival benefit of an internal mammary artery (IMA) graft to the left anterior descending (LAD) artery are attained in this approach, as well as the durability of PCI with drug-eluting stents (DES) to non-LAD targets. This chapter will review the range of minimally invasive surgical techniques that form the basis of the surgical leg of HCR, address pharmacologic issues unique to HCR, and finally to review logistical considerations in the sequencing of each leg of HCR, surgical and percutaneous. Keywords Hybrid coronary revascularization • Percutaneous coronary intervention • Minimally invasive surgery • Totally endoscopic coronary artery bypass 9.1 Introduction Hybrid coronary revascularization (HCR) is a treatment strategy for the revascularization of multi-vessel coronary artery disease that utilizes minimally-invasive coronary artery bypass grafting (CABG) techniques in conjunction with percutaneous coronary intervention (PCI), integrating the advantages of both. The long-term symptom relief and survival benefit of an internal mammary artery (IMA) graft to the left anterior descending (LAD) artery are attained in this approach, as well as the durability of PCI with drug-eluting stents (DES) to nonLAD targets [1–6]. Furthermore, early ambulation and discharge and reduced morbidity are afforded by the M.C. Srivastava, MD (*) • B. Taylor, MD • M.R. Vesely, MD Division of Cardiology, University of Maryland Medical Center, 110 South Paca St., Baltimore, MD 21201, USA e-mail: msrivast@medicine.umaryland.edu D. Zimrin, MD Department of Medicine, University of Maryland School of Medicine, Baltimore, MD, USA minimally-invasive nature of the surgical and percutaneous interventions, which are performed without median sternotomy or institution of central by-pass [7–9]. Hybrid strategies have also included valve replacement combined with PCI, percutaneous valve therapy and aortic de-branching procedures combined with endovascular grafting [6]. The advent of HCR, as well as percutaneous structural heart interventions and endovascular techniques have been an impetus for the development of state-of-the-art hybrid operating suites that facilitate the performance of cardiac surgery and PCI in the same procedural setting. Minimally-invasive surgical techniques have progressed, with advanced operators performing totally endoscopic coronary artery bypass (TECAB). Likewise, stent technology has advanced and the introduction of second generation DES, with lower stentthrombosis and re-stenosis rates, has made them competitive as a revascularization approach compared with saphenous vein grafts (SVGs) for non-LAD targets. Development in interventional techniques and lesion modification technologies such as rotational atherectomy have also broadened the lesion subtypes amenable to percutaneous therapy. C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_9, © Springer Science+Business Media Dordrecht 2014 135 136 M.C. Srivastava et al. A consideration unique to HCR is the sequence of surgical and percutaneous intervention and the timing of these in relation to one another. In this regard, there are important implications for anti-coagulation and anti-platelet therapy, ischemia burden during either leg of revascularization, the ability to assess graft patency with completion angiography, and the ability to perform rescue surgical grafting for a failed PCI attempt. The optimal sequence of revascularization for HCR with TECAB and PCI has not been determined. Reports on HCR results have been published. HCR uses minimally-invasive surgical techniques that range from those requiring mini-thoracotomies to totally endoscopic approaches. These results have demonstrated low mortality rates ranging from 0–2 %, shorter intensive care unit and hospital lengths of stay, as well superior cosmetic results and shorter recovery times. While results are encouraging, logistical and political factors have limited widespread adoption of the HCR approach. High-volume centers still perform only 5 % of CABG case volume via an HCR approach. Technical demands and learning curves associated with minimally invasive coronary artery bypass grafting techniques also importantly contribute to limiting HCR volume [6]. This chapter are to review the range of minimally-invasive surgical techniques that form the basis of the surgical leg of HCR, address pharmacologic issues unique to HCR, and finally to review logistical considerations in the sequencing of each leg of HCR, surgical and percutaneous. 9.2 composite outcome was not significantly different (5.6 % versus 7.0 %, respectively; p = 0.19). The overall rate of graft patency was lower in the off-pump group however the patency rate for left-internal mammary artery pedicle grafts to the LAD was not significantly different (95.3 % versus 96.2 %, respectively; p = 0.48). In an analysis by Puskas et al., off-pump CABG was found to disproportionately benefit high-risk surgical patients with an operative mortality benefit noted in patients with a Society of Thoracic Surgeons Predicted Risk of Mortality (PROM) greater than 2.5–3 % [10]. 9.4 In the Mid-CAB technique, LIMA to LAD revascularization is performed via a mini-thoracotomy and utilizing off-pump CABG technique, thereby eliminating CPB and need for mid-line sternotomy. Decreased bleeding and infection rates compared with off-pump CABG have also been appreciated. Typically thoracotomy is performed in the fourth or fifth interspace. Costal cartilage removal or disarticulation is sometimes required for adequate visualization. Large MidCAB series have been reported in the literature with shortterm LIMA to LAD patency rates of 95–97 % [5]. The first series of Mid-CAB LIMA to LAD revascularization combined with PCI of non-LAD vessels was reported by Angelini et al. in 1996 [12]. Minimally Invasive LAD Revascularization 9.5 The two components of cardiac surgery that impose significant morbidity risk are the institution of cardiopulmonary bypass (CPB) and the sternotomy incision [10]. Minimallyinvasive surgical techniques have focused on eliminating the need for CPB and the development of sternal-sparing techniques. 9.3 Minimally Invasive Direct Coronary Artery Bypass Grafting (Mid-CAB) Off-Pump CABG Off-pump CABG utilizes stabilizer technology to allow performance of coronary artery bypass revascularization on the beating heart. The elimination of CPB provides the potential advantages of reduced myocardial depression and cerebral dysfunction and a lower incidence of pulmonary complications as well as avoidance of a generalized systemic inflammatory response [11]. These benefits are tempered by the concern for lower overall graft patency rates, a higher incidence of peri-operative MI and less complete revascularization. In the ROOBY trial of 2,203 patients randomized to on-pump versus off-pump CABG, the rate of the 30-day Totally Endoscopic Coronary Artery Bypass Grafting (TECAB) TECAB entails thoracoscopic mobilization of the LIMA as well as robotic LIMA to LAD anastomosis without implementing median sternotomy or thoracotomy. A consideration for this approach is the need for single-lung ventilation and chest cavity insufflation to develop the virtual space of the anterior mediastinum in which the LIMA lies. The chest is insufflated with carbon dioxide, inducing a controlled pneumothorax with cardiac displacement. Resulting hemodynamic instability, as left and right-sided filling pressures drop and oxygenation is altered, is managed with pre-emptive volume loading and peripheral vasoconstriction. In this approach, peripheral bypass with an intra-aortic balloon occluder for cardioplegic arrest is instituted for arrested heart TECAB [5]. Finally, in the beating-heart TECAB approach, revascularization is performed without CPB or median sternotomy and both the LIMA takedown and anastomosis are performed robotically. Srivastava et al. described the largest published series of beating-heart TECAB of 214 patients, reporting an early graft patency, assessed by computed tomography 9 137 Hybrid Coronary Revascularization angiography (CTA) or angiography, of 99 % and clinical freedom from graft failure and re-intervention at a mean of 528 ± 697 days in 98.6 % of patients [13]. Gao et al. reported TECAB on beating heart of 90 patients; the early and midterm graft patency was 98.8 %, assessed by angiography [14]. And Gao et al. report hybrid coronary revascularization by total endoscopic robotic coronary artery bypass grafting on beating heart and stent placement in 2009[15]. Bonatti et al. reported an intention-to-treat intermediate-term experience of 226 patients undergoing HCR via arrested heart and beating heart TECAB with 5-year bypass graft patency and 5-year freedom from MACCE comparable to patients undergoing open CABG [16]. 9.6 Patient Selection Patient selection for HCR is a collaborative effort between the cardiac surgeon and interventional cardiologist, comprising the Heart Team approach. In this merger, the cardiac surgeon and the interventional cardiologist evaluate the clinical and anatomical features of each patient to develop an optimal revascularization strategy. Indications and contraindications for consideration for HCR as detailed by Popma and colleagues are listed in Tables 9.1 and 9.2 respectively [17]. Specific considerations include anatomic suitability for a hybrid revascularization as well as clinical characteristics of the patient. Small caliber LAD vessels or significant intramyocardial segments pose technical challenges for a minimally invasive approach. Non-LAD targets should be reviewed for suitability of percutaneous intervention in terms of anatomic complexity and likelihood of long-term patency. Considerations regarding patient clinical characteristics include ability to tolerate single-lung ventilation and the hemodynamic aberrations associated with chest cavity insufflation. The ideal anatomy is a small cardiac silhouette with a large left pleural space. Thus absolute exclusion criteria for minimally-invasive cardiac surgery utilizing robotic assistance via thoracoscopic guidance include a history of severe chronic obstructive pulmonary disease who cannot tolerate single-lung ventilation and history of previous left chest surgery. Patients with severe pulmonary hypertension have a relative contraindication as rapid desaturation and hemodynamic compromise are poorly tolerated. Importantly actively ischemic patients can decompensate with the imposition of chest insufflation [5]. Leacche and colleagues evaluated 30-day outcomes of patients undergoing HCR stratified by Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) score and the European System for Cardiac Operative Risk Evaluation (euroSCORE). In comparison with patients undergoing conventional CABG, patients with high SYNTAX scores (≥33) and elevated Table 9.1 Indications for hybrid coronary revascularization Emergency revascularization of non-LAD target with residual LAD disease Insufficient native vessel size or absence of venous conduits Non-LAD lesions located in vessels not ideal for SVG long-term patency or placement Absence of suitable venous conduits due to prior vein stripping High-risk co-morbidities Adapted from Popma et al. [17] Table 9.2 Contraindications to HCR Clinical conditions: Hemodynamic instability Decompensated heart failure Chronic lung disease with FEV1 < 50 % predicted Coagulopathy Malignant ventricular arrhythmias Recent large myocardial infarction Prior left thoracotomy Exclusion for PCI Exclusion for thoracoscopic LIMA-LAD grafting Unusable or previously used LIMA Previous thoracic surgery involving the left pleural space Poor quality or diffusely diseased LAD Chest wall irradiation Left subclavian artery stenosis Adapted from Popma et al. [17] euroSCORES (>5) faired better with conventional CABG, with higher bleeding complications and a higher incidence of the composite end-point of death from any cause, stroke, myocardial infarction and low cardiac output syndrome [18]. Thus, HCR may not be an ideal strategy for clinically highrisk patients with complex anatomy. 9.7 Anti-coagulation/Platelet Inhibition An important consideration for HCR is the anti-coagulation and platelet inhibition strategy as the risk of surgical bleeding has to be balanced with the risk of stent thrombosis [19]. These considerations are most relevant when HCR is performed in a same-session approach or when PCI has been performed prior to the surgical revascularization arm. Unfractionated heparin is the most commonly used anticoagulant for both PCI and CABG procedures as anti-coagulant effect can be monitored by measuring activated clotting times (ACTs) and can be reversed with protamine. Low-molecular weight heparin is a less attractive option for cardiac surgery, limited by its long half-life and irreversibility. Typical heparin reversal with protamine is performed post-bypass, which can be problematic in an HCR approach when surgical revascularization is performed after PCI, as there is a theoretical risk of 138 M.C. Srivastava et al. stent-thrombosis with protamine administration. Interestingly, in a series comparing same-session performed HCR without protamine reversal versus standard off-pump CABG, less bleeding was noted in the HCR cohort [18]. This finding was attributed to lesser bleeding associated with minimally-invasive surgical techniques. The direct thrombin inhibitor, Bivalirudin has been evaluated as an anti-coagulation strategy in HCR with mid-CAB with demonstrated efficacy by Kiaii and colleagues [20]. In this series, Bivalirudin was administered intraoperatively during the mid-CAB of same-session HCR and continued for the PCI of the revascularization. The optimal anti-coagulation strategy has not been determined in HCR. Anti-platelet therapy is an additional consideration during HCR as PCI requires dual anti-platelet therapy (DAPT) with aspirin and an oral thienopyridine such as Clopidogrel which works at the platelet P2Y ADP receptor site. Continued DAPT through the surgical revascularization period when PCI is performed first clearly has implications for bleeding risk. Platelet inhibition strategy is most complex in the same-session approach as the timing interval between both revascularization periods is minimal. The timing of administration of a loading dose of a thienopyridine and protamine reversal are particularly relevant. Diverse strategies have been successfully implemented without a consensus in the literature regarding the ideal approach. Reicher and colleagues performed mid-CAB followed by PCI without protamine reversal with Clopidogrel loading immediately after PCI. In their series, they documented adequate platelet inhibition by 24 h by ADP-induced aggregation [8]. Zhao and colleagues have successfully used the strategy of administering a 300 mg loading dose of Clopidogrel just prior to PCI followed immediately by CABG with subsequent protamine reversal [21]. At our institution (University of Maryland), a strategy of CABG first followed by protamine reversal of heparin with subsequent re-heparinization and clopidogrel loading via NG tube for PCI after CABG has been used successfully in a same-session approach. 9.8 Sequence of Revascularization The optimal sequence of revascularization in HCR is not arbitrary as there are advantages and disadvantages inherent to the three potential revascularization approaches: Surgery prior to PCI versus PCI prior to surgery versus a samesession intervention where both revascularization procedures are performed in the same procedural setting with either procedure being performed first. Notably, patient presentation often dictates intervention sequence. 9.8.1 CABG Prior to PCI Approach When surgical revascularization is performed as the initial intervention, an important advantage is that an improvement in safety profile of subsequent PCI as typical revascularization in the large LAD territory has been established. Furthermore, anti-coagulant use and platelet inhibition during the interventional procedure can be optimized for PCI result rather than tailored to avoid surgical bleeding. Completion angiography to assess graft patency can also be performed in this approach. While the utility of completion angiography is controversial, in an analysis by Zhao et al. of 366 patients who underwent routine completion angiography after conventional coronary artery bypass grafting (CABG), 12 % of grafts were found to have important angiographic defects, with 2.8 % undergoing subsequent repair [21]. Complex lesion subsets such as bifurcation left main disease are ideally approached with CABG performed initially as this allows for a reduction in the complexity of both the surgical and interventional procedures as well as a significant improvement in the safety profile of subsequent PCI. For example, a left main bifurcation lesion presents a complex target for PCI and requires double-vessel grafting if CABG is utilized. However, both revascularization procedures are simplified by HCR. The LAD may be revascularized by placement of a single arterial graft to the LAD, a less complex surgery than double vessel-bypass. This can then be followed by protected left main stenting into the circumflex vessel, a significantly lower-risk intervention than unprotected bifurcation left main stenting. Similar improvements in the complexity and safety of other complex lesion subsets can also be realized with the CABG-first approach. Figure 9.1 illustrates a complex trifurcation lesion revascularized via HCR. A disadvantage inherent to this approach is the potential for significant ischemia burden during CABG if lesions planned for subsequent PCI subtend a large area of myocardium. Importantly, significant ischemia can result in hemodynamic instability with end-organ dysfunction, particularly relevant with proximal RCA disease where right ventricular and left ventricular dysfunction can complicate the intraoperative course. An additional disadvantage with this approach is the inability to perform rescue surgical revascularization if PCI fails without embarking on a second, highrisk surgical intervention. 9.8.2 PCI Prior to CABG Approach When HCR is performed in a staged fashion with PCI prior to CABG, a sub-optimal interventional result can be achieved with subsequent surgical revascularization. Additionally, when the area of myocardium subtended by the vessel planned for PCI is large, initial PCI reduces ischemic burden during CABG. Conversely, initial PCI in the setting of significant un-revascularized disease, particularly in the LAD territory, is a higher-risk procedure. By default, patients presenting with acute coronary syndromes will undergo percutaneous intervention to a culprit vessel prior to multi-vessel revascularization. 9 Hybrid Coronary Revascularization 139 a b c d Fig. 9.1 Simplification of a complex lesion. Panel a demonstrates a complex distal left main trifurcation lesion involving the LAD, left circumflex and ramus vessels. Panels b and c show placement of a right internal mammary artery graft anastomosed to the LAD with a radial artery Y-graft placed to a PDA lesion and a LIMA graft placed to the LAD via TECAB. Panel d shows subsequent protected left main into ramus vessel PCI (Reproduced with permission from Lee et al. [22]) A disadvantage of the PCI-first approach is that it requires that CABG be performed on dual anti-platelet therapy while imposing limitations on the interventionalist for choice and duration of anti-coagulant therapy. Additionally, there is a theoretically increased risk of stent-thrombosis from platelet activation when protamine is administered during cardiac surgery. This risk is thought to be more prominent in the offpump versus on-pump setting [6]. patient comfort need to be balanced with financial considerations such as hospital LOS. In the same-session approach, complete revascularization is performed in one procedural setting, shortening the interval between each revascularization period, which are still performed independently. The risk of bleeding due to anti-coagulation for PCI in the immediate post-operative period and the potential for acute in-stent thrombosis due to performing PCI in the post-operative inflammatory state are still relevant. The primary benefit of this approach is complete revascularization in one procedural setting while maintaining the ability to perform completion angiography and approach complex lesion subsets in the environment of a surgically-equipped hybrid operating suite. A shorter length of stay would be expected with this approach. 9.8.3 Same-Session Revascularization Approach The ideal duration of time between surgical and percutaneous intervention remains indeterminate, as safety and 140 There is likely no arbitrarily superior sequence of revascularization in HCR. Individualized selection for each strategy based on patient presentation and anatomical considerations is likely the most effective way to determine the order of interventions. Patients presenting with acute myocardial infarctions will typically undergo PCI first. Patients with type C lesions with a high potential for PCI failure will be better suited for a PCI first approach as well, as rescue surgical revascularization can be performed at the time of CABG. Conversely, patients with complex lesions, particularly in the left main territory, are better suited for a CABG first approach as this would allow for performance of PCI in a protected environment. A simultaneous procedure is satisfying in that it provides one-stop revascularization but creates logistical challenges involving personnel, equipment and anticoagulant/platelet inhibition strategies that must be carefully considered. Conclusion HCR is an approach for coronary revascularization that optimizes treatment modalities for particular lesion subsets and may afford the best long term patency, while maintaining the survival benefit of the LIMA graft and minimizing morbidity. The Heart Team approach merges the insight and skill-sets of both the cardiac surgeon and the interventional cardiologist to allow for optimized revascularization based on the coronary anatomy and clinical characteristics of the patient. The limitations of this approach include the availability of hybrid operating suites and the advanced technologies and skill sets required for the performance of HCR. Additionally, specific features of the approach such as optimal anti-coagulation strategies and sequence of revascularization remain to be elucidated. M.C. Srivastava et al. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. References 1. The VA Coronary Artery Bypass Surgery Cooperative Study Group. Eighteen-year follow-up in the Veterans Affairs Cooperative Study of Coronary Artery Bypass Surgery for stable angina. Circulation. 1992;86:121–30. 2. European Coronary Surgery Study Group. Long-term results of prospective randomized study of coronary artery bypass surgery in stable angina pectoris. Lancet. 1982;2:1173–80. 3. Rogers W, Coggin C, Gersh B, et al. Ten-year follow-up of quality of life in patients randomized to receive medical therapy or coronary artery bypass graft surgery. The Coronary Artery Surgery Study (CASS). Circulation. 1990;82:1647–58. 4. The Bypass Angioplasty Revascularization Investigation (BARI) Investigators. Comparison of coronary bypass surgery with 19. 20. 21. 22. angioplasty in patients with multi-vessel disease. N Engl J Med. 1996;335:217–25. Narasimhan S, Srinivas V, DeRose J. Hybrid coronary revascularization: a review. Cardiol Rev. 2011;19:101–7. Byrne J, Leacche M, Vaughan D, et al. Hybrid cardiovascular procedures. J Am Coll Cardiol Intv. 2008;1:459–68. Bonatti J, Lehr E, Vesely M, et al. Hybrid coronary revascularization: which patients? When? How? Curr Opin Cardiol. 2010;25: 568–74. Reicher B, Poston R, Mehra M, et al. Simultaneous “hybrid” percutaneous coronary intervention and minimally invasive surgical bypass grafting: feasibility, safety, and clinical outcomes. Am Heart J. 2008;155:661–7. Katz M, Van Praet F, de Canniere D, et al. Integrated coronary revascularization: percutaneous coronary intervention plus robotic totally endoscopic coronary artery bypass. Circulation. 2006; 114(Suppl I):I473–6. Puskas J, Thourani V, Kilgo P, et al. Off-pump coronary artery bypass disproportionately benefits high-risk patients. Ann Thorac Surg. 2009;88:1142–7. Shroyer A, Grover F, Hattler B. On-pump versus off-pump coronary artery bypass surgery. N Engl J Med. 2009;361:1827–37. Angelini G, Wilde P, Selerno A, et al. Integrated left small thoracotomy and angioplasty for multi-vessel coronary artery revascularization. Lancet. 1996;347:757–8. Srivastava S, Gadasalli S, Agusala M, et al. Beating heart totally endoscopic coronary artery bypass. Ann Thorac Surg. 2010;89: 1873–9. Gao C, Yang M, Wu Y, Wang G, et al. Early and midterm results of totally endoscopic coronary artery bypass grafting on the beating heart. J Thorac Cardiovasc Surg. 2011;142:843–9. Gao C, Yang M, Wang G, et al. Hybrid coronary revascularization by endoscopic robotic coronary artery bypass grafting on beating heart and stent placement. Ann Thorac Surg. 2009;87: 737–41. Bonatti J, Zimrin D, Lehr E, et al. Hybrid coronary revascularization using robotic totally endoscopic surgery: perioperative outcomes and 5-year results. Ann Thorac Surg. 2012;94:1920–6. Popma J, Nathan S, Hagberg R. Hybrid myocardial revascularization: an integrated approach to coronary revascularization. Catheter Cardiovasc Interv. 2010;75:S28–34. Leacche M, Byre J, Solenkova N, et al. Comparison of 30-day outcomes of coronary artery bypass grafting surgery versus hybrid coronary revascularization stratified by SYNTAX and euroSCORE. J Thorac Cardiovasc Surg. 2013;145(4):1–9. Zimrin D, Bonatti J, Vesely M, et al. Hybrid coronary revascularization: an overview of options for anticoagulation and platelet inhibition. Heart Surg Forum. 2010;13(6):E405–8. Kiaii B, McClure R, Stewart P, et al. Simultaneous integrated coronary artery revascularization with long-term angiographic followup. J Thorac Cardiovasc Surg. 2008;136:702–8. Zhao D, Leacche M, Balguer J, et al. Routine intra-operative completion angiography after coronary artery bypass grafting and 1-stop hybrid revascularization: results from a fully integrated hybrid catheterization laboratory/operating room. J Am Coll Cardiol. 2009;53(3):232–41. Lee JD, Vesely MR, Zimrin D, Bonatti J. Advanced hybrid coronary revascularization with robotic totally endoscopic triple bypass surgery and left main percutaneous intervention. J Thorac Cardiovasc Surg. 2012;144(4):986–7. Robotic Left Ventricular Epicardial Lead Implantation 10 Changqing Gao, Chunlei Ren, and Ming Yang Abstract Cardiac resynchronization therapy (CRT) has been considered to improve the patient’s hemodynamics, functional status and survival probability for chronic heart failure (CHF) patients. Transvenous insertion of left ventricular leads is currently the route of choice for CRT. However, technical limitations owing to individual coronary sinus (CS) and coronary venous anatomy result in a 10–15 % failure rate of left ventricular lead placement and effective biventricular pacing. The epicardial lead implantation may be the last alternative for those who cannot receive or fail lead implantation through veins. Application of robotic technology to epicardial implantation allows for high-resolution, three-dimensional vision of the ventricular surface. The robotic approach provides assurance of accurate surgical positioning, minimum trauma and improved outcomes. Approximately 30 % of patients with heart failure exhibit significant ventricular dyssynchrony secondary to alterations in intraventricular conduction. Cardiac resynchronization therapy (CRT) has an alternative for chronic heart failure (CHF) patients, and has been regarded as Class I indication for heart failure treatment in 2005 American College of Cardiology/American Heart Association (ACC/AHA) guideline [1]. Several trials have recently demonstrated significant improvement in ventricular function, exercise tolerance, quality of life, and reduction in hospitalization and mortality in patients undergoing CRT. The left ventricular (LV) lead is implanted transvenously in the majority of cases and advanced through the coronary sinus into a LV epicardial vein. However, technical limitations owing to individual coronary sinus (CS) and coronary venous anatomy result in a 10–15 % failure rate of left ventricular lead placement and effective biventricular pacing. The endovenous lead positioning can also cause many complications, such as dislocation of pacing lead, chronically enhanced pacing threshold leading to reimplantation, and phrenic nerve stimulation. C. Gao, MD (*) • C. Ren • M. Yang, MD Department of Cardiovascular Surgery, PLA General Hospital, No. 28 Fuxing Road, Beijing 100853, People’s Republic of China e-mail: gaochq301@yahoo.com Furthermore, major complications such as coronary sinus perforation may occur. The epicardial lead implantation may be the last alternative for those who cannot receive or fail lead implantation through veins. The huge trauma by sternotomy limits the application of epicardial implantation. This has caused interest in alternative techniques, such as a limited thoracotomy, video-assisted thoracoscopy or robotic approach. 10.1 Anesthesia, Patient Position The patient is positioned supine on the left edge of the operating table. After routine induction of anesthesia, doublelumen intubation is carried out for single right lung ventilation. Standard hemodynamic monitoring is used with a radial arterial line for systemic blood pressure monitoring. A central venous line or a pulmonary artery catheter can be used for central access of the cardiac monitoring. External defibrillator patches are placed on the chest and the patient is positioned supine with the left chest elevated to 30° with the aid of a small bolster under the left chest (Fig. 10.1). The operative side arm with protective padding is hung loosely and supported by a sheet. da Vinci Surgical System setup is as previously described. C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9_10, © Springer Science+Business Media Dordrecht 2014 141 142 C. Gao et al. Fig. 10.3 The pericardium is opened posterior to the phrenic nerve Fig. 10.1 The patient was positioned with the left chest elevated approximately 30° and with left arm tucked at the left side Fig. 10.4 The temporary epicardial pacing lead is sutured Fig. 10.2 Port placement for robotic left ventricular epicardial lead placement. The ports are placed in line in AAL and the working port in MAL. The tip of the instrument is allowed for the access to the ventricular surface 10.2 Surgical Technique After the expose of left chest, the endoscopic camera is inserted via a 0.8 cm incision in the 5th intercostal space (ICS) in anterior axillary line (AAL). The left and right instrument arms are inserted through two 0.8-cm trocar incisions in 3rd and 7th ICS in AAL. A 2-cm incision posterior to the camera in the 5th ICS in midaxillary line (MAL) of left side is used as working port for the introduction of the lead and sutures as necessary (Fig. 10.2). Carbon dioxide is continuously insufflated into the chest cavity via camera cannula and the CO2 insufflation at a pressure of 8–10 mmHg is used in the left pleural space to help with exposure. Special consideration has to be given to hemodynamic effects because of the impaired heart function. The instruments are controlled by a surgeon who sits at the operating console away from the operative field. The Fig. 10.5 The MEDTRONIC screw-in type epicardial pacing lead pericardium is then opened posterior to the phrenic nerve (Fig. 10.3), the lateral and posterior left ventricular wall was exposed. As the patient has complete atrioventricular block, a temporary epicardial pacing lead is sutured (Fig. 10.4) and used as standby after it is tested working normally. A screw-in type epicardial pacing lead (Fig. 10.5) is introduced to the thoracic cavity through the working port by the patient-side surgeon (Fig. 10.6) then rotated into the lateral and posterior left ventricular wall with two laps (Fig. 10.7). 10 Robotic Left Ventricular Epicardial Lead Implantation The robotic arms are used to fix the lead to the left ventricular surface by screw in fixation and the other end of lead is brought out through the right port (Fig. 10.8). The lead was tested for threshold, resistance, and lateness within the native QRS complex. A transverse incision is made at the pacemaker pocket and the previous dual chamber pacemaker is isolated and took out (Fig. 10.9), meanwhile the temporary pacemaker is working instead. The left ventricular epicardial 143 pacing lead, which is then tunneled to the pacemaker generator pocket, together with the previous right ventricular lead and the right atrial lead are all connected to the three chambers pacemaker, and these are embedded in the pocket. After the pacemaker is confirmed working smoothly, the pocket as well as the chest incisions are sutured. A thoracic drainage tube was placed and the patient was transferred to ICU. 10.3 Postoperative Management Postoperatively patients are monitored at the ICU. Discharge to an intermediate care unit takes place as soon as hemodynamics and spontaneous respiration have been adequately stabilized. Chest drains are removed when drainage reaches less than 50 mL/12 h. 10.4 Fig. 10.6 The screw-in type epicardial pacing lead is delivered by the patient side surgeon Summary Prospective randomized trials have demonstrated improvements in ventricular function, exercise capacity, and quality of life among patients undergoing ventricular resynchronization therapy via biventricular pacing [2, 3]. Transvenous insertion of LV leads is currently the route of choice for CRT. a b c d Fig. 10.7 The screw-in type epicardial pacing lead is rotated clockwise into the lateral posterior wall of the left ventricle from part (a) to part (d) 144 C. Gao et al. Fig. 10.8 The other end of lead is brought out then tested for threshold and resistance Fig. 10.10 The excellent cosmetic results after robotic left ventricular epicardial lead implantation Fig. 10.9 A transverse incision is made at the pacemaker pocket and the previous dual chamber pacemaker is isolated and took out Unfortunately, its success rate is about 75–93 %, as it is totally dependent on the inconsistent coronary venous anatomy. And the surgical synchronizing technique, as a complement of percutaneous method for severe heart failure patients, is still at the stage of development. Compared with the endovenous approach, surgical synchronization treatment has its advantages such as precise location, high successful rates of lead implantation, good surgical results and avoidance of exposure to radiation damage, but the drawbacks of surgery, for instance, surgical trauma, were inevitable. Besides, surgical approach of CRT also has limitations in critical heart failure patients. Hence, how to reduce wound is key to improving surgical synchronization treatment. With the development of minimally invasive surgical technology, some advanced medical centers has already started the study of minimally invasive approach to achieve CRT by epicardial lead implantation, and the initial results were satisfactory [4, 5], especially the robotic enhanced technology has provided a minimally invasive approach for CHF treatment (Fig. 10.10). By the virtues of high definition of 3D visualization, computer elimination of tremor and stable fixation and suturing of lead, the robotic-assisted technique has provided assurance of accurate surgical positioning, minimum trauma and improved outcomes [6–10]. The lateral and posterior basal side of LV was easy to expose during the surgery, and surgical stimulation on these sites has been proved to have better resynchronization effect than coronary sinus approach [11]. Besides, as the surgical field was locally magnified with high definition, it is easy to avoid fat, fibrosis and vessel-enriched area, and different sites can be tested in order to make sure the epicardial lead was fixed at the most delayed site of LV and achieve optimized synchronization result [12]. This effective and convenient way has uncomparable advantages compared with conventional endovenous approach by implanting the lead through the branch of veins. Moreover, limited incisions made by the robotic surgery enable the patients’ quick recovery and is especially suitable for patients with poor heart function. The initial experience has shown the safety, feasibility and effectiveness brought by robotic-enhanced application in epicardial lead implantation for CHF treatment. It is proved to be an alternative to patients failed in endovenous approach. The mid and long term results need more cases and long-term follow-up to be confirmed. 10 Robotic Left Ventricular Epicardial Lead Implantation References 1. Cleland JGF, Daubert JC, Erdmann E, et al. The Cardiac Resynchronization Heart Failure (CARE-HF) Study Investigators. N Engl J Med. 2005;352:1539–49. 2. Cazeau S, LeClerq C, Lavergne T, et al. Effects of multisite biventricular pacing in patients with heart failure and intraventricular conduction delay. N Engl J Med. 2001;344:873–80. 3. Abraham WT, Fischer WG, Smith AL, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002;346:1845–53. 4. Derose JJ, Balaram S, Ro C, et al. Midterm follow-up of robotic biventricular pacing demonstrates excellent lead stability and improved response rates. Innovations. 2006;1:105–10. 5. Atoui R, Essebag V, Wu V, et al. Biventricular pacing for end stage heart failure: early experience in surgical vs. transvenous left ventricular lead placement. Interact Cardiovasc Thorac Surg. 2008;7:839–44. 6. Gao C, Yang M, Wang G, et al. Robotically assisted mitral valve replacement. J Thorac Cardiovasc Surg. 2012;143(4 Suppl):S64–7. 145 7. Gao C, Yang M, Wang G, et al. Totally endoscopic robotic ventricular septal defect repair. Innovations. 2010;5(4):278–80. 8. Gao C, Yang M, Wang G, Wang JL, et al. Excision of atrial myxoma using robotic technology. J Thorac Cardiovasc Surg. 2010; 5(139):1282–5. 9. Gao C, Yang M, Wang G, et al. Totally robotic resection of myxoma and atrial septal defect repair. Interact Cardiovasc Thorac Surg. 2008;24(3):313–6. 10. Gao C, Yang M, Wu Y, et al. Early and midterm results of totally endoscopic coronary artery bypass grafting on the beating heart. J Thorac Cardiovasc Surg. 2011;142(4):843–9. 11. Ansalone G, Giannantoni P, Ricci R, et al. Biventricular pacing in heart failure: back to basics in the pathophysiology of left bundle branch block to reduce number of nonresponders. Am J Cardiol. 2003;91:55F–61. 12. Gao C, Ren CL, Xiao CS, et al. The robotic epicardial lead implantation in cardiac resynchronization therapy. Zhonghua Wai Ke Za Zhi. 2013;51(5):1. Index A AAL. See Anterior axillary line (AAL) Acute myocardial infarction, 17, 140 Acute pulmonary edema, 17 Adhesions, 12, 16, 113 Adult, 11, 19, 43, 60–73, 75 Airway management, 16 Airway pressure, 18, 19, 21, 24, 25 Alfentanil, 20 Alkalosis, 19 Almitrine, 18 Alveolar overdistention, 19 Analgesia, 20, 23 Anastomosis, 11, 22, 23, 111, 113, 116, 122, 123, 125–128, 130–132, 136 Anesthesia, 15–29, 34, 51, 62–63, 69, 73, 76, 84, 91, 95, 106, 111–112, 120, 132, 141–142 Anesthesiologists, 15–17, 21–26, 28, 29, 51 Anesthetics, 15, 16, 19–23, 25 Anesthetic staff, 22 Anesthetic techniques, 21–22 Angiocatheter, 51, 55–57, 63, 64, 66, 67, 73, 77, 84, 85, 87, 91, 97, 102, 106, 107 Annular dilatation, 34, 100 Annuloplasty band, 11, 92, 98, 100, 101 Annulus, 34, 36, 42, 73, 76–78, 80, 91–93, 95, 98, 99, 106, 110 Antegrade, 11, 27, 28, 39, 57–58, 60, 64, 73, 77, 84, 87, 91, 95, 97, 102, 106 Anterior axillary line (AAL), 112, 120, 142 Antianginal medications, 16 Anticlockwise direction, 107 Antihypertensive, 16 Aortic aneurysm, 17 Aortic cross clamping, 57, 60 Aortic occlusion, 27–29, 64, 67, 69, 73, 77, 91 Arndt blocker, 17 Arrested heart, 11, 63–69, 71, 87, 111, 119, 136, 137 Arterial blood gases, 16, 25, 26 Arterial cannulation, 21, 25, 53 Arteriotomy, 23, 53, 60, 122, 124 Ascending aorta, 11, 27, 28, 37, 39–41, 57, 58, 83, 84 Aspirin, 16, 60, 138 Assisted venous drainage, 25–27, 91 Asthma, 16 Atelectatic lung, 18 Atracurium, 21 Atrial fibrillation, 10, 12, 16, 91 Atrial retractor, 11, 66–68, 73, 76, 77, 80, 87, 89–91, 98, 105, 106 Atrial septal defects (ASD), 2, 11, 12, 27, 28, 33, 43–45, 61–73, 80, 84, 86, 95 closure of, 61, 63–73 Atriotomy, 12, 67, 73, 78, 85, 86, 88, 92, 97, 102, 106, 107 Atrioventricular valve repair/replacement, 73–80 Atrium, 12, 23–25, 34, 35, 37–40, 42–46, 51, 53–57, 64, 66–69, 73, 76–78, 80, 83–86, 88–91, 98, 102, 106–108 Auscultation, 23 Autologous pericardial patch(s), 12, 66–69, 86 Awake intubation, 16 B Barlow’s disease, 34 Barotraumas, 16 Beating heart, 2, 11, 22–23, 27, 28, 67–71, 73, 86, 88, 90, 111–132, 136, 137 Bed-side assistant, 21 Benign tumors, 83 Beta-blockers, 16 Bispectral (BIS) analysis, 25 Blood drainage, 22, 27 Blood loss, 22 Blood pressure, 18–21, 23, 25, 28, 57, 112, 141 Body mass index, 17 Body position, 21 Brachial plexus injury, 21 Bradycardia, 21, 22 Brain protection, 25 Bronchial blocker, 17, 19, 21 Bronchodilators, 17 Bronchoscopy, 17, 18, 21, 23, 111 Bryce-Smith tube, 17 C CABG. See Coronary artery bypass graft (CABG) CAD. See Coronary artery disease (CAD) Calcified mitral annulus, 95 Camera, 4, 6, 7, 10, 61, 63, 77, 84, 91, 94, 96, 105, 112, 120, 121, 142 port, 10, 91, 112, 120 Cannulation, 12, 21, 24–26, 29, 33, 34, 37, 39–41, 46, 50, 51, 53–60, 62, 63, 73, 76, 83, 86, 91, 95, 96, 105 Capnograph, 17, 25 Carbon dioxide (CO2), 12, 16–25, 27, 28, 63, 67, 69, 77, 91, 97, 106, 112, 120, 127, 131, 132, 136, 142 absorption, 16, 18, 23, 25 insufflation, 16–21, 23, 24, 27, 112, 131, 142 PETCO2, 19, 24, 25 pneumothorax, 16, 17, 19, 21, 23 Cardiac function, 12, 19, 76 Cardiac index (CI), 19, 20, 23 Cardiac output (CO), 16, 19, 25, 131, 134 Cardiac tumors, 10, 83, 84 C. Gao (ed.), Robotic Cardiac Surgery, DOI 10.1007/978-94-007-7660-9, © Springer Science+Business Media Dordrecht 2014 147 148 Cardioplegia, 11, 25, 27–29, 57–60, 67, 84, 86, 87, 93, 94, 97, 102, 107 Cardiopulmonary bypass (CPB), 12, 16, 17, 21–28, 33, 34, 37–39, 41, 42, 44–46, 49–63, 67, 69–71, 73–75, 77, 84, 87–89, 91, 93, 95, 102, 104–107, 109, 111, 127, 131, 132, 136 Cardiotomy, 66 Cardiovascular function, 19 Cardiovascular surgery, 2, 10, 11, 13 Carlens, 17 Catheter, 17, 23–26, 28, 29, 51, 52, 54–59, 61, 62, 67, 68, 112, 118, 128, 130, 141 CPB (Cardiopulmonary bypass), 49–59 Central venous cannula, 16 Central venous catheter, 23, 25, 62 Chest x-ray, 16 Chitwood clamp, 11, 27, 57, 67, 106 Chitwood cross-clamp, 64, 65, 75, 77, 84, 91, 95, 97, 106, 107 Chordae, 34–36, 101–104 elongation, 34, 35 rupture, 34–36 Chronic obstructive pulmonary disease (COPD), 16, 17, 129, 137 CI. See Cardiac index (CI) Cisatracurium, 20 Clefts, 76–80, 91, 92, 100, 101, 104 Clopidogrel, 16, 138 Coagulopathy, 17, 137 Collapsed lung, 18, 19, 21, 24 Commissurotomy, 95 Communication, 7, 8, 10, 16, 22, 76, 78, 80 Comorbidity, 16, 17, 131 Complications, 12, 15, 21, 22, 25, 27, 28, 34, 60, 61, 68, 70, 74, 92, 104, 108, 127, 130, 131, 136, 137, 141, 4143–45 Computed tomographic scan, 16, 130 Computer-enhanced instruments, 2 Congenital heart diseases, 12, 43, 61–80 Congestive heart failure, 17 Console surgeon, 57, 69, 108, 122, 132 Continuous positive airway pressure (CPAP), 17, 18, 21, 24 Contraindications, 12, 16, 69, 105, 129, 137 Controller, 4, 6, 84 Conversions, 28, 70, 91, 109, 132 COPD. See Chronic obstructive pulmonary disease (COPD) Coronary artery bypass graft (CABG), 2, 10, 22–23, 71, 111, 116–129, 131, 135–140 Coronary artery disease (CAD), 97, 127, 135 Coronary revascularization, 2, 10, 11, 126–131, 135–144 Coronary sinus, 12, 25, 28, 29, 43, 78–80, 141, 144 Coronary surgery, 11, 111, 131 Coronary syndromes, 119, 138 Cosmetics, 12, 70, 76, 80, 88, 90, 104, 118, 127, 131, 136, 144 Cox-Maze, 12 CPAP. See Continuous positive airway pressure (CPAP) CPB. See Cardiopulmonary bypass (CPB) Cross-clamp time, 11, 69–71, 74, 75, 88, 89, 104, 109 D da Vinci, 2, 4, 8–11, 15, 75, 77, 88, 91, 94, 98, 100, 102, 105, 109, 115, 122, 127, 131 (Si) surgical system, 2–8, 11, 15–17, 22–25, 29, 64, 70, 74, 77, 84, 88, 89, 94, 102, 105, 108, 132, 141 3D computed tomography angiography (CTA), 50 Defibrillation thresholds, 22 Degrees of freedom, 2, 4, 71, 94, 131 Index Dependent lung, 18, 19, 24 Depth of anesthesia, 25 Desaturation, 18, 26, 129, 137 Desflurane, 19, 21 De Vaga technique, 66, 67 Dexedetomidine, 20 Diazepam, 20 Difficult airway, 16 Direct-vision approach, 28, 37, 93–94, 109 Double-lumen endotracheal intubation, 34, 51, 62, 120, 141 Double-lumen endotracheal tube, 17, 18, 20, 23, 24, 111 Double-lumen intubation, 111, 120, 141 Double lumen tube, 16, 21, 105 dP/dt, 20 Droperidol, 20 E Echocardiograms, 104–105 Echocardiographic (ECHO) examination, 16, 44, 49–50, 91, 108 Elecocautery, 4, 22 Electrocardiogram (ECG), 23, 25, 78 Electrocautery, 4, 22 Electrolytes, 16 Emphysematous bullae, 16 Emphysematous chest, 16 Endoaortic balloon, 25, 27, 28, 91 Endoaortic occlusion, 11, 25 Endoscope, 2, 8, 61, 70, 112, 131 Endoscopic ITAs harvest, 115 Endoscopic trocar, 9, 63, 95 Endostabilizer, 122, 132 Endowrist, 5, 11, 97, 123, 132 Etomidate, 20 Event-free survival, 111 Excision, 12, 45, 83–92 External defibrillator pads, 22, 112 External defibrillator patche, 62, 95, 112, 120, 141 Extracorporeal, 27, 65, 87, 102, 107 Extubation, 20–23 F Fast track, 20–23, 25 anesthesia, 21, 22 Femoral arterial cannula, 25 Femoral artery, 27, 50–54, 60, 67, 95, 96 Femoral-femoral bypass, 21, 25, 84 Femoral vein, 26, 39, 50, 51, 53–55, 60, 86, 95 Femoral venous cannula (FVC), 26, 39, 58 Fentanyl, 19, 20 Fiberoptic bronchoscope, 17, 18, 21 Fibroelastic deficiency, 34 FiO2, 19, 24 Fogarty catheter, 17 Fossa ovalis, 45, 88 Functional residual capacity (FRC), 18 FVC. See Femoral venous cannula (FVC) G Gas exchange, 16, 24 General anesthesia, 18, 25, 51, 76, 91 Gore-Tex running suture, 66, 67 Guidance of cannula, 21 Index H Half-life, 20, 137 Halothane, 19 Harvesting time, 115–117, 126 Heart rate (HR), 16, 20, 23 Hemodilution, 24, 25 Hemodynamic(s), 12, 16, 19–21, 23, 34, 36–37, 41, 69, 87, 102, 120, 129, 131, 132, 136–138, 141–143 compromise, 16, 19, 132, 137 stability, 22 Heparization, 26 High airway pressures, 19 High frequency jet ventilation, 18 High-frequency positive pressure ventilation, 19 Hospital stay, 2, 22, 29, 61, 68, 74, 90, 104, 119 HPV. See Hypoxic pulmonary vasoconstriction (HPV) HR. See Heart rate (HR) Hybrid coronary revascularization, 11, 127–129, 135–140 Hybrid procedure, 16, 129 Hybrid revascularization, 128, 130, 137 Hypercapnia, 16, 18, 19, 23 Hypertension, 17, 69, 129, 137 Hypnotics, 19, 20 Hypoglycemic medications, 16 Hypotension, 23 Hypothermia, 19, 21, 24 Hypothermic CPB, 24, 28, 67, 94 Hypoxemia, 112 Hypoxia, 19, 132 Hypoxic pulmonary vasoconstriction (HPV), 18, 19, 24 I ICS. See Intercostal space (ICS) ICU. See Intensive care unit (ICU) Incisions, 1–3, 7, 9, 11, 15, 22, 27, 33, 43, 45, 51, 52, 55, 58, 60–63, 70, 73–77, 80, 84, 88–91, 93–96, 105, 107, 108, 111, 112, 116, 118–120, 123, 125, 129, 131, 132, 136, 142–144 Induced tension pneumothorax, 16 Induction, 16, 20–21, 23, 25, 34, 61, 111, 120, 141 Inferior vena cava (IVC), 21, 25, 37, 39, 63, 65, 66, 73, 89 Inflammatory response, 17, 22, 136 Inhalation agents, 19 Instruments, 1, 2, 4–13, 22, 25, 61, 63, 71, 77, 88, 91, 94, 95, 98, 101, 103, 105, 110, 112, 113, 120, 121, 132, 142 Insulin, 16 Intensive care unit (ICU), 20–22, 69, 70, 87, 102, 127, 143 Intercostal space (ICS), 9, 39, 57, 58, 63, 95, 97, 116, 120, 131, 142 Internal jugular vein, 23, 34, 39, 49, 51, 55, 56, 58, 60, 62, 63, 95 Internal thoracic artery (ITA), 111, 128 Interventional cardiologists, 61, 129, 137, 140 Intra-aortic balloon occlusion device, 25 Intracardiac mass, 45 Intracoronary shunts, 22, 23 Intrapleural CO2 insufflation, 18, 19, 23 Intrapleural pressure, 16, 19 Intrapulmonary shunt, 18, 19, 24 Intrathoracic CO2 pressure, 19 Intrathoracic pressure, 12, 19, 23 Intravenous anesthesia, 19 Intubation, 16, 20, 23, 34, 51, 62, 76, 91, 111, 120, 141 Intuitive surgical system, 11 Ischemia, 21, 23, 24, 68, 130, 132, 136, 138 Ischemic preconditioning, 22, 132 149 Isoflurane, 19, 21 ITA. See Internal thoracic artery (ITA) IVC. See Inferior vena cava (IVC) K Ketamine, 20 Kinetic-assisted venous drainage (KAVD), 27 L LAD. See Left anterior descending artery (LAD) Laparoscopic surgery, 2, 3 Laryngoscopy, 20 Lateral decubitus position, 18, 19, 21 Leaflet billowing, 34, 35 Leaflet prolapse, 23, 34, 35, 98 Learning curves, 2, 60, 69–71, 74–76, 88, 89, 102–105, 108–110, 115–118, 126–127, 131, 132, 136 Left anterior descending (LAD) artery, 11, 23, 116–120, 122–124, 127–132, 135–139 Left atrial roof, 88 Left atrial tumor, 85, 89 Left internal mammary artery (LIMA), 11, 22, 132, 136, 137, 139, 140 Left ventricular ejection fraction (LVEF), 17 Left ventricular epicardial lead placement, 142 Left ventricular stroke work index (LVSWI), 20 Less-invasive, 12 Lidocaine, 19, 123 LIMA. See Left internal mammary artery (LIMA) Lorazepam, 20 Lung capacity, 18 Lung injury, 18, 19 LVEF. See Left ventricular ejection fraction (LVEF) LVSWI. See Left ventricular stroke work index (LVSWI) M Magnesium, 16 Maintenance of anesthesia, 16, 20–21 MAL. See Midaxillary line (MAL) MCL. See Midclavicular line (MCL) Mean arterial pressure (MBP), 19 Mechanical ventilation, 18, 20, 69, 75, 88 Median sternotomy, 10–12, 23, 28, 33, 37, 61, 70, 75, 83, 90, 93, 94, 135, 136 Microemboli, 27, 68 Microincision, 11, 94 Midaxillary line (MAL), 64, 73, 77, 84, 91, 95, 106, 142 Midazolam, 20, 21 MIDCAB. See Minimally invasive direct coronary artery bypass (MIDCAB) Midclavicular line (MCL), 9, 63, 95, 105, 112, 122 Mini-incision, 93–94 Mini-incision mitral valve surgery (MIMVS), 93 Minimally invasive cardiac surgery, 27, 28, 33, 93, 108, 137 Minimally invasive coronary artery bypass grafting, 22, 128, 135, 136 Minimally invasive direct coronary artery bypass (MIDCAB), 11, 16, 22, 115–118, 120, 131, 132 Minimally invasive surgery, 1, 2, 13, 15, 22 Minithoracotomy, 11, 22, 93, 94, 126, 131, 132, 136 Minute ventilation, 19 Mitral insufficiency, 23, 95Mitral prolapse, 36, 44 Mitral regurgitation, 94, 104 150 Mitral stenosis (MS), 23, 34, 41, 109 Mitral valve, 2, 10, 23, 24, 35, 38, 41–44, 76–80, 88, 92–94, 97, 98, 100, 101, 104–106, 108 plasty, 91–92 repair, 2, 11, 16, 21, 23, 29, 61, 71, 80, 88, 89, 92, 94–96, 98, 102, 105, 108, 131 surgery, 11, 12, 17, 23–25, 33–43, 93–110 Monitoring, 16, 23, 25, 69, 112, 141 Mortality, 12, 21, 61, 70, 93, 110, 131, 136, 141 Multivessel CAD, 127 Muscle relaxants, 20, 21 Myocardial irritability, 16 Myocardial ischemia, 21, 23 Myocardial preservation, 33 Myocardial protection, 27, 33, 60 Myocardial stabilizer, 22 Myxoma, 2, 12, 16, 45, 46, 83–92 N Near-infrared spectral analysis, 25 Neochord insertion, 104 Neoplasms, 83 Neuromuscular blocker/blockade, 18, 21 Nifedipine, 19 Nitric oxide, 18 Nitroglycerin, 23 Nitroprusside, 19 Nondependent lung, 18, 19 Norepinephrine, 23 NYHA class, 17, 76 O Off-pump CABG, 136, 138 One-lung ventilation (OLV), 16–25, 105 On pump, 11, 28, 69, 136, 139 Operation time, 69, 70, 74, 75, 88, 89, 104, 109, 110, 126 Opioids, 20, 21 Ostium primum defect, 12, 76–80 Oxygenation, 18, 19, 23, 24, 136 P PA catheters. See pulmonary artery (PA) catheters Pancuronium, 20, 21 PAP. See Pulmonary arterial pressures (PAP) Paravalvular regurgitation, 42–44 Partial anomalous pulmonary venous connection, 11 Partial atrioventricular septal defect, 76–80 Partial sternotomy, 84, 93 Patency, 17, 23, 111, 118, 127, 130–132, 136–138, 140 Patent ductus arteriosus, 11 Patient cart, 4, 6–10 position, 9, 22, 62–63, 73, 84, 95, 105, 111–112, 119, 141–142 selection, 16–17, 45, 95, 126, 129–131, 137 Patient-side surgeon, 9, 63, 66, 73, 95, 101, 105, 107, 108, 112, 142, 143 PCI. See Percutaneous coronary intervention (PCI) PCWP, 25 Peak airway pressure, 21 Peak inspiratory pressure, 18 Index PEEP. See Positive end expiratory pressure (PEEP) Percutaneous catheter techniques, 61 Percutaneous coronary intervention (PCI), 11, 127, 129, 130, 135–140 Perfusionist, 22, 28, 57 Pericardiotomy, 63, 73, 121–123 Pericardium stay suture, 63, 64, 73, 95 Peripheral cardiopulmonary bypass, 16, 21, 25–27, 49–61 Peripheral vessels, 37, 50 Permissive hypercapnia, 19 Phenylephrine, 23 Phrenic nerve, 63, 64, 73, 84, 95, 116, 141, 142 Physiotherapy, 17 Pipecuronium, 20, 21 Platelet-inhibition, 137, 138, 140 Pleural cavity, 19, 114, 116 Pneumothorax, 12, 16–19, 21–23, 25, 136 Polytetrafluoroethylen, 11, 73, 86, 92, 107 Port-access, 61, 84, 93 Positive end expiratory pressure (PEEP), 18, 24, 31 Postoperative analgesic, 22, 23 Postoperative course, 22, 78, 92, 111 Postoperative management, 69, 87–88, 102, 143 Postoperative period, 22 Potassium, 16 Pregnancy, 19 Preload, 19, 23, 41 Preoperative evaluation, 16, 49 Pre-operative preparation, 49–50 Preoperative visit, 16 Primary cardiac tumors, 83 Propofol, 19–22 Protamine, 24, 58, 123, 137–139 Pulmonary artery occluded pressure (PAOP), 20 Pulmonary arterial pressures (PAP), 19–21, 23, 25 Pulmonary artery (PA) catheter, 23, 25, 112, 141 Pulmonary compliance, 18, 136 Pulmonary function, 16, 17, 130 Pulmonary vascular resistance (PVR), 16, 19, 20, 73 Pulmonary veins, 27, 36, 44, 64, 65, 73, 85, 88, 90, 97, 98 Pulse oximetry, 25 PUMA, 2 PVR. See Pulmonary vascular resistance (PVR) Q Quadrangular resection, 11, 98, 104 R Radial arterial cannula, 25 RAP. See Right atrial pressure (RAP) Real-time 3D transesophageal echocardiography, 34 Recurrence, 12, 75, 87, 88, 90, 118 Regurgitation, 36, 41–44, 58, 66, 69, 73, 76, 77, 88, 91, 94, 98, 103, 104, 109 Reinflate lung, 18 Reintubation, 21 Remifentanil, 20 Remote access perfusion, 28, 69, 90 Respiratory rate, 19, 24 Retrograde cardioplegia cannula position, 25 Revascularization, 2, 10, 11, 22, 23, 111, 118, 126–131, 135–144 Index Right atrial pressure (RAP), 20 Right atrium, 24, 34, 35, 37–40, 45, 46, 51, 53–55, 66–68, 73, 76–78, 80, 83, 86, 88 Right groin incision, 51, 62, 76, 91 Right internal jugular vein (RIJV), 23, 25–28, 34, 39, 49, 55, 56, 58, 60, 62, 63, 95 Right internal thoracic artery (RITA), 113–119, 123, 125 Right-to-left transpulmonary shunt, 18 RIJV. See Right internal jugular vein (RIJV) RITA. See Right internal thoracic artery (RITA) Robertshaw, 17 Robot, 2, 11–13, 21, 22, 75, 84, 88, 94, 105 Robotic assisted CABG, 22–23 Robotic assisted endoscopic minimal invasive coronary artery bypass (MIDCAB), 11, 16, 22, 115–118, 120, 131, 132 Robotic coronary bypass graft, 10, 111–132, 137, 140 Robotic instruments, 6, 11, 22, 25, 73, 94, 95, 101, 105 Robotic mitral valve placement, 105–110 Robotic mitral valve plasty, 104, 105 Robotic mitral valve repair, 11, 23, 29, 94–96, 105 Robotic surgical system, 3, 61, 71, 80 Robotic technique, 3, 11, 13, 17, 29, 110, 131 Rocuronium, 20, 21 Running sutures, 60, 66–68, 73, 78, 80, 86, 87, 92, 98, 99, 101, 102, 107, 132 S SaddleLoop, 122–125 Same-session revascularization, 139–140 Seldinger, 25, 26, 53–56, 62, 76, 91 Sevoflurane, 19, 21, 29 Shunt, 18, 19, 22–24, 44, 45, 74, 75 Single-lumen endotracheal tube, 17, 18, 20, 23, 24, 111 Single lumen tube, 17, 21 Single lung ventilation, 15, 29, 62, 69, 76, 91, 95, 104, 111, 112, 119, 129, 132, 136, 137 Smoking, 17 Standard procedures, 49 Stereo viewer, 4, 5 Sternotomy, 4, 5 Steroids, 17 Stroke volume (SV), 19, 20 ST-segment monitoring, 25 Subendocardial defects, 86 Submammary, 84 Subvalvular apparatus, 36, 95, 101, 108, 109 Succinylcholine, 20 Sufentanil, 20, 23 Superior pulmonary vein, 65, 97 Superior vena cava (SVC), 21, 24–26, 37, 39, 40, 44–46, 50, 53, 55, 56, 60, 63–65, 67, 68, 73, 89, 97, 98, 106 Surgical console, 4 Surgical team, 16, 21, 22, 127 Suturing, 12, 13, 60, 86, 105, 127, 131, 132, 144 SVC. See Superior vena cava (SVC) SVR. See Systemic vascular resistance (SVR) Systemic embolism, 89 Systemic heparinization, 26, 53, 62, 116, 122, 123 Systemic vascular resistance (SVR), 20, 21 Systolic anterior motion, 41 151 T Tachycardia, 19, 21, 23, 91 TECAB. See Totally endoscopic coronary artery bypass (TECAB) TEE. See Transesophageal echocardiography (TEE) Therapeutic, 34, 83, 93 Thoracic epidural anesthesia, 19 Thoracoscopic surgery, 3, 12 Thoracoscopy, 3, 12, 19, 21, 69, 104, 116, 131, 136, 137, 141 Thoracotomy, 11, 12, 22, 61, 70, 76, 94, 95, 116, 136, 137, 141 incision, 22, 116 Three-dimensional visualization, 4, 61, 94, 115 Tidal volume, 18, 19, 24 Totally endoscopic coronary artery bypass (TECAB), 2, 11, 15–17, 22, 115, 116, 118–129, 131, 132, 135–137, 139 Totally endoscopic procedures, 61, 128 Totally robotic cardiovascular surgical procedures, 11 Totally robotic coronary bypass on beating heart (BH-TECAB), 115 Transesophageal echocardiography (TEE), 16, 18, 21, 23–29, 33–46, 51, 53, 55–59, 62, 63, 69, 70, 74, 76, 77, 87, 91, 95, 102, 103, 105–107 Transthoracic aortic clamp, 27, 94 Transthoracic chitwood clamp, 11 Transthoracic echocardiography, 69, 88, 102 Transthoracic electrical impedance (TTI), 22 Transvenous, 12, 141, 143 Trapezoidal resection, 98 Trauma, 15, 27, 61, 70, 80, 91, 111, 131, 141, 144 Tricuspid valve, 11, 16, 66–69, 73, 74, 76, 79, 86 Tricuspid valve plasty, 66, 67, 69 Trigone, 98, 99 Trocar, 9, 18, 63, 88, 95, 105, 142 TTI. See Transthoracic electrical impedance (TTI) Tumors, 10, 12, 45, 46, 83–91 Two-lung ventilation, 18, 22, 24 Tying knots, 66, 73, 87, 102 U U-clip, 11, 22, 98–101, 122–124, 132 Univent tube, 17, 21 Urine output, 25 V Vacuum-assisted venous drainage (VAVD), 27 Vascular injuries, 25 Vasodilator, 19, 21 VAVD. See Vacuum-assisted venous drainage (VAVD) Vecuronium, 20, 21 Venous cannulae, 21, 25, 27 Venous cannula position, 25, 27, 53 Venous drainage cannula, 26, 62 Ventilated lung, 18, 19, 24 Ventilation, 16–20, 23–25, 27, 69, 70, 75, 76, 88, 91, 111, 119, 120, 129, 132, 136, 137, 141 Ventilation-perfusion distribution, 16 Ventilation-perfusion relationship, 18 Ventilation to perfusion ratio (V/Q), 18 Ventilatory defects, 19 Ventricular fibrillation (VF), 22, 23, 28, 44, 84, 94, 141, 143 152 Ventricular septal defects, 2, 12, 73–78, 80 repair, 2, 12, 73–78, 80 Video-assisted procedure, 93, 94, 141 Video-directed instruments, 94 Vision cart, 4–7, 9 Visualization, 1, 4, 12, 23, 27, 33, 37, 44, 61, 68, 73, 76, 80, 94, 95, 110–112, 136, 144 V/Q mismatch, 18 Index W Working port, 9, 57, 63, 66, 68, 77, 87, 88, 91, 95, 96, 102, 105, 107, 108, 142 Z ZEUS surgical system, 3