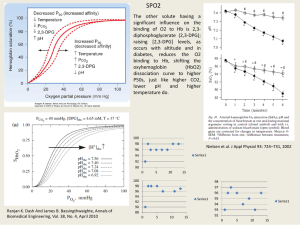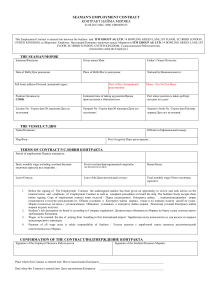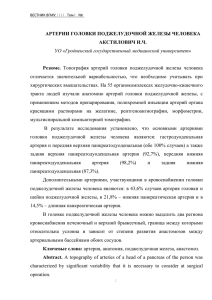
2.4 198 Isolated Vessels Rudolf Schubert Introduction Blood vessels play an important role in the regulation of blood pressure and blood flow distribution. In order to understand the mechanisms of these regulatory processes in health and disease, the in vivo behaviour of vessels and their interaction in vessel networks has to be known. However, under in vivo conditions, vessel responses depend on a complicated interaction between the different cell types of the vessel wall (smooth muscle cells, endothelial cells and various cells in the adventitia), factors released from nerve endings, metabolites originating from the surrounding tissue, hormones transported by the blood flow, mechanical factors like shear stress and transmural pressure and also the behaviour of proximal and distal vessel segments. The complexity of this system quite substantially limits the possibility of interpretation of experimental findings in mechanistic terms. Therefore, in vitro methods for the investigation of blood vessel function have been introduced, where many of these confounding factors can be controlled. The first experiments performed to study the function of blood vessels employed large vessels. However, recent technical developments also allow experiments to be conducted on small arteries, arterioles and small veins from various vascular beds. In practice, vessel segments with a diameter in the range from about 20 µm to several millimeters and a length of about 0.1–10 mm are used. These vessel segments consist of endothelial cells in the tunica intima, smooth muscle cells in the tunica media and nerve endings, fat cells, fibroblasts etc. in the tunica adventitia. Investigations into the functioning of these vessel segments, i.e. of their reactions to the application of external stimuli such as vasoactive substances, pressure, etc., employ several different methods. In the past, spiral strip preparations were used. Since this procedure results in a relatively large number of damaged smooth muscle and endothelial cells and in disruption of the normal vascular architecture, the use of cylindrical vessel segments is now preferred. Two methods for the investigation of vessel segments have been developed. One method employs ring vessel segments threaded on to two hooks or wires and the other cannulated vessel segments fixed on two pipettes. In this chapter an overview of these two methods will be given. Isolated Vessels 199 Description of Methods and Practical Approach Solutions In in vitro experiments, vessels are studied after isolation from their normal environment. In order to simulate this environment, physiological saline solution is used and experiments are conducted at 37 °C. Here are some examples for the composition of the physiological saline solution reported in the literature (in mM): ▬ 120 NaCl, 4.5 KCl, 1.2 NaH2PO4, 1 MgSO4, 1.6 CaCl2, 0.025 EDTA, 5.5 Glucose, 26 NaHCO3, 5 HEPES, pH 7.4. ▬ 145 NaCl, 4.7 KCl, 1.2 NaH2PO4, 1.2 MgSO4, 2 CaCl2, 0.02 EDTA, 5 Glucose, 2 Pyruvate, 18 NaHCO3, pH 7.4. ▬ 145 NaCl, 4.7 KCl, 1.2 NaH2PO4, 1.17 MgSO4, 1.5 CaCl2, 0.02 EDTA, 5 Glucose, 2 Pyruvate, 3 MOPS, pH 7.4. Obviously, there are differences in the compositions of the solutions used, but how critical are they? The differences are smallest and most of them of only minor importance in the cases of the contents of Na+, H2PO4–, SO2–, HCO3–, Cl–, Mg2+, EDTA (used to chelate trace amounts of heavy metal ions), pyruvate and glucose. The same is true for K+, but one should have in mind that addition or removal of just a few mM of K+ has profound effects on the activity of the Na+/K+-pump and the activity of inward rectifier potassium channels, which have a considerable impact on the contractile state of small arteries (Zaritsky et al. 2000). Ca2+ is an important ion, because it plays a central role in the molecular mechanism of contraction. The concentration of free calcium in blood plasma is around 1.5 mM. Therefore, a calcium concentration in this range should be used to simulate physiological conditions in the experimental solution. H+ is another important ion, especially for small arteries and arterioles, where small changes in pH induce considerable changes in diameter. The solution should therefore contain a pH-buffer. Often, NaHCO3 is used as buffer, since this is the main physiological pH buffer in plasma. The protons and the bicarbonate ions establish equilibrium with CO2 in the solution giving a PCO2 of about 35 mmHg. However, CO2 leaves the solution into the surrounding air, where the CO2 content is virtually zero. Thus, in order to stabilise the equilibrium, i.e. to control PCO2 and pH, solutions containing a bicarbonate buffer are commonly bubbled with carbogen, a gas mixture of 95% O2 and 5% CO2. Sometimes, an artificial pH buffer like HEPES is added in an attempt to further stabilise the pH. It should be mentioned however, that the use of carbogen will produce a PO2 in the range of 400–500 mmHg. This is an unphysiologically high value, which might be justified in large arteries in order to get a normal PO2 deep inside the thick vessel wall. However, it should be taken into account that O2 affects vessel contractility directly. Thus, at least when studying small vessels, it is better to use a gas mixture of 75% N2, 20% O2 and 5% CO2. Sometimes the problems with the bicarbonate buffer have been avoided by using solutions without NaHCO3, where only artificial pH buffers like HEPES or MOPS are used (see solution 3 above). Due to equilibration with the surrounding air, a PO2 of 2.4 2 200 Isolated Organs about 150 mmHg is achieved, which is still somewhat higher than physiological values. However, the PCO2 is unphysiologically low under these conditions, which should be remembered in experiments on vessels sensitive to PCO2. In-Vitro Techniques Vessel Isolation An important issue for a successful experiment is the isolation of the vessel segments. Experiments on small vessels require an especially careful vessel preparation. Direct contact of the isolation instruments with the vessel and stretching of the vessel, especially in the longitudinal direction, should be avoided. In order to prevent hand tremor, special supports for the arms are helpful. Isolation of the vessels should be done with appropriate instruments. Often, fine forceps (Dumont No 5) and small scissors are used [for a very detailed discussion of practical aspects of the isolation procedure for small vessels see Duling et al. (1981)]. The isolation can be done in one of the solutions described above. If the solution contains NaHCO3, the solution has to be gassed in order to ensure a physiological pH. Otherwise the pH will increase, which leads to contraction, particularly of small arteries. Such contracted vessels are very difficult to mount on the myograph (for mounting procedures see next paragraph) and are consequently prone to excessive damage. Since bubbling of the solution in the isolation chamber results in bad visibility, solutions without NaHCO3 are often used. In addition, in order to prevent damage to the vessels, the solution used for vessel isolation may be kept at low temperature and may contain only a low calcium concentration. Thus, under appropriate conditions, the function of the smooth muscle cells as well as of the endothelium can be preserved in isolated, in vitro vessel preparations. It is common practice, and often even necessary for methodological reasons, for the adventitia to be more or less completely removed from the vessels. However, it should not be forgotten that the adventitia is an integral part of the vessel wall. Indeed, it has been shown that complete, careful removal of the adventitia without media damage leads to changes in some contractile and relaxant responses (Gonzalez et al. 2001). Vessel Mounting Ring Vessel Segments This method is the classical, older approach, where ring segments are held on two hooks or similar devices or, in the case of resistance vessels, on two wires passed through their lumen (Bevan and Osher 1972; Mulvany and Halpern 1976, 1977; Mulvany et al. 1978). One of the hooks or wires is connected to a force transducer allowing wall force to be measured. These preparations can be investigated under isotonic conditions by adjusting the circumference during changes in activation in order to achieve a constant force (for example see Nilsson and Sjoblom 1985; Boels et al. 1990; Boonen and Demey 1994). In most cases, however, these preparations are used under isometric conditions, where the vessel circumference stays constant and Isolated Vessels 201 changes in force during changes in activation are determined. The diameters of the hooks and wires have to be adapted to the diameter of the vessel under study in order not to damage the vessel due to undue stretching when inserting two hooks or wires into the vessel lumen. The use of wires as small as 14 µm has been reported (Bukoski et al. 2001). Nevertheless, there is a lower limit for the vessel diameter suitable for experiments on ring vessel segments. In addition, if tungsten wire is used, it has been observed that aged tungsten wire may undergo spontaneous surface oxidation, which resulted in altered vessel relaxant responses. Thus, it was concluded that gold or tungsten-free stainless steel wire should be used (Bukoski et al. 2001). At the beginning of an experiment with ring vessel segments, the initial stretch, or preload, of the vessel has to be set in order to simulate its in vivo conditions. This procedure is important, because many vessel responses depend on the amount of initial stretch. Thus, noradrenaline sensitivity increased with increased stretch (Price et al. 1981; Nilsson and Sjoblom 1985). The maximum constriction to noradrenaline and to several other vasoconstrictors increased with increasing stretch and then decreased with further stretching resulting in a bell-shaped diameter–tension relationship (Nilsson and Sjoblom 1985; Boonen and Demey 1994). However, these diameter–tension relationships were different for different agonist and for different vessels (Boonen and Demey 1994). In addition, acetylcholine-induced membrane potential hyperpolarisation was larger in stretched compared to unstretched preparations and this difference was suggested to reflect the involvement of additional mechanisms (NO, PGI2) in the stretched preparation (Parkington et al. 1993). The procedure of setting the initial stretch is known as “normalisation”, because it allows the comparison of data from different vessels. To apply stretch to the vessel segment, the second hook or wire is connected to a micrometer. Thus, the distance between the hooks or wires, i.e. the vessel circumference, can be increased. A critical evaluation of common normalisation procedures by Halpern (Halpern 1991; Halpern and Kelley 1991) showed that some of them (stretch to a just detectable force, to a fixed force or to the in situ circumference) are not appropriate. Often an initial stretch is selected, where the maximum of the active response to some agonist is achieved. This requires that the passive and the active force–circumference relationships be determined experimentally for the particular vessel and agonist desired. In practice, these data are available for a number of vessels and agonists in the literature. If documented in appropriate detail in order to understand how the values were obtained, one can use values of initial stretch reported previously. However, it should be taken into account that in many cases the maximum active response is achieved when the initial stretch, i.e. passive force, of the vessel is of the same order of magnitude as the total force. Hence, active force, the difference between total and passive force, is small and may be difficult to determine accurately. Thus, in many experiments a circumference 10 or 20% smaller than that at the maximum of the active response is used. Under these conditions the maximum active force is only slightly smaller but the passive force is considerably smaller compared to the situation at maximum active force, due to the steep exponential passive force-circumference relationship. Alternatively, an initial stretch corresponding to the in vivo pressure of the vessel (calculated using the La place relationship and the known circumference and passive stretch) may be chosen. 2.4 In-Vitro Techniques 2 202 Isolated Organs After the normalisation procedure, the performance of a viability test is recommended. Usually this includes 2–3 applications of an agonist at high concentration, sometimes combined with the addition of a high (120 mM) potassium solution. This procedure is necessary in order to observe stable contractile vessel responses after the vessel isolation and mounting procedure. However, the application of high agonist concentrations gives only first, rough information about the viability of the preparation. In addition, an agonist concentration about 100 times smaller than the saturating concentration should be tested. On top of this contraction an agonist able to activate the endothelium such as acetylcholine can be added in order to test the viability of the endothelium. In principle, a judgement about the viability of a vessel requires knowledge of the “normal” responses of the particular vessel under investigation. The level of these responses can be determined only experimentally. It is either already known from previous studies or, in the case of a not well-characterised vessel, has to be found during the course of a certain number of preliminary experiments on that vessel. The investigation of ring vessel segments is performed most often using fixed supports for the hooks or wires, i.e. under isometric conditions. Vessel responses, i.e. levels of activation of the smooth muscle cells, are represented as changes in force (usually given in mN). However, in order to be able to compare responses of vessels with different lengths, wall tension, i.e. force per wall per unit of vessel length (T = F/2L, where T is tension, F is force and L is vessel length, given in mN/mm) is used. In addition, in order to be able to compare responses of vessels of different thicknesses, wall stress (σ = T/w, where σ is wall stress, T is tension and w is wall thickness, given in mN/mm2) is employed. The latter requires the determination of vessel wall thickness. This can be done by microscopic observation of the vessel wall at the site of the hook or the wire using a calibrated eyepiece. It should be taken into account, however, that in this place the vessel wall is somewhat thinner than the upper and lower part of the vessel wall. This will result in a certain overestimation of wall stress. Cannulated Vessel Segments This method is a newer approach, in which vessel segments are fitted on to two cannulas and fixed using appropriate sutures (see inset in Fig. 1). The construction of the cannulas depends on the size of the vessel to be investigated. In most cases the outer diameter of the cannulas should be slightly smaller than the inner diameter of the isolated vessel, i.e. of the vessel without the distending influence of transmural pressure. Vessels down to a diameter of about 60–80 µm can be mounted on simple pipettes pulled from polyethylene tubing or from glass capillaries using a special micropipette puller (Halpern et al. 1984). Using these pipettes, the vessel is simply slipped on using fine forceps and secured by suture (see also inset in Fig. 1). For smaller vessels a double-barrel pipette system has proven useful (see Duling et al. 1981 for construction details). This is however difficult to prepare and to handle and has a high flow resistance in perfusion experiments. Mounting of the vessel is performed by pulling the vessel into the holding pipette by applying reduced pressure to the lumen of this pipette. Then a perfusion pipette is advanced into the lumen of the vessel, so that the vessel is fixed between the perfusion pipette and a constriction of the hold- Isolated Vessels 203 Figure 1 Cannulated vessel segments. An experiment on a rat skeletal muscle small artery (see inset) is presented showing the viability test with the development of a spontaneous myogenic tone and the application of noradrenaline (NA) at 10–7 M and, after washout, of a bolus of acetylcholine (Ach) at 10–6 M in a and the vessel response to different levels of transmural pressure in b. For more details refer to the text ing pipette. An alternative double-barrelled pipette system consisting of two concentric micropipettes has been described by VanBavel et al. (1990) for small vessels with low flow resistance. One end of the vessel is sucked into the inner pipette and is held in place by applying sub-atmospheric pressure on the outer pipette. The inner pipette serves to apply pressure and flow to the vessel segment. Another method allowing physiological flows to be investigated and ensuring that the pressure drop across the cannula is much smaller than that over the vessel was developed by Hoogerwerf et al. (1992). Here the outer surface of a vessel is glued with fibrin glue to the inner side of a glass cannula with the aid of a smaller inner cannula, which is removed completely after the vessel is fixed. 2.4 In-Vitro Techniques 2 204 Isolated Organs For mounting, vessels are first secured on one cannula using appropriate sutures as mentioned in the previous paragraph. Then the vessel is flushed with saline to remove remaining blood. During this procedure the pressure applied should be low in order not to damage the vessel. Subsequently, the second end of the vessel is fixed on the second cannula. One of the cannulas is connected to either a reservoir, which can be elevated to a selected height, or a special pump producing the desired pressure. The other cannula can simply be closed in experiments without flow through the vessel lumen, or is connected to another reservoir or pump in experiments with flow. If nonflow conditions are selected, this condition should be controlled carefully during the course of the whole experiment. After mounting, cannulated vessel segments are often subjected to a desired pressure in order to simulate in vivo conditions, a procedure similar to setting initial stretch in ring vessel segments. This leads to an increase in the length of the vessel (see for example Lew and Angus 1992), observed as a buckling of the vessel mounted between two fixed cannulas. Usually this buckle is removed by simply adjusting one of the cannulas connected to a micrometer. However, longitudinal stretch in situ has been shown to produce depolarisation in endothelium denuded preparations and depolarisation followed by hyperpolarisation at higher axial stretch in endotheliumintact preparations and to affect noradrenaline-evoked contractions (Monos et al. 1993, 2001). Therefore, longitudinal stretch may by an important parameter, which should be controlled for in experiments on cannulated vessel segments. Indeed, a study investigating the influence of longitudinal stretch on the contractile and relaxant responses of several small arteries in vitro showed that in some, but not all, vessels, responses to noradrenaline were optimised at longitudinal stretches larger than 20% (Coats and Hillier 1999). However, this was not observed for some other contractile agonists. Thus, if the effect of longitudinal stretch on the vessel response studied is unknown, it should be determined in preliminary experiments. After pressurisation a viability test is recommended. This is of special importance for cannulated vessel segments, especially from resistance vessels, because pressureinduced vessel reactions have been shown to be especially sensitive to inappropriate handling during the vessel isolation procedure. The first indicator of viability is the development of a spontaneous myogenic tone after the pressure is increased and the temperature reaches 37 °C. In addition, the viability of the vessel, i.e. the reactivity to contractile and relaxing agents, including those acting via the endothelium, should be assessed (for an example see Fig. 1a). A judgement about the viability of a vessel requires knowledge of the “normal” responses of the particular vessel under investigation. These responses can be determined only experimentally. It is either already known from previous studies or, in the case of a not well-characterised vessel, has to be found during the course of a certain number of preliminary experiments on that vessel. Responses of cannulated vessel segments are sometimes represented as changes in perfusion pressure during constant flow perfusion or as changes in perfusate flow rate during constant pressure perfusion (see as an example Machkov et al. 1998). However, in the majority of studies, responses of cannulated vessel segments are represented as diameter changes. These are best measured using optical techniques. This requires a microscope and appropriate tissue illumination in order to achieve an optimal visu- Isolated Vessels 205 alisation of the vessel for precise diameter measurements. For large vessels (>400 µm), only the outer diameter can be determined, because the tissue is not transparent enough to find the inner edge of the vessel wall. For smaller vessels outer and inner diameter can be measured. In this case, inner, i.e. lumen diameter is the preferred readout, because this is the variable determining flow. Diameter can be measured manually by a micrometer eyepiece, an image splitting device or video scan lines. However, automatic methods based on video systems are more convenient (Halpern et al. 1984; Halpern 1991). These days, the vessel image is usually captured by a video camera attached to the microscope and presented on the computer monitor using a frame grabber card. There, special programs analyse the contrast profile produced by the vessel and find the outer and the inner diameter of the vessel using edge detection or pattern recognition algorithms (for example see Fischer et al. 1996 and references therein). Thus, an automatic tracking of vessel diameter changes is possible. Interaction from the user is only required when inner diameter changes need to be followed during strong contractions, where the contrast profile of the inner edge of the vessel wall may be too weak. An alternative approach is to fill the vessel lumen with FITC-labelled dextran and to determine the change in fluorescence emission, which reflects the mean cross-sectional area. Since cross-sectional area is proportional to the inner diameter, changes of the latter are easily derived from the recorded changes in cross-sectional area. This technique allows the determination of changes in inner diameter even in larger vessels which are not transparent enough for direct observation of the inner diameter (VanBavel et al. 1990). In experiments on cannulated vessel segments, pressure and flow should be established at values close to the in vivo conditions for the vessel under investigation. Such data have been published for a number of vessels and should be taken from the literature. For orientation in small arteries with a diameter in the range from 50–200 µm, transmural pressure is in the range 40–100 mmHg and flow is in the range 6–15 µl/min (to get a physiological level of shear stress with saline, i.e. without the cellular components of blood). The control of transmural pressure and flow in this situation is based on the following basic principles (see also Halpern 1991). First, a pressure difference is established between the cannula at the proximal end of the vessel (P1) and the cannula at the distal end of the vessel (P2). Since the flow through the cannulas and the vessel segment is associated with some friction, pressure gradients may develop along this system. Thus, in order to control the pressure in the vessel segment, flow resistance should be estimated. This is based on the Poiseuille law for flow Q = (P1-P2)πr4/8ηL where P1-P2 is the pressure difference, r is the radius, η is the viscosity of the fluid and L is the length of the segment. Strictly speaking this equation holds only if certain limitations are met, but cannulated vessel segments do not critically violate these limitations. Thus, the criterion for laminar flow is met using vessel segments with a length about 3–4 times longer than the lumen diameter (see also Duling et al. 1981). In addition, flow is given by Q = (P1-P2)/R 2.4 2 206 Isolated Organs where R is flow resistance. Hence R = (8ηL)/πr4 Taking for η a value of 6.92×10–3 poise (water at 37 °C – this is about one third of the value for whole blood, thus a three times larger flow as under physiological conditions will produce a physiological shear stress) In-Vitro Techniques R = 3.5×103 L/d4 mmHg/µl/min where the diameter (d) and the length (L) are expressed in µm. For example, a 450 µm long vessel segment with a lumen diameter of 150 µm has a R of 0.0031 mmHg/µl/ min. Thus, a flow of 10 µl/min produces a pressure drop of 0.031 mmHg between the ends of the vessel. Such calculations can easily be performed for any other vessel size. Flow may be measured by either weighing the effluent for a given interval of time (evaporation from these small volumes should be considered) or using a drop counter (uniform drop size should be obtained) or employing commercially available flow meters. In addition, flow can be estimated from the pressure difference (P1-P2) imposed when the flow resistances of the cannulas are much larger than that of the vessel, using Q = (P1-P2)/R. Under these conditions, the vessel flow resistance, which changes with altered diameter, can be neglected. However, in most situations, the flow resistance of the cannulas and of the vessel have similar values. Then, it is important to measure Q and P. A method of measuring the flow resistance of the cannulas is to insert them into a piece of polyethylene tubing of large diameter relative to the cannula and to measure perfusion pressure at various flows produced by a constant flow pump (for details see Halpern and Kelly 1991). Pressure should also be known, because it has effects on vessel diameter itself and therefore, should often be kept constant in order to understand the effect of flow. The pressure in the vessel segment can be measured directly by using a servo-micropressure null measurement. However, for this to be accomplished the vessel has to be punctured, which may introduce too much damage to the vessel wall and release of vasoactive substances. An indirect approach is to use cannulas with the same flow resistance. At steady flow the pressure in the vessel segment will be the mean of P1 and P2. However, it should be noted that pressure transducers used in these studies should be carefully calibrated. The investigation of cannulated vessel segments is often performed using a fixed transmural pressure. Because of the compliance of the tubing systems used to apply pressure, which accommodates the small volume changes during vessel diameter reactions, isobaric conditions are fulfilled during vessel reactions. Comparison of Both Mounting Methods A number of studies have shown that results obtained with the 2 mounting methods under the most commonly used conditions, i.e. ring vessel segments under isometric conditions and cannulated vessel segments under isobaric conditions, can be differ- Isolated Vessels 207 ent. Thus, the sensitivity of ring segments to noradrenaline was higher than that of cannulated segments (Buus et al. 1994; VanBavel and Mulvany 1994). In addition, the depolarisation induced by a maximum concentration of noradrenaline was 2.6-fold larger in ring segments compared to cannulated segments (Schubert et al. 1996). Since wall tension increases in ring segments, but decreases in cannulated segments, these findings have been explained by assuming that part of the vasoconstrictor-induced responses are wall tension dependent. Thus, a clear understanding of the differences between the mounting methods is required in order to able to select the most appropriate method for the specific hypothesis to be tested. Cannulated vessel segments are considered to be closer to in vivo conditions, because they (see also Halpern 1991): ▬ have a circular cross section. This is in sharp contrast to the two flat sheets of tissue when vessels are fixed on two hooks or wires. ▬ change their diameter in order to show alterations in the contractile state. This condition is also fulfilled in isotonic ring vessel segments, but not in the most often used isometric ring vessel segments. ▬ have an untouched endothelium. In contrast, the hooks and wires are in direct contact with the endothelium and may damage it during the mounting procedure in ring vessel preparations, especially in small vessels. ▬ are under the influence of a physiological stimulus, the transmural pressure, and develop spontaneous myogenic tone not usually seen with ring vessel preparations. ▬ are subjected to longitudinal elongation under pressurised conditions, which compensates for the retraction occurring during dissection. There is no elongation in ring vessel segments, which should be taken into account for morphological measurements. For example, in ring vessel segments larger wall-to-lumen ratios compared to cannulated vessel segments were observed. Thus, ring vessel segments are not a good estimate of in vivo wall-to-lumen ratio (for example see Lew and Angus 1992). ▬ allow agents to be superfused and/or perfused, enabling selective application from the luminal or the adventitial side of the vessel wall. Since receptors for vasoactive substances are often differentially expressed on endothelial and smooth muscle cells and the endothelium is a diffusion barrier for some, especially water-soluble substances applied from the vessel lumen, the route of application has to be taken into account. Indeed, different responses have been observed for phenylephrine and vasopressin, which were 10 to 100 time more potent when applied from the adventitial side (Lew and Angus 1992). Examples Ring Vessel Segments A typical example of an experiment performed using a ring vessel segment is shown in Fig. 2. Here, changes in wall tension with time are shown. After mounting of the vessel, the myograph was heated to 37 °C during the first 20 min (Fig. 2a). Thereafter, 2.4 208 Isolated Organs In-Vitro Techniques 2 Figure 2a,b Ring vessel segments. An experiment on a mouse aorta is presented showing the normalisation procedure and the viability test using serotonin (5-HT) at 10–5 M in a and the relaxation response to different concentrations of acetylcholine (Ach) and the contractile response to different concentrations of noradrenaline (NA) in b. For more details refer to the text the normalisation procedure as described in detail above is shown, which ends with establishing the optimal vessel diameter corresponding to 90% of the passive diameter of the vessel at 100 mmHg. Subsequently, the vessel was exposed twice to serotonin at a concentration of 10–5 M during the viability test. The response of the vessel to serotonin at the second application was larger than that at the first application, demonstrating the need for the viability test in order to get stable vessel responses. Then, an experiment was performed (Fig. 2b), showing a relaxation induced by the application of 4 different concentrations of acetylcholine after preconstriction of the vessel with serotonin and, after appropriate washout, a constriction induced by the application of 4 different concentrations of noradrenaline. Cannulated Vessel Segments A typical example of an experiment performed using a cannulated vessel segment is shown in Fig. 1. The inset shows a vessel cannulated by two pipettes and fixed there using strands of suture. In this example, changes in inner vessel diameter with time Isolated Vessels 209 are shown. After mounting of the vessel, the myograph was heated to 37 °C. During this period the vessel started to constrict, indicating the development of a spontaneous myogenic tone (Fig. 1a). Subsequently, the vessel was exposed to noradrenaline to test smooth muscle cell viability and, after washout, to acetylcholine in order to test endothelium viability. Then, an experiment was performed (Fig. 1b), showing the response of the vessel to consecutive pressure increases from 10 to 140 mmHg, i.e. the myogenic response, which is characterised by vessel dilations at lower pressure values and constrictions at pressures larger than 60 mmHg. Troubleshooting Solutions Solutions should be prepared carefully; in particular the occurrence of calcium precipitates should be avoided. This is especially important in experiments where calcium concentrations up to 10 mM are used, for example to study the dependence of a certain response on extracellular calcium. At such high calcium concentrations, precipitates of calcium and the phosphate anion may occur. If this happens, phosphate should be eliminated from the solution. Normalisation As shown in Fig. 2, lengthening of the vessel during a normalisation step leads to a fast increase in wall tension, followed by a decrease in wall tension consisting of a quick and a slow phase. However, sometimes a different picture is seen. If the increase and the following decrease in tension are considerably slowed down, the mechanical connection between the hooks or wires used to mount the vessel and the force transducer should be checked for the ability to move freely. This is especially important under isometric conditions, where these movements are very small but essential for the measurement. In some small arteries, especially from the cerebral and the coronary circulation, another phenomenon is sometimes observed. There, the phase of decreasing tension may be followed by a spontaneous increase in tension, indicating the development of spontaneous active tone. Since the normalisation procedure requires the determination of the passive tension of the vessel, the appearance of active tone should be avoided. In order to fulfill this requirement, either a dilating agonist should be added or a solution containing a low calcium concentration should be used. Viability test In some experiments on ring segments of small arteries the first application of an agonist during the viability test may produce a response considerably smaller than expected from previous experiments suggesting poor viability of the vessel preparation. Before replacing such a vessel, a second or third application of the agonist should 2.4 2 210 Isolated Organs be performed, where normal responses are often observed. In experiments on cannulated small arteries the development of a spontaneous myogenic tone is sometimes not observed, suggesting poor viability of the vessel preparation. Before replacing such a vessel, a contractile agonist at a submaximal concentration should be added. After washout of the agonist, a stable partial constriction often remains, indicating the induction of a spontaneous myogenic tone. However, the vessel should be replaced if upon washout vessel diameter returns to the fully relaxed state, even if this process is very slow. Since experiments will usually last several hours, a stable spontaneous myogenic tone is essential. In-Vitro Techniques Functional Antagonism Two problems arise from the so-called functional antagonism. The first is the selection of the preconstriction level in relaxation experiments using ring vessel segments. Since these vessel preparations usually do not develop spontaneous tone, relaxation responses can only be studied after preconstriction. However, the increase in tension produced by the vasoconstrictor used for preconstriction is imposing a functional antagonism to the effect of the relaxant agent. Thus, the use of increasing concentrations of the preconstricting agent resulted in a considerable decrease of the maximum response and in some cases also of the sensitivity to several relaxant agents (Stork and Cocks 1994). A systematic study employing different levels of preconstriction revealed that functional antagonism could only be avoided using a concentration of the preconstricting agent producing not more than 40% of maximum constriction (Stork and Cocks 1994). The second problem arises in experiments aimed at comparing responses to a certain vasoactive substance in the absence and presence of a pharmacological inhibitor, which has an effect on the preconstriction level or the spontaneous myogenic tone. The change of the initial tone may induce enough functional antagonism to produce an altered response, which however may not be related to the specific action of the inhibitor. In this situation, control experiments evaluating the role of changes of the initial tone are absolutely required. References Bevan JA, Osher JV (1972) A direct method for recording tension changes in the wall of small blood vessels in vitro. Agents Actions 2: 257–260 Boels PJ, Claes VA, Brutsaert DL (1990) Mechanics of K(+)-induced isotonic and isometric contractions in isolated canine coronary microarteries. Am.J Physiol 258: C512–C523 Boonen HC, DeMey JGR (1994) Distension influences responses to agonists and potassium in several types of small artery. In: Halpern W, Bevan J, Brayden JE, Dustan H, Nelson MT, Osol G (eds) The resistance arteries. Humana Press, Totowa, p 13–21 Bukoski RD, Shearin S, Jackson WF, Pamarthi MF (2001) Inhibition of Ca2+-induced relaxation by oxidized tungsten wires and paratungstate. J Pharmacol Exp Ther. 299: 343–350 Buus NH, VanBavel E, Mulvany MJ (1994) Differences in sensitivity of rat mesenteric small arteries to agonists when studied as ring preparations or as cannulated preparations. Br J Pharmacol 112: 579–587 Coats P, Hillier C (1999) Determination of an optimal axial-length tension for the study of isolated resistance arteries on a pressure myograph. Exp Physiol 84: 1085–1094 Duling BR, Gore RW, Dacey jr RG, Damon DN (1981) Methods for isolation, cannulation, and in vitro study of single microvessels. Am J Physiol 241: H108–H116 Isolated Vessels 211 Fischer JG, Mewes H, Hopp HH, Schubert R (1996) Analysis of pressurized resistance vessel diameter changes with a low cost digital image processing device. Comp Meth Prog Biomed 50: 23–30 Gonzalez MC, Arribas SM, Molero F, Fernandez-Alfonso MS (2001) Effect of removal of adventitia on vascular smooth muscle contraction and relaxation. Am J Physiol Heart Circ.Physiol 280: H2876–H2881 Halpern W (1991) Common in vitro investigative methods. In: Bevan J, Halpern W, Mulvany MJ (eds) The resistance vasculature. Humana Press, Totowa, pp 45–57 Halpern W, Kelley M (1991) In vitro methodology for resistance arteries. Blood Vessels 28: 245–251 Halpern W, Osol G, Coy GS (1984) Mechanical behavior of pressurized in vitro prearteriolar vessels determined with a video system. Ann Biomed Eng 12: 463–479 Hoogerwerf N, van der Linden PJ, Westerhof N, Sipkema P (1992) A new mounting technique for perfusion of isolated small arteries: the effects of flow and oxygen on diameter. Microvascular Research 44: 49–60 Lew MJ, Angus JA (1992) Wall thickness to lumen diameter ratios of arteries from SHR and WKY: comparison of pressurised and wire-mounted preparations. J Vasc Res 29: 435–442 Machkov VV, Vlasova MA, Tarasova OS, Mikhaleva LM, Koshelev VB, Timin EN, Rodionov IM (1998) Responses to noradrenaline of tail arteries in hypertensive, hypotensive and normotensive rats under different regimens of perfusion: role of the myogenic response. Acta Physiol Scand 163: 331–337 Monos E, Contney SJ, Dornyei G, Cowley AW, Stekiel WJ (1993) Hyperpolarization of in situ rat saphenous vein in response to axial stretch. Am J Physiol 265: H857–H861 Monos E, Raffai G, Contney SJ, Stekiel WJ, Cowley AW Jr. (2001) Axial stretching of extremity artery induces reversible hyperpolarization of smooth muscle cell membrane in vivo. Acta Physiol Hung 88: 197–206 Mulvany MJ, Halpern W (1976) Mechanical properties of vascular smooth muscle cells in situ. Nature 260: 617–619 Mulvany MJ, Halpern W (1977) Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats. Circ Res 41: 19–26 Mulvany MJ, Hansen OK, Aalkjaer C (1978) Direct evidence that the greater contractility of resistance vessels in spontaneously hypertensive rats is associated with a narrowed lumen, a thickened media, and an increased number of smooth muscle cell layers. Circ Res 43: 854–864 Nilsson H, Sjoblom N (1985) Distension-dependent changes in noradrenaline sensitivity in small arteries from the rat. Acta Physiol Scand 125: 429–435 Parkington HC, Tare M, Tonta MA, Coleman HA (1993) Stretch revealed three components in the hyperpolarization of guinea-pig coronary artery in response to acetylcholine. J Physiol 465: 459–476 Price JM, Davis DL, Knauss EB (1981) Length-dependent sensitivity in vascular smooth muscle. Am J Physiol 241: H557–H563 Schubert R, Wesselman JPM, Nilsson H, Mulvany MJ (1996) Noradrenaline-induced depolarization is smaller in isobaric compared to isometric preparations of rat mesenteric small arteries. Pflugers Arch Eur J Physiol 431: 794–796 Stork AP, Cocks TM (1994) Pharmacological reactivity of human epicardial coronary arteries: characterization of relaxation responses to endothelium-derived relaxing factor. Br J Pharmacol 113: 1099–1104 VanBavel E, Mooij T, Giezeman MJ, Spaan JA (1990) Cannulation and continuous cross-sectional area measurement of small blood vessels. J Pharmacol Methods 24: 219–227 VanBavel E, Mulvany MJ (1994) Role of wall tension in the vasoconstrictor response of cannulated rat mesenteric small arteries. J Physiol London 477: 103–115 Zaritsky JJ, Eckman DM, Wellman GC, Nelson MT, Schwarz TL (2000) Targeted disruption of Kir2.1 and Kir2.2 genes reveals the essential role of the inwardly rectifying K(+) current in K(+)-mediated vasodilation. Circ Res 87: 160–166 2.4